Back to Journals » Patient Preference and Adherence » Volume 9
Patient experiences with self-monitoring renal function after renal transplantation: results from a single-center prospective pilot study
Authors van Lint C, van der Boog P, Wang W, Brinkman W, Rövekamp T, Neerincx M, Rabelink T, van Dijk S
Received 9 July 2015
Accepted for publication 7 October 2015
Published 7 December 2015 Volume 2015:9 Pages 1721—1731
DOI https://doi.org/10.2147/PPA.S92108
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Céline L van Lint,1 Paul JM van der Boog,1 Wenxin Wang,2,3 Willem-Paul Brinkman,2 Ton JM Rövekamp,3 Mark A Neerincx,2 Ton J Rabelink,1 Sandra van Dijk1,4
1Department of Nephrology, Leiden University Medical Centre (LUMC), Leiden, 2Faculty of Electrical Engineering, Mathematics and Computer Science, Delft University of Technology, Delft, 3Department of Technology in Healthcare, Prevention and Health, Dutch Organization for Applied Scientific Research (TNO), Leiden, 4Department of Health, Medical and Neuropsychology, Faculty of Social and Behavioural Sciences, Leiden University, Leiden, the Netherlands
Background: After a kidney transplantation, patients have to visit the hospital often to monitor for early signs of graft rejection. Self-monitoring of creatinine in addition to blood pressure at home could alleviate the burden of frequent outpatient visits, but only if patients are willing to self-monitor and if they adhere to the self-monitoring measurement regimen. A prospective pilot study was conducted to assess patients’ experiences and satisfaction.
Materials and methods: For 3 months after transplantation, 30 patients registered self-measured creatinine and blood pressure values in an online record to which their physician had access to. Patients completed a questionnaire at baseline and follow-up to assess satisfaction, attitude, self-efficacy regarding self-monitoring, worries, and physician support. Adherence was studied by comparing the number of registered with the number of requested measurements.
Results: Patients were highly motivated to self-monitor kidney function, and reported high levels of general satisfaction. Level of satisfaction was positively related to perceived support from physicians (P<0.01), level of self-efficacy (P<0.01), and amount of trust in the accuracy of the creatinine meter (P<0.01). The use of both the creatinine and blood pressure meter was considered pleasant and useful, despite the level of trust in the accuracy of the creatinine device being relatively low. Trust in the accuracy of the creatinine device appeared to be related to level of variation in subsequent measurement results, with more variation being related to lower levels of trust. Protocol adherence was generally very high, although the range of adherence levels was large and increased over time.
Conclusion: Patients’ high levels of satisfaction suggest that at-home monitoring of creatinine and blood pressure after transplantation offers a promising strategy. Important prerequisites for safe implementation in transplant care seem to be support from physicians and patients’ confidence in both their own self-monitoring skills and the accuracy of the devices used.
Keywords: adherence, blood pressure, creatinine, kidney transplantation, satisfaction, self-monitoring
Background
Kidney transplantation is the treatment of choice for end-stage renal disease patients. It is associated with a reduced risk of mortality and cardiovascular events, as well as better quality of life than treatment with chronic dialysis.1 However, patients are at risk for acute rejection, predominantly in the first 6 months after transplantation.2 Most patients who develop acute rejection are asymptomatic, and present only with an increased serum creatinine. Consequently, frequent laboratory monitoring is essential in order to detect a creatinine increase as early as possible. Further, as hypertension is both a potential indicator of decreased kidney function and an important risk factor for kidney-transplant failure,3–6 blood pressure needs to be closely monitored too. Besides being burdensome to health care capacity, the high frequency of monitoring visits are a burden to patients: firstly, because many patients need to travel a considerable distance to get to the hospital; and secondly, because fear of rejection, the most common stressor among kidney-transplant patients,7–10 is more intense prior to clinical visits.10 The latter is conceivable, as the visits focus on discussing laboratory results that indicate how the patient’s graft is functioning.
Being able to monitor creatinine and blood pressure at home could alleviate the burden of frequent outpatient visits and high levels of stress prior to consultations. With the development of a handheld point-of-care creatinine device, patients are now able to self-monitor creatinine. In contrast to self-monitoring creatinine, patients self-monitoring blood pressure is more common practice, and the clinical benefits of home-based blood pressure measurements in kidney-transplant patients have already been shown.11,12
However, experiences and satisfaction with self-monitoring of transplanted patients have never been taken into account. Research in other chronic disease populations shows that self-monitoring is generally highly valued by patients.13–17 However, this does not pertain to every patient. A factor that seems to influence patient motivation for and satisfaction with self-monitoring is level of trust. Patients have to trust the accuracy and reliability of the monitoring device(s)18,19 and their own self-monitoring skills,20,21 and they have to experience support and trust from their clinician as well.22,23 Further, previous studies showed that self-monitoring increased patients’ feelings of security, reassurance, and control over their own medical condition,13,14,16,24,25 suggesting that worrisome patients have more to gain from self-monitoring than those worrying less. On the contrary, self-monitoring bodily symptoms can also rouse intrusive feelings of fear and doubt, especially when frequent self-monitoring picks up even small fluctuations.13,26
To the best of our knowledge, there is a lack of data about the attitude of kidney-transplant patients toward self-monitoring. This poses a problem, as the feasibility of self-monitoring is highly dependent on the willingness and ability of patients to monitor at home.19,27 The aim of the current study was as follows: firstly, to study kidney-transplant patients’ willingness to self-monitor after kidney transplantation and their experiences with self-monitoring; secondly, to assess how worries and trust regarding devices, personal skills, and the doctor–patient interaction are related to experienced level of satisfaction; and thirdly, to study patients’ adherence to the measurement protocol, as good adherence to the protocol is a prerequisite for safety from a clinical point of view.
Materials and methods
This prospective pilot study was performed at the Leiden University Medical Centre in advance of a randomized control trial on the applicability of self-monitoring after kidney transplantation. The study protocol was reviewed and approved by the Medical Ethics Committee. Patients were recruited from June 2010 to January 2011, at 2–4 weeks prior to a living donor transplantation. Inclusion criteria were being ≥18 years of age, mastery of the Dutch language, and having access to the Internet. All participants provided written informed consent.
All patients received transplant care as usual. Immunosuppressive regimens comprised of basiliximab for induction (except for one patient receiving alemtuzumab) and glucocorticoids, tacrolimus, and mycophenolate mofetil for maintenance therapy. To optimize levels of the immunosuppressive agents, regular monitoring of trough levels was combined with monitoring systemic exposure (as measured by areas under the curve) at 6 weeks and 6 months posttransplantation and yearly afterward.
In addition to regular outpatient care, participants monitored levels of whole-blood creatinine and blood pressure at home during the first 12 weeks after kidney transplantation. They received a plan starting from the day after discharge. Measurement frequency was decreased stepwise, ranging from daily in the first weeks to once a week in weeks 9–12. Patients registered their measurement results in an online disease-management system (DMS) to which their physician also had access.
Patients completed a questionnaire at discharge from hospital after kidney transplantation (ie, baseline) and at the end of the study period after 12 weeks (ie, follow-up). Baseline questionnaires and return envelopes were supplied 1 day in advance of discharge from the hospital. Follow-up questionnaires were sent out after completion of the study period, ie, after 12 weeks.
The first ten patients who finished participation were interviewed about their experiences. A semistructured protocol was applied with open-ended questions that reflected topics from the questionnaire (Table S1). Interviews were recorded and transcribed in full. As interview data were only used to facilitate interpretation of quantitative results, no further formal coding and analysis was conducted.
Self-monitoring procedure
Prior to or immediately following transplantation, patients received instructions about how to perform, interpret, and record the creatinine and blood pressure measures. For self-monitoring creatinine, each participant received a StatSensor® Xpress™ creatinine hospital meter (Nova Biomedical, Waltham, USA; certified according to International Organization for Standardization 13485:2003, In Vitro Diagnostics Directive, meets International Electrotechnical Commission 61010, Underwriters Laboratories, and US Food and Drug Administration labeled for in vitro diagnostic use) and measurement accessories (ie, test strips, control solution to test the quality of the strips, and safety lancets for capillary blood sampling). Although the devices’ accuracy for detecting current kidney function with a single creatinine measurement is debated,28–31 they seem suitable for monitoring creatinine trends with serial creatinine measurements in kidney-transplant patients.31 It is important to distinguish between these applications, as this determines the analytical performance requirements of the devices.32 For trend monitoring, the accuracy of a single creatinine-test result is less critical, as test results are used to detect changes between sequential measurements. Patients received specific instructions about how to interpret sequential results, rather than single measurements. Further, values registered in the online DMS were depicted in a graph to support trend-wise interpretation of test results.
For self-monitoring blood pressure, each participant received a Microlife WatchBP® Home (Microlife AG, Widnau, Switzerland), an oscillometric device for blood pressure self-measurement on the upper arm. The Microlife WatchBP Home fulfills the validation requirements for self-monitoring blood pressure at home.33
Questionnaires
Both validated questionnaires and questionnaires designed specifically for the study were used. We measured level of general and more specific satisfaction, experience with self-monitoring, amount of transplant-related worries (Worry Scale, Transplant Effects Questionnaire),34 trust in own monitoring skills (self-efficacy), and patients’ perceptions of the level of autonomy support from their physician (Health Care Climate Questionnaire).35 Item examples, answering scales, and time of application are listed in Table 1.
  | Table 1 Characteristics of the questionnaires |
Demographics that could not easily be extracted from the hospital system (marital status, nationality, educational level, and Internet use) were self-reported at baseline. Education level was based on the highest level of education accomplished, and categorized into three categories according to the International Standard Classification of Education (ie, low, middle, and high level).36
Clinical data
Creatinine and blood pressure values that were recorded by the patients were exported from the DMS database. The number of registered measurements was counted per 3-week study period (weeks 1–3, weeks 4–6, etc). Laboratory creatinine and eGFR (estimated glomerular filtration rate, according to the Modification of Diet in Renal Disease study) were exported from the hospital system. Average eGFR was calculated per 3-week study period for each individual patient.
Statistical analyses
Descriptive statistics were calculated for patients’ creatinine, kidney function, blood pressure (mean arterial pressure [MAP]), and antihypertensive treatment, as well as for level of general satisfaction, experience with using the devices, self-monitoring skills, and experienced autonomy support. When applicable, scores on the 5-point Likert scales were grouped into three categories to describe patients’ views: don’t agree (score ≤2), agree (score ≥4), or neutral (score 3). Student’s t-test was used to assess whether patients’ self-monitoring experiences differed between the creatinine and blood pressure device. Paired-sample t-tests were used to compare baseline and follow-up scores regarding satisfaction and self-monitoring skills. To investigate whether specific patient characteristics were related to experiences and attitudes, Pearson’s correlations were computed with a preset subset of patient characteristics that was derived from the literature, being age, sex, level of trust in accuracy of the devices (creatinine and blood pressure), support from the physician to be autonomous, self-efficacy regarding self-monitoring, and transplant-related worries.
Adherence to measurement frequency according to protocol was calculated by dividing the number of online registered measurements per week by the number of requested measurements per week. This procedure has been used before to calculate adherence to self-monitoring blood glucose.37 All statistical analyses were performed with SPSS version 20.0. P-values of <0.05 were considered significant.
Results
Study population
During the period of inclusion, 42 patients received a kidney from a living donor. Of the 34 eligible patients, 32 gave informed consent. Two patients dropped out because of serious medical complications following surgery. Thirty patients received the self-monitoring equipment and started performing self-measurements after a mean of 8 (standard deviation [SD] 3) days after transplantation. One patient was lost to follow-up (Figure S1 for the study flowchart). Characteristics of the study population are shown in Table 2. The majority of patients were female, married or living together, and of Dutch origin. Just over half were transplanted prior to initiation of dialysis (preemptive).
The baseline questionnaire was completed by 30 (100%) and the follow-up measure by 25 (83%) patients. Although the number of patients who did not complete the follow-up questionnaire was too low to conduct formal analyses, nonresponders to the follow-up questionnaire seemed to perceive more disadvantages of performing and interpreting self-measurements at baseline than responders. The ten patients that were interviewed seemed representative of the total study population (ie, no differences were observed regarding sociodemographics, Internet experience, satisfaction, or opinions about self-monitoring [data not shown]). Patient quotes that reflect questionnaire results are given in Table 3.
  | Table 3 Patient quotes from the interviews (n=10) |
Clinical data
Mean levels of creatinine and mean eGFR measured at baseline were 132 (SD 35) and 51 (SD 19), respectively. Mean levels of creatinine and mean eGFR at follow-up were 134 (SD 37) and 49 (SD 11), respectively. MAP was 101 (SD 7) at baseline and improved over time (Table 2). Twenty-one of 30 patients (70%) were prescribed antihypertensive treatment at discharge after transplantation. For one patient, baseline antihypertensive treatment could not be traced. The remaining patients (n=8) did not use any antihypertensive medication at baseline. The mean number of antihypertensive prescriptions was 1.28 per patient (ranging from 0 to 3).
During the period of inclusion, three patients experienced an episode of acute rejection (at 26, 84, and 90 days posttransplantation, respectively). For two of these patients, a steep increase in blood-level creatinine was visible in the self-measured creatinine values preceding hospital admittance for rejection treatment. The third patient did not self-monitor creatinine in the week preceding diagnosis of acute rejection. It therefore remains unclear whether this specific rejection could have been detected at home.
Patients’ experiences with using the measurement devices
The majority of patients considered using the creatinine and blood pressure devices to be pleasant (95% and 100%, respectively), useful (91% and 100%, respectively), and reassuring (63% and 76%, respectively). Trust in accuracy of the creatinine meter was significantly lower than trust in accuracy of the blood pressure meter (P<0.001) (Figure 1). Based on the remarks patients made during the interviews (Table 3, quote 1), we hypothesized that levels of unexplained variation in successive creatinine measurements might have resulted in lower levels of trust in the accuracy of the creatinine meter. To verify this, we calculated variation in creatinine measurements designated as the mean percentage change from successive measurements (ie, difference between two measurements divided by their average). Analysis showed that a higher level of mean variation was indeed related to a lower level of trust in the creatinine device (P=0.03). However, no associations were found between the amount of mean variation in creatinine results and whether using the creatinine meter was considered pleasant, reassuring, or useful (P=0.78, 0.71, and 0.57, respectively). The same analyses were conducted with regard to variations in successive measurements of MAP. Mean variation in MAP was neither related to trust in accuracy of the blood pressure meter (P=0.86), nor to whether use of the blood pressure meter was considered pleasant, reassuring, or useful (P=0.88, 0.43, and 0.99, respectively).
Psychological measures: self-efficacy, perceived autonomy support, and worries
Patients reported a high amount of trust in their own monitoring skills at baseline (mean 4.37, SD 0.49) already, and this did not change over time (follow-up mean 4.31, SD 0.78; P=0.69). In line with this, interview data suggested that self-monitoring was perceived as very easy, with half of the patients (n=5) spontaneously mentioning the simplicity of the required actions, while none reported any difficulties (Table 3, quote 2).
Although patients were generally satisfied with the level of autonomy support they received, (mean 3.87, SD 0.70), half of the interviewed patients (n=5) stated that their physicians had only limited interest in patients’ self-measured creatinine data. Despite the seemingly limited attention some physicians paid to the creatinine values measured at home, patients considered self-monitoring creatinine to be beneficial anyway (Table 3, quote 3).
Physicians did however pay attention to patients’ self-measured blood pressure results (Table 3, quote 4). In line with this, analysis of hospital records revealed that for 80% of our patients, home-based blood pressure measurements were registered in the hospital system. On average, patients seemed to be somewhat worried about their transplantation, but these worries declined over time (baseline mean 2.98, SD 0.88, follow-up mean 2.38, SD 0.82; P=0.01).
Patients’ satisfaction
Patients reported high levels of satisfaction with the self-monitoring facilities of the DMS (baseline mean 7.25, SD 1.23), which significantly increased over time (follow-up mean 7.78, SD 1.19; P=0.01). A high level of satisfaction at follow-up was related to higher levels of trust in the accuracy of the creatinine meter (P<0.01), perceived autonomy supportiveness of physicians (P<0.01), and efficacy concerning self-monitoring skills (P<0.01).
The most important perceived advantage of self-monitoring at follow-up was the receipt of an automatic warning when creatinine level was increased (Tables 3 and 4, quote 5). In general, patients tended to agree with the list of suggested advantages, whereas they tended to disagree with the list of suggested disadvantages (Table 4). Slight changes were observed in the ratings of advantages and disadvantages over time (Table 4). For example, the advantage that physicians had access to the values measured at home was rated as less advantageous at follow-up than at baseline (P=0.01).
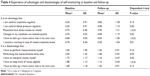  | Table 4 Experience of advantages and disadvantages of self-monitoring at baseline and follow-up |
Patients’ adherence to measurement protocol
Level of adherence to the measurement protocol is depicted in Figure 2. As the number of registered creatinine and blood pressure values was similar within patients, adherence rates pertain to both creatinine and blood pressure measurements. Mean adherence was consistently close to or >100% (ie, more measurements than requested were registered). However, there were large differences between patients that increased over time. Adherence ranged from 0 to 367% during the follow-up period in weeks 10–12, with four patients recording <80% and 14 patients recording >120% of the required measurements. None of the patient characteristics was related to measurement adherence. We hypothesized that either patients’ kidney function (ie, eGFR according to the Modification of Diet in Renal Disease formula using laboratory serum creatinine) or the amount of variation in successive measurements might be related to how frequently patients measured their creatinine and blood pressure. Additional analyses showed that kidney function was not related to measurement frequency (P=0.33). However, between measurement frequency and mean variation in successive measurements, a trend was observed (P=0.08), suggesting a higher amount of variation to be related to lower measurement frequency and vice versa.
  | Figure 2 Percentage adherence to measurement frequency per protocol. |
Discussion
Patient self-monitoring after kidney transplantation could possibly alleviate the burden of frequent outpatient visits and high levels of stress prior to consultations. The feasibility of self-monitoring, however, is highly dependent on the willingness and ability of kidney-transplant patients to monitor at home. The current results showed that patients were highly motivated to self-monitor kidney function and reported high levels of general satisfaction. The use of both the creatinine and blood pressure meters was considered pleasant and useful, despite levels of trust in the accuracy of the creatinine device being relatively low. Trust in the accuracy of the creatinine device appeared to be related to level of variation in subsequent measurement results, with more variation accompanying lower levels of trust. Average adherence to the monitoring protocol was good, but large individual differences between patients were found that increased over time.
Our results indicate that self-monitoring may be highly attractive to transplanted patients. Especially in the first 6 months after transplantation, when a relatively high risk of rejection2 necessitates highly frequent monitoring, self-monitoring may provide both additional reassurance to patients about how their graft is functioning and a potential measure to diminish the number of outpatient appointments. The experience of an extra sense of security, reassurance, and control has been reported in other self-monitoring studies.14–17 Our high response rate (32 of 34 willing to participate) further suggests that self-monitoring is not just an attractive option for a small selection of patients, which has been observed in other chronic disease populations,27,38–40 but may also be appealing to the majority of recipients of a living donor kidney.
However, for successful implementation of self-monitoring into posttransplantation care, some barriers should be considered. Several factors were related to patients’ satisfaction with self-monitoring. Firstly, although patients’ relatively low levels of trust in the accuracy of the creatinine meter did not seem to discourage them from measuring, patients were more satisfied if they perceived the self-monitoring devices as being reliable. This corresponds with existing literature, showing that patients’ confidence in the accuracy and perceived reliability of devices is an important prerequisite to the acceptance of these devices.18,19 Although patients received instructions for trend monitoring, their unfamiliarity with interpreting successive rather than single measurement values may have hampered their trust in the creatinine device. Indeed, trend monitoring may be more demanding than interpreting a single measurement value, as trend monitoring requires a careful consideration of the combination of several measurements.
Secondly, satisfaction about self-monitoring was related to patients’ perceived support from their physicians to be autonomous. This is in line with self-determination theory,41 which emphasizes the need of autonomy-supportive social contexts. It also emphasizes that patients do consider self-monitoring as a care system in which their physicians keep playing an important role. Indeed, several studies show that patients consider self-monitoring a less attractive option if this automatically implies a loss of human interaction with the clinical staff.19,42
Although patients were satisfied with the general amount of autonomy support from their physicians, interview data revealed that several physicians paid little attention to the self-measured creatinine data. Previous studies have also shown that physicians may be somewhat hesitant toward patient self-monitoring.43,44 It has been suggested that physicians consider it difficult to determine whether patients are capable of self-monitoring and interpreting the measurements,45,46 are afraid that self-monitoring will lead to a loss of control over therapy, and think that allowing patients to self-monitor will be more time-consuming.45,47,48 However, in the current study physicians did pay attention to self-measured blood pressures. The difference in attention for creatinine and blood pressure measurements might have been due to a relatively low level of trust in the accuracy of the creatinine device. Although they were also informed on the suitability of the device for monitoring creatinine trends, physicians expressed doubts about the accuracy of the meter, due to a variation in successive measurements. The greater familiarity with home-based blood pressure monitoring might have also played a role. The positive effects of self-monitoring blood pressure on therapy outcomes have been clearly demonstrated,27,49 whereas for self-monitoring creatinine this has yet to be established.
Thirdly, patients were more satisfied if they had a high self-efficacy regarding their own monitoring skills. The importance of self-efficacy for experienced satisfaction has been shown before,20,21 suggesting that thoroughly instructing and supporting patients are important prerequisites for successful and satisfactory self-monitoring. Our data did not support the suggestion that self-monitoring bodily symptoms could cause (unnecessary) worry and doubts,13,26 or would be more or less beneficial for worried patients.
Finally, to enhance safe implementation of self-monitoring in which self-measured values are an important source of information, patients should adhere to the self-monitoring protocol. Nonadherence to the protocol may leave serious complications unnoticed, which could ultimately lead to permanent loss of kidney function. Protocol adherence in the current study was generally good, with the majority of patients measuring more often than requested. Considering that fear of rejection is common in patients after a (recent) transplantation,7–10 it is tempting to assume that conducting extra measurements indicates a high need for reassurance. In the current study, however, no relation was found between measurement frequency and level of transplant-related worries. Besides patients performing more measurements than required, some patients did not adhere to the protocol, and their number increased over time. The current data set did not offer a clear-cut explanation for this finding, although a trend for a negative relation between measurement frequency and amount of variation in subsequent creatinine-test results was observed. This suggests the existence of a relation between higher amount of variation and lower measurement frequency and vice versa.
In addition to the suggested role of level of variation, two features of this study could have contributed to a lower level of adherence over time. First, the limited attention some physicians paid to measurement results might have reduced the perceived need to perform the measurements. Second, as self-monitoring creatinine and blood pressure was an add-on service to regular outpatient care, patients were not dependent upon their own measurements for information on their kidney function. This could have diminished patients’ perceived need to self-monitor. Adherence might thus improve when monitoring at home has a more prominent role in posttransplantation care instead of being just an add-on service. Nevertheless, protocol nonadherence remains a serious issue to consider in future studies to ensure safety of self-monitoring.
Conclusion
To the best of our knowledge, this is the first study to investigate the possibility of self-monitoring kidney function after kidney transplantation and the first study on kidney-transplant patients’ attitude toward self-monitoring. The results show that self-monitoring creatinine and blood pressure after kidney transplantation was well received by kidney-transplant patients. However, the relatively small number of participants and the selection of recipients of living donor kidneys prevents us from drawing strong conclusions that can be generalized to the entire kidney-transplant population. Further, as nonresponders to the follow-up questionnaire seemed to be somewhat less positive about self-monitoring at baseline, the absence of their follow-up experiences could have introduced a small bias toward a positive evaluation.
Overall, our results suggest that a self-monitoring care system has the potential to improve posttransplantation care in several ways: firstly, by increasing patient satisfaction;14,17,24,27,37,38,50–52 secondly, by decreasing the high number of outpatient visits, as important parameters can be monitored at home; and finally, by advancing the detection of acute rejection and hypertension due to higher frequency of monitoring, which may improve kidney-graft survival.5,53–58 Future studies should determine whether it is feasible and safe to implement patient monitoring of kidney function and blood pressure into transplantation care.
Acknowledgment
This work was supported by a grant from the Dutch Kidney Foundation.
Disclosure
The authors report no conflicts of interest in this work.
References
Tonelli M, Wiebe N, Knoll G, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11:2093–2109. | ||
Chon WJ, Brennan DC. Clinical manifestations and diagnosis of acute renal allograft rejection. 2013. Available from: http://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-acute-renal-allograft-rejection. Accessed October 13, 2015. | ||
Fernández-Fresnedo G, Palomar R, Escallada R, et al. Hypertension and long-term renal allograft survival: effect of early glomerular filtration rate. Nephrol Dial Transplant. 2001;16 Suppl 1:105–109. | ||
Hillebrand U, Suwelack BM, Loley K, et al. Blood pressure, antihypertensive treatment, and graft survival in kidney transplant patients. Transpl Int. 2009;22:1073–1080. | ||
Mange KC, Cizman B, Joffe M, Feldman HI. Arterial hypertension and renal allograft survival. JAMA. 2000;283:633–638. | ||
Opelz G, Döhler B. Improved long-term outcomes after renal transplantation associated with blood pressure control. Am J Transplant. 2005; 5:2725–2731. | ||
Baines LS, Joseph JT, Jindal RM. Emotional issues after kidney transplantation: a prospective psychotherapeutic study. Clin Transplant. 2002;16:455–460. | ||
Griva K, Ziegelmann JP, Thompson D, et al. Quality of life and emotional responses in cadaver and living related renal transplant recipients. Nephrol Dial Transplant. 2002;17:2204–2211. | ||
Kong IL, Molassiotis A. Quality of life, coping and concerns in Chinese patients after renal transplantation. Int J Nurs Stud. 1999;36:313–322. | ||
Fallon M, Gould D, Wainwright SP. Stress and quality of life in the renal transplant patient: a preliminary investigation. J Adv Nurs. 1997;25:562–570. | ||
Agena F, Prado ES, Souza PS, et al. Home blood pressure (BP) monitoring in kidney transplant recipients is more adequate to monitor BP than office BP. Nephrol Dial Transplant. 2011;26:3745–3749. | ||
Sberro-Soussan R, Rabant M, Snanoudj R, et al. Home and office blood pressure monitoring in renal transplant recipients. J Transplant. 2012;2012:702316. | ||
Barnard KD, Young AJ, Waugh NR. Self monitoring of blood glucose – a survey of diabetes UK members with type 2 diabetes who use SMBG. BMC Res Notes. 2010;3:318. | ||
Cromheecke ME, Levi M, Colly LP, et al. Oral anticoagulation self-management and management by a specialist anticoagulation clinic: a randomised cross-over comparison. Lancet. 2000;356:97–102. | ||
Gadisseur AP, Breukink-Engbers WG, van der Meer FJ, van den Besselaar AM, Sturk A, Rosendaal FR. Comparison of the quality of oral anticoagulant therapy through patient self-management and management by specialized anticoagulation clinics in the Netherlands: a randomized clinical trial. Arch Intern Med. 2003;163:2639–2646. | ||
Jones MI, Greenfield SM, Bray EP, et al. Patients’ experiences of self-monitoring blood pressure and self-titration of medication: the TASMINH2 trial qualitative study. Br J Gen Pract. 2012;62:e135–e142. | ||
Sawicki PT. A structured teaching and self-management program for patients receiving oral anticoagulation: a randomized controlled trial. Working Group for the Study of Patient Self-Management of Oral Anticoagulation. JAMA. 1999;281:145–150. | ||
Shah SG, Robinson I. Patients’ perspectives on self-testing of oral anticoagulation therapy: content analysis of patients’ Internet blogs. BMC Health Serv Res. 2011;11:25. | ||
Shah SG, Barnett J, Kuljis J, Hone K, Kaczmarski R. Factors determining patients’ intentions to use point-of-care testing medical devices for self-monitoring: the case of international normalized ratio self-testing. Patient Prefer Adherence. 2013;7:1–14. | ||
Biderman A, Noff E, Harris SB, Friedman N, Levy A. Treatment satisfaction of diabetic patients: what are the contributing factors? Fam Pract. 2009;26:102–108. | ||
Markson LE, Vollmer WM, Fitterman L, et al. Insight into patient dissatisfaction with asthma treatment. Arch Intern Med. 2001;161:379–384. | ||
Oliveira VC, Refshauge KM, Ferreira ML, et al. Communication that values patient autonomy is associated with satisfaction with care: a systematic review. J Physiother. 2012;58:215–229. | ||
Jaana M, Paré G, Sicotte C. Home telemonitoring for respiratory conditions: a systematic review. Am J Manag Care. 2009;15:313–320. | ||
Sawicki PT, Gläser B, Kleespies C, et al. Self-management of oral anticoagulation: long-term results. J Intern Med. 2003;254:515–516. | ||
Michie S, McCaffery K, Heneghan C. Monitoring as a learning and motivational tool. In: Glasziou PP, Irwig L, Aronson JK, editors. Evidence-Based Medical Monitoring: From Principles to Practice. London: BMJ Books; 2008;123–139. | ||
McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet. 2010;376:163–172. | ||
Korpi-Steiner NL, Williamson EE, Karon BS. Comparison of three whole blood creatinine methods for estimation of glomerular filtration rate before radiographic contrast administration. Am J Clin Pathol. 2009;132:920–926. | ||
Shephard M, Peake M, Corso O, et al. Assessment of the Nova StatSensor whole blood point-of-care creatinine analyzer for the measurement of kidney function in screening for chronic kidney disease. Clin Chem Lab Med. 2010;48:1113–1119. | ||
Straseski JA, Lyon ME, Clarke W, Dubois JA, Phelan LA, Lyon AW. Investigating interferences of a whole-blood point-of-care creatinine analyzer: comparison to plasma enzymatic and definitive creatinine methods in an acute-care setting. Clin Chem. 2011;57:1566–1573. | ||
van Lint CL, van der Boog PJ, Romijn FP, et al. Application of a point of care creatinine device for trend monitoring in kidney transplant patients: fit for purpose? Clin Chem Lab Med. 2015;53:1547–1556. | ||
Horvath AR, Lord SJ, St John A, et al. From biomarkers to medical tests: the changing landscape of test evaluation. Clin Chim Acta. 2014;427:49–57. | ||
Stergiou GS, Giovas PP, Gkinos CP, Patouras JD. Validation of the Microlife WatchBP Home device for self home blood pressure measurement according to the International Protocol. Blood Press Monit. 2007;12:185–188. | ||
Ziegelmann JP, Griva K, Hankins M, et al. The Transplant Effects Questionnaire (TxEQ): the development of a questionnaire for assessing the multidimensional outcome of organ transplantation – example of end stage renal disease (ESRD). Br J Health Psychol. 2002;7:393–408. | ||
Williams GC, Grow VM, Freedman ZR, Ryan RM, Deci EL. Motivational predictors of weight loss and weight-loss maintenance. J Pers Soc Psychol. 1996;70:115–126. | ||
United Nations Educational, Scientific and Cultural Organization Institute for Statistics (UIS). International Standard Classification of Education: ISCED 2011. Montreal: UIS; 2012. | ||
Vincze G, Barner JC, Lopez D. Factors associated with adherence to self-monitoring of blood glucose among persons with diabetes. Diabetes Educ. 2004;30:112–125. | ||
Bloomfield HE, Krause A, Greer N, et al. Meta-analysis: effect of patient self-testing and self-management of long-term anticoagulation on major clinical outcomes. Ann Intern Med. 2011;154:472–482. | ||
Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299:2857–2867. | ||
van der Meer V, Bakker MJ, van den Hout WB, et al. Internet-based self-management plus education compared with usual care in asthma: a randomized trial. Ann Intern Med. 2009;151:110–120. | ||
Deci EL, Ryan RM. Self-determination theory. In: Van Lange PA, Kruglanski AW, Higgins ET, editors. Handbook of Theories of Social Psychology. Vol 1. London: Sage; 2012;416–437. | ||
Khan TI, Kamali F, Kesteven P, Avery P, Wynne H. The value of education and self-monitoring in the management of warfarin therapy in older patients with unstable control of anticoagulation. Br J Haematol. 2004;126:557–564. | ||
Peel E, Douglas M, Lawton J. Self monitoring of blood glucose in type 2 diabetes: longitudinal qualitative study of patients’ perspectives. BMJ. 2007;335:493. | ||
Vasileiou K, Barnett J, Young T. Interpreting and acting upon home blood pressure readings: a qualitative study. BMC Fam Pract. 2013; 14:97. | ||
Sharma U, Barnett J, Clarke M. Clinical users’ perspective on telemonitoring of patients with long term conditions: understood through concepts of Giddens’s structuration theory and consequence of modernity. Stud Health Technol Inform. 2010;160:545–549. | ||
Thorne SE, Ternulf NK, Paterson BL. Attitudes toward patient expertise in chronic illness. Int J Nurs Stud. 2000;37:303–311. | ||
Sunaert P, Vandekerckhove M, Bastiaens H, et al. Why do GPs hesitate to refer diabetes patients to a self-management education program: a qualitative study. BMC Fam Pract. 2011;12:94. | ||
Blakeman T, Macdonald W, Bower P, Gately C, Chew-Graham C. A qualitative study of GPs’ attitudes to self-management of chronic disease. Br J Gen Pract. 2006;56:407–414. | ||
Bray EP, Holder R, Mant J, McManus RJ. Does self-monitoring reduce blood pressure? Meta-analysis with meta-regression of randomized controlled trials. Ann Med. 2010;42:371–386. | ||
Gadisseur AP, Kaptein AA, Breukink-Engbers WG, van der Meer FJ, Rosendaal FR. Patient self-management of oral anticoagulant care vs management by specialized anticoagulation clinics: positive effects on quality of life. J Thromb Haemost. 2004;2:584–591. | ||
Ryan F, Byrne S, O’Shea S. Randomized controlled trial of supervised patient self-testing of warfarin therapy using an Internet-based expert system. J Thromb Haemost. 2009;7:1284–1290. | ||
Van Gaalen JL, Hashimoto S, Sont JK. Telemanagement in asthma: an innovative and effective approach. Curr Opin Allergy Clin Immunol. 2012;12:235–240. | ||
Bellos JK, Perrea DN, Vlachakos D, Kostakis AI. Chronic allograft nephropathy: the major problem in long-term survival: review of etiology and interpretation. Transplant Rev. 2005;19:138–144. | ||
Griva K, Stygall J, Ng JH, Davenport A, Harrison MJ, Newman S. Prospective changes in health-related quality of life and emotional outcomes in kidney transplantation over 6 years. J Transplant. 2011;2011:671571. | ||
Joosten SA, Sijpkens YW, van KC, Paul LC. Chronic renal allograft rejection: pathophysiologic considerations. Kidney Int. 2005;68:1–13. | ||
Kaden J, May G, Völp A, Wesslau C. Factors impacting short and long-term kidney graft survival: modification by single intra-operative high-dose induction with ATG-Fresenius. Ann Transplant. 2011;16:81–91. | ||
Kasiske BL, Anjum S, Shah R, et al. Hypertension after kidney transplantation. Am J Kidney Dis. 2004;43:1071–1081. | ||
McDonald S, Russ G, Campbell S, Chadban S. Kidney transplant rejection in Australia and New Zealand: relationships between rejection and graft outcome. Am J Transplant. 2007;7:1201–1208. | ||
Opelz G, Döhler B. Influence of time of rejection on long-term graft survival in renal transplantation. Transplantation. 2008;85:661–666. |
Supplementary materials
  | Table S1 Interview protocol |
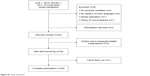  | Figure S1 Study flowchart. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.