Back to Journals » Patient Preference and Adherence » Volume 11
Patient adherence to subcutaneous IFN beta-1a injections using the RebiSmart® injection device: a retrospective real-world study among Dutch and German patients with multiple sclerosis
Authors Krol M, de Voer G, Osowski U
Received 23 December 2016
Accepted for publication 14 April 2017
Published 11 July 2017 Volume 2017:11 Pages 1189—1196
DOI https://doi.org/10.2147/PPA.S130985
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Marieke Krol,1 Gert de Voer,2 Ulrike Osowski3
1QuintilesIMS, Capelle aan den Ijssel, the Netherlands; 2Merck B.V., Schiphol-Rijk, the Netherlands; 3Merck KGaA, Darmstadt, Germany
Purpose: Long-term treatment adherence among patients with multiple sclerosis (MS) is a general concern, with an established correlation with clinical efficacy. Closely monitoring patients’ treatment behavior may have a beneficial effect on adherence. This study assessed adherence, in daily life, to subcutaneous (sc) IFN beta-1a, self-administered using the RebiSmart® electronic injection device (the IFN beta-Ia autoinjector device), in patients with MS.
Patients and methods: This was a retrospective observational study analyzing treatment adherence based on injection data, eg, injection date and dose, extracted from the IFN beta-Ia autoinjector devices collected from patients in Germany and the Netherlands.
Results: Data recorded in the period from 2007 to 2012 by the IFN beta-Ia autoinjector devices from 1,682 (79.7% from Germany, 20.3% from the Netherlands) patients were analyzed. A mean of 94.8% of the multi-dose cartridges (containing sc IFN beta-1a for three injections) were used completely, indicating a low incidence of application errors and drug wastage. The mean adherence rate was 90.7% and 82.9% over the entire observation period (mean treatment duration: 150.1 weeks). Median adherence rates were similar between German and Dutch patients (97.9% vs 99.0%).
Conclusion: In daily clinical practice, patients using the IFN beta-Ia autoinjector device were highly adherent to sc IFN beta-1a. The injection data stored electronically in the device may help patients to adhere to treatment regimens and, if viewed by physicians, promote discussion of adherence issues with patients.
Keywords: multiple sclerosis, injection device, IFN beta-1a, observational study
Introduction
Multiple sclerosis (MS) is a disease in which the myelin sheath around the nerves of the central nervous system is attacked by the immune system. These inflammations cause damage to eg, myelin, axons, oligodendrocytes, and subsequent neurodegeneration. In brain tissue of MS patients, macroscopic and microscopic lesions can be observed throughout the central nervous system. Based on the course of the disease, which varies individually, different MS subtypes are recognized. The relapsing-remitting subtype is the most common form.1 Prevalence estimates of MS range between 62 and 128 per 100,000 persons in Central Europe.2
Patients with relapsing-remitting MS were originally treated with injectable disease-modifying drugs (DMDs), such as IFNs (beta-1a or beta-1b), and glatiramer acetate. More recently, oral immunosuppressant teriflunomide and dimethyl fumarate became registered MS treatments. Depending on country regulations and reimbursement criteria, alternative treatments eg, fingolimod, natalizumab, or alemtuzumab can be administered to MS patients with highly-active disease. For all these treatments, success strongly depends on the patients’ therapy adherence.3 Previous research has indicated that adherence to DMDs is often poor,4–6 potentially resulting in health deterioration and adding to the financial burden to the health care system.6–8 It is often assumed that the alternative route of administration of oral therapies leads to better adherence, but there is no reliable scientific evidence for this assumption.9
Several interventions have been explored over the years, aiming to increase patient adherence to DMDs. Good communication between patients and physicians or other health care providers, and patient education have been recognized as important factors that can positively affect adherence.10,11 This could, for instance, be facilitated by patient support programs offering enhanced therapy guidance and counseling to the patients.12,13 However, such support programs can be expensive as they require the involvement of qualified personnel, and are costly in terms of time. A convenient and cost-saving option to facilitate treatment monitoring and patient–physician communication may be the use of electronic monitoring systems.
One such system is the RebiSmart® electronic autoinjector (the IFN beta-Ia autoinjector device) (Ares Trading SA, Coinsins, Switzerland), developed to administer injections of subcutaneous (sc) IFN beta-1a (Rebif®, Merck Serono Europe Limited, London, UK, an affiliate of Merck KGaA, Darmstadt, Germany). The IFN beta-Ia autoinjector device allows patients to individually adjust comfort settings such as injection speed and depth, and electronically stores date and time of injections, cartridge changes, and prescribed doses. These data can be viewed by patients and physicians using a specifically designed software system, allowing identification of potential adherence issues and encouraging discussion between patients and physicians.14
The implications for adherence, and ultimately the impact on patients’ health, of implementing such electronic monitoring systems need to be thoroughly investigated to determine whether these systems are worthwhile – especially in daily medical practice. To our knowledge, only three studies included analyses of treatment adherence in patients using the IFN beta-Ia autoinjector device system so far.15–18 Two studies were prospective observational studies conducted in various European countries;15,16 the third study was a retrospective audit of adherence data collected in daily practice in the UK and Ireland.17 The outcomes of these studies suggest that patients using the IFN beta-Ia autoinjector device are more adherent than those using traditional injection methods to administer DMDs. Nevertheless, more evidence is needed to determine whether these results hold in other settings and to identify potential country-specific differences. Therefore, this retrospective observational study aimed to assess adherence in patients with MS using the IFN beta-Ia autoinjector device in a real life setting in Germany and the Netherlands.
Patients and methods
Design and data source
The study was a retrospective, observational analysis of data collected from the IFN beta-Ia autoinjector devices that had been used by patients with MS in routine medical care in Germany and the Netherlands, for the injection of sc IFN beta-1a. In both the Netherlands and in Germany the IFN beta-Ia autoinjector devices were distributed by a single pharmacy (ApotheekZorg, 5531 AG Bladel, the Netherlands; Bahnhofapotheke, 59199 Bönen, Germany). The IFN beta-Ia autoinjector devices analyzed in this study had been returned by patients between October 2009 and December 2012 to these pharmacies for replacement or upon termination of treatment. In Germany, the devices originated from patients who had registered with a support service (Merck Serono Service Center, hosted by Sanvartis GmbH, Duisburg, Germany), which included access to a helpline and home visits by a qualified nurse. Demographic data (age and sex) were available for German patients only. Device replacement was due after 3 years. Anonymized data of patients who retrospectively provided their consent for the processing of their data were included in the analyses. Treatment data collected from the IFN beta-Ia autoinjector devices included date of injection, duration of injection, type of injection/activity (normal injection, incomplete injection, cartridge change), and dose. This noninterventional study analyzing anonymous data did not include people, medical records, or human tissue, therefore this study does not fall into the scope of the German Drug Act (Arzneimittelgesetz) and the Dutch Medical Research Involving Human Subjects Act (Wet medisch-wetenschappelijk onderzoek met mensen). Ethical approval was consequently not required in Germany and the Netherlands. In line with the German data protection law (Bundesdatenschutzgesetz), all data were anonymized and all patients provided their consent for processing of their data. Moreover, the anonymization and use of the data was conducted in compliance with Dutch data privacy law (Wet bescherming persoonsgegevens).
Endpoints
The endpoints of primary interest were adherence (%) to sc IFN beta-1a, based on the injection data recorded by the IFN beta-Ia autoinjector device and the proportion of adherent patients. Adherence was calculated as ([number of administered injections]/[number of scheduled injections]) ×100%. The recommended dose of sc IFN beta-1a administered by the IFN beta-Ia autoinjector device is 22 or 44 μg three times per week, according to the Summary of Product Characteristics19 (note that new patients should start on 8.8 μg). Thus, the number of scheduled injections was estimated as 3× (treatment duration in weeks). Patients were considered adherent if they had administered ≥80% of scheduled injections. Treatment duration was analyzed as the time between first and last injection, as recorded by the IFN beta-Ia autoinjector device. Other endpoints were the proportion of patients who administered >95% of scheduled injections, the number and duration of treatment interruptions (defined as a gap of >10 days between two consecutive injections), and use of complete cartridge, which was calculated as ([number of completely used cartridges]/[number of all used cartridges]) ×100%. A cartridge was considered completely used if a new cartridge was inserted after three normal injections according to the log of the IFN beta-Ia autoinjector device. The mean dose of sc IFN beta-1a per week and the mean number of injections per week, calculated as ([sum of all single doses or number of injections]/[treatment duration in weeks]), were also assessed.
Statistical analysis
Endpoint analysis was performed on the full analysis set, which comprised all patients for whom adherence, based on the IFN beta-Ia autoinjector device injection log, could be calculated. Patients were stratified into subgroups by country and treatment status: “pretreated” (IFN beta-1a dose of first recorded injection was 22/44 μg) or “treatment-naïve” (dose of first injection was 8.8 μg). Furthermore, patients from Germany were divided into subgroups by age (≤40 years and >40 years) and sex.
Summary statistics, including mean, median, standard deviation (SD), and range were computed for continuous variables, and counts and proportions were computed for categorical data. Differences in adherence (%), use of complete cartridge (%), treatment duration, number of treatment interruptions, mean weekly dose, and mean number of injections per week between subgroups were assessed ad hoc using the nonparametric Mann–Whitney U test. The tests were two-sided at the 5% level of significance. The statistical software package SAS® version 9.3 (SAS Institute Inc., Cary, NC, USA) was used for all analyses.
Results
Patients
The full analysis set comprised a total of 1,682 patients: 1,340 (79.7%) from Germany and 342 (20.3%) from the Netherlands. The demographic data of the German patients are summarized in Table 1. A higher proportion of women (72.5%) than men (27.5%) were observed in the German sample, as was expected for this indication, and the mean age was 41.1 years. Based on the first dose in the injection log, 1,110 (66.0%) patients were pretreated and 572 (34.0%) patients were treatment-naïve with regard to IFN beta-1a.
Adherence
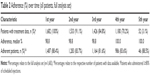
The mean (±SD) adherence to sc IFN beta-1a over the entire treatment period (mean treatment duration discussed in the following sections), as derived from the data logged by the IFN beta-Ia autoinjector device, was 90.7%±17.3% (median: 98.1%). As shown in Table 2, 70.2% of all patients still used their the IFN beta-Ia autoinjector device in the fourth year after the first recorded injection. Median adherence remained at the same high level throughout the observational period (it has to be noted however, that the sample size decreased over time and was very small in the fifth year). The median adherence rates were similar between German and Dutch patients (97.9% vs 99.0%). Likewise, as shown in Table 3, small differences were found in adherence between pretreated and treatment-naïve patients (median adherence: 97.7% vs 99.0%), patients aged ≤40 years and >40 years (97.4% vs 98.2%), and women and men (97.7% vs 98.4%). The last two subgroup comparisons included only patients from Germany.
Of all patients, 1,395 (82.9%) were considered adherent, as they had administered ≥80% of scheduled injections. The number of patients with adherence >95% was 1,082 (64.3%). The proportion of adherent patients was slightly higher in the Dutch than the German subgroup, especially with regard to adherence >95% (Figure 1). The proportions of adherent patients are presented for all subgroups in Table 3, showing that the number of adherent patients was higher among treatment-naïve patients and, for Germany only, older (aged >40 years) patients, and men.
  | Figure 1 Patients (%) adherent (adherence ≥80%) or non-adherent (adherence <50%–79%) to sc IFN beta-1a over the entire treatment period. |
Completely used cartridges
A cartridge contains three doses of IFN beta-1a. The mean (±SD) proportion of cartridges that was used completely was 94.8% (±9.8%) in all patients. The median percentage of completely used cartridges was 97.9% in all patients, 98.2% in German patients, and 95.7% in Dutch patients. The small difference between the two countries was significant (P<0.001).
Treatment duration and interruptions
The mean (±SD) period between the first and the last injection logged by the IFN beta-Ia autoinjector device was 150.1 (±46.7) weeks. The longest treatment duration, ie, the longest time a device had been used by a patient, was 252.7 weeks (~5 years). The proportion of patients who returned their device within the first year was higher in the Netherlands than in Germany: 69.3% of Dutch patients used their the IFN beta-Ia autoinjector device in the second year compared to 96.7% of German patients. The median duration of treatment was shorter for patients in the Netherlands than for patients in Germany (P<0.001; Table 4).
The mean (±SD) number of treatment interruptions was 1.4 (±3.3) (median: 0 interruptions). There was no significant difference in the frequency of treatment interruptions between countries (Table 4). The mean (±SD) length of the treatment interruptions was 60.5 (±103.9) days for all patients (n=687), 58.6 (±102.4) days for German patients (n=551), and 68.5 (±110.3) days for Dutch patients (n=135).
Dosage and number of injections
The mean (±SD) weekly dose of sc IFN beta-1a was 97.2 (±32.7) μg (median: 106.9 μg) in all patients. During the treatment period, dose modifications were observed in 1,201 patients (71.4%). The median value of the mean weekly dose was significantly higher in patients in the Netherlands than in patients in Germany (P<0.001; Table 4). The mean (±SD) weekly number of administered injections was on average 2.7 (±0.5; median: 2.9). The median values of the mean weekly number of injections were similar between German and Dutch patients, but the Mann–Whitney U test detected a significant difference in the spread of the data (P=0.039; Table 4).25
Discussion
Adherence to IFN beta-1a in patients with MS was measured retrospectively by analyzing treatment data recorded by the IFN beta-Ia autoinjector device. Electronic systems for monitoring treatment adherence in MS and other chronic diseases have been shown to be more reliable than patient self-reporting.20,21
We observed high adherence among patients under routine medical care in Germany and the Netherlands. On average, 91% of scheduled injections had been administered by the patients. Overall, the proportion of adherent patients (≥80% of scheduled injections administered) over the entire treatment period was 83%. Earlier studies investigating adherence to DMDs among patients with MS reported considerably lower proportions of adherent patients.4,22 A retrospective study including 1,211 patients initiated on sc IFN beta-1a in the US found that 59% were adherent.22 In another study analyzing adherence to DMDs for the therapy of MS, using medication profiles of 50,057 patients from Germany, the proportion of patients adherent to sc IFN beta-1a was only 39%.4 In contrast to our study, these studies were based on medical and pharmacy claims data, and adherent patients were defined as showing a medication possession ratio (MPR) ≥0.8 at observation periods of 12–36 months22 or 24 months,4 respectively. The MPR is a common method for measuring adherence based on dispensed medication, but it cannot verify that the medication has actually been used, and it may be prone to overestimation of adherence.17 In addition, the data analyzed in these studies4,22 originate from a time (between 2000 and 2009) when the IFN beta-Ia autoinjector device had not yet been available for the administration of sc IFN beta-1a. Manual application of IFN beta-1a has been shown to be associated with a higher incidence of injection site reaction than autoinjection, which may suggest improved adherence in patients using automatic injection devices.23 Therefore, due to the differences in the methods of assessing adherence and drug application, a direct comparison between these earlier studies and the present analysis is not possible.
Three recent studies, another retrospective and two prospective observational studies, also investigated adherence in MS patients by analyzing data of actually administered doses of sc IFN beta-1a recorded by the IFN beta-Ia autoinjector device.15–18 Furthermore, the definition of adherence in these studies was very similar to that used in our study. Although slightly lower, the adherence rates observed in our study are in line with those seen in these three studies. The retrospective analysis by Willis et al17 of the IFN beta-Ia autoinjector device data from 225 patients in the UK and Ireland, who continued therapy for at least 2 years, yielded a mean adherence rate of 95% and showed that 91% of the patients were adherent (≥80% adherence) at month 24. A prospective observational study in 119 patients in Italy showed that after 12 weeks of treatment, 88% of the patients were adherent (≥80% adherence).15 A very high mean adherence rate of 97% at month 12 (or at the time of early discontinuation) was also observed in 791 patients included in a prospective observational study performed in 14 countries across Europe.16
It has been suggested that participants of clinical studies may be more motivated to adhere to their prescribed treatment regimens24; thus, study participation per se may have influenced the behavior of the patients enrolled in the prospective studies. In our study, adherence was measured in patients under routine care conditions, who were not aware at the time of the IFN beta-Ia autoinjector device usage, that the logged data would be used for research purposes. The conditions were similar in the retrospective study performed by Willis et al,17 but had a smaller sample size than in our study, and only included patients who persisted with treatment for a minimum of 2 years. Therefore, despite the similarities between the studies regarding setting, evaluation criteria, and method of sc IFN beta-1a application, other differences in the design have to be taken into account when comparing adherence results.
Adherence to prescribed drugs can vary considerably between countries. The reasons for these differences remain unclear and do not seem to be due to sociodemographic and socialeconomic factors.26 The median adherence rate of patients in Germany was similar to that of patients in the Netherlands. Median adherence rates were also similar between men and women, younger and older patients, and treatment-naïve and pretreated patients. Patients naïve to IFN beta-1a treatment seemed to be more adherent than pretreated patients. In a previous study, treatment-naïve MS patients were less adherent to DMD therapy due to injection site reactions than patients who switched from another DMD.27 The use of an electronic autoinjector such as the IFN beta-Ia autoinjector device may reduce injection pain and influenza-like symptoms and thus promote adherence, especially in the early stages of therapy.15,16,28 In addition, being able to self-monitor their treatment by electronic logs, and becoming involved in their therapy may help patients to get used to a treatment regimen that has to be adhered to for a long time.
In the present study, the observational period or treatment duration was not predefined, but was derived individually from the injection logs. The results showed that ~70% of the patients had used the same the IFN beta-Ia autoinjector device over a period of >3 years (5% had used the same device for >4 years). The high level of adherence (median rates per year) was maintained over the entire observation period of up to 5 years. The median treatment duration, as recorded by the IFN beta-Ia autoinjector device, was 167 weeks in German patients, which corresponds well with the recommended replacement interval of 3 years. In the Netherlands, the median treatment duration was close to 2 years, suggesting that either scheduled replacement intervals were shorter or persistence to the therapy was lower. Indeed, the proportion of patients returning their the IFN beta-Ia autoinjector device within or after the first year was considerably higher in the Netherlands than in Germany. The reason for this difference cannot be determined because the reasons for returning the devices were not documented.
Based on the injection log data, ~5% of the used cartridges were not completely empty. Usually, a cartridge can only be removed if the device indicates that the cartridge needs to be replaced. Replacement is due when there is not enough medication left for a full prescribed dose. Interrupted injections, eg, due to injection pain, which are not completed may result in leftover medication in the cartridge. Furthermore, the cartridge needs to be replaced if the medication is not used up within 28 days, the needle is not removed within 30 minutes after injection, or the cartridge is damaged. Although we did not collect the reasons for cartridge replacements and their frequency, our results suggest an overall low incidence of incomplete injections or incorrect usage of the device, and thus low medication wastage.
Limitations
The persistence component of adherence was not considered in the analysis of adherence rates. The calculation of treatment duration, and consequently of adherence, was based on the time between first and last recorded injection irrespective of treatment interruptions (gaps >10 days between two injections). Such gaps were identified in 41% of the patients. As the reasons for treatment interruptions were not documented, adherence may have been underestimated in patients who interrupted treatment in agreement with their physician due to medical reasons (eg, in case of pregnancy). Furthermore, the reasons for returning the IFN beta-Ia autoinjector devices were unknown (eg, scheduled replacement, device defects, or adverse reactions). In a few patients, eg, patients with an incomplete injection in addition to three normal injections per week (this is possible if, during, the incomplete injection the device is removed from the skin before there is any significant release of medication from the cartridge), adherence was overestimated due to the way this endpoint was computed. Adherence was also overestimated in cases where the prescribed weekly dose was spread over more than three injections. The high observed maximum values of adherence (190%) and the mean number of injections per week (5.7) were from a patient who injected 22 μg of sc IFN beta-1a twice daily (within a few hours) on 3 days a week during most of the 176 weeks recorded by the patient’s injection device. Whether this regimen was in accordance with the prescription is unknown. Nevertheless, it shows that monitoring treatment behavior of patients through their doctors or other health care professionals, may also be important for preventing some patients from taking higher than the prescribed doses.
Selection bias due to the decreasing number of patients with available IFN beta-Ia autoinjector device data over time might have been possible, for instance, if shorter treatment durations were associated with reduced motivation and non-adherence. The IFN beta-Ia autoinjector device does not indicate the actual injected dose. Thus, incomplete injections were included in the analysis with the prescribed dose, which caused slight overestimation of the mean weekly IFN beta-1a dose. However, only 0.5% of all injections were incomplete (results not shown).
Previous IFN therapy was assumed based on the dose of the first injection recorded by the IFN beta-Ia autoinjector device. However, we had no data to verify that patients starting with the 8.8 μg titration dose were truly treatment-naïve, or that patients receiving 22 μg or 44 μg were not treatment-naïve. A diagnosis of MS was assumed for all patients, as IFN beta-1a administered via the IFN beta-Ia autoinjector device is approved only for this indication. No information on the patients’ MS history was available. A selection bias, due to the collection of devices from patients who had registered with a support service in Germany, cannot be excluded. These patients may have been more likely to adhere, as studies in MS patients have reported a positive effect on adherence through telephone support and motivational interviewing.12 As it was not known whether the patients from the Netherlands had received nursing support or not, a potential influence could not be evaluated.
Conclusion
The high adherence to sc IFN beta-1a observed in this retrospective study in MS patients under routine care using the IFN beta-Ia autoinjector device suggests, together with similar results of previous studies, that the use of an electronic injection device may promote treatment adherence. There are various factors associated with the use of such a device that may exert a positive effect on adherence. The individual contributions of these factors, including ease of use of the device, improved injection tolerance, enhanced treatment monitoring through patients and physicians, or additional home and telephone support services, need to be investigated in different cultural environments in comparative studies.
Acknowledgment
The authors thank Jana Distler, Werner Fink, and Tanja Henrichs of syneed medidata GmbH, Konstanz, Germany, for data analysis and assistance in preparing this manuscript, which was funded by Merck KGaA, Darmstadt, Germany.
Disclosure
Marieke Krol is a former employee and Gert de Voer is an employee of Merck BV, Schiphol-Rijk, the Netherlands, an affiliate of Merck KGaA, Darmstadt, Germany. Ulrike Osowski is an employee of Merck KGaA, Darmstadt, Germany. The authors report no other conflicts of interest in this work.
References
Butler M, Forte ML, Schwehr N, Carpenter A, Kane RL. Decisional dilemmas in discontinuing prolonged disease-modifying treatment for multiple sclerosis. Comparative Effectiveness Review. No. 150. | ||
Kingwell E, Marriott JJ, Jetté N, et al. Incidence and prevalence of multiple sclerosis in Europe: a systematic review. BMC Neurol. 2013;13:128. | ||
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. | ||
Hansen K, Schüssel K, Kieble M, et al. Adherence to disease modifying drugs among patients with multiple sclerosis in Germany: a retrospective cohort study. PLoS One. 2015;10(7):e0133279. | ||
Wong J, Gomes T, Mamdani M, Manno M, O’Connor PW. Adherence to multiple sclerosis disease-modifying therapies in Ontario is low. Can J Neurol Sci. 2011;38(3):429–433. | ||
Tan H, Cai Q, Agarwal S, Stephenson JJ, Kamat S. Impact of adherence to disease-modifying therapies on clinical and economic outcomes among patients with multiple sclerosis. Adv Ther. 2011;28(1):51–61. | ||
Yermakov S, Davis M, Calnan M, et al. Impact of increasing adherence to disease-modifying therapies on healthcare resource utilization and direct medical and indirect work loss costs for patients with multiple sclerosis. J Med Econ. 2015;18(9):711–720. | ||
Devonshire V, Lapierre Y, Macdonell R, et al. The Global Adherence Project (GAP): a multicenter observational study on adherence to disease-modifying therapies in patients with relapsing-remitting multiple sclerosis. Eur J Neurol. 2011;18(1):69–77. | ||
Sartori A, Carle D, Freedman MS. Teriflunomide: a novel oral treatment for relapsing multiple sclerosis. Expert Opin Pharmacother. 2014;15(7):1019–1027. | ||
Remington G, Rodriguez Y, Logan D, Williamson C, Treadaway K. Facilitating medication adherence in patients with multiple sclerosis. Int J MS Care. 2013;15(1):36–45. | ||
Lugaresi A, Rottoli MR, Patti F. Fostering adherence to injectable disease-modifying therapies in multiple sclerosis. Expert Rev Neurother. 2014;14(9):1029–1042. | ||
Caon C, Saunders C, Smrtka J, Baxter N, Shoemaker J. Injectable disease-modifying therapy for relapsing-remitting multiple sclerosis: a review of adherence data. J Neurosci Nurs. 2010;42(5 Suppl): S5–S9. | ||
Turner AP, Sloan AP, Kivlahan DR, Haselkorn JK. Telephone counseling and home telehealth monitoring to improve medication adherence: results of a pilot trial among individuals with multiple sclerosis. Rehabil Psychol. 2014;59(2):136–146. | ||
Lugaresi A. RebiSmart™ (version 1.5) device for multiple sclerosis treatment delivery and adherence. Expert Opin Drug Deliv. 2013;10(2):273–283. | ||
Lugaresi A, Florio C, Brescia-Morra V, et al. Patient adherence to and tolerability of self-administered interferon β-1a using an electronic autoinjection device: a multicentre, open-label, phase IV study. BMC Neurol. 2012;12:7. | ||
Bayas A, Ouallet JC, Kallmann B, Hupperts R, Fulda U, Marhardt K; SMART study group. Adherence to, and effectiveness of, subcutaneous interferon β-1a administered by RebiSmart® in patients with relapsing multiple sclerosis: results of the 1-year, observational SMART study. Expert Opin Drug Deliv. 2015;12(8):1239–1250. | ||
Willis H, Webster J, Larkin AM, Parkes L. An observational, retrospective, UK and Ireland audit of patient adherence to subcutaneous interferon beta-1a injections using the RebiSmart(®) injection device. Patient Prefer Adherence. 2014;8:843–851. | ||
Lugaresi A, De Robertis F, Clerico M, et al. Long-term adherence of patients with relapsing-remitting multiple sclerosis to subcutaneous self-injections of interferon β-1a using an electronic device: the RIVER study. Expert Opin Drug Deliv. 2016;13(7):931–935. | ||
European Medicines Agency. Summary of Product Characteristics Rebif. EMA; 2009. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000136/WC500048681.pdf. Accessed April 21, 2017. | ||
Bruce JM, Hancock LM, Lynch SG. Objective adherence monitoring in multiple sclerosis: initial validation and association with self-report. Mult Scler. 2010;16(1):112–120. | ||
Greenlaw SM, Yentzer BA, O’Neill JL, Balkrishnan R, Feldman SR. Assessing adherence to dermatology treatments: a review of self-report and electronic measures. Skin Res Technol. 2010;16(2):253–258. | ||
Halpern R, Agarwal S, Dembek C, Borton L, Lopez-Bresnahan M. Comparison of adherence and persistence among multiple sclerosis patients treated with disease-modifying therapies: a retrospective administrative claims analysis. Patient Prefer Adherence. 2011;5:73–84. | ||
Mikol D, Lopez-Bresnahan M, Taraskiewicz S, Chang P, Rangnow J; Rebiject Study Group. A randomized, multicentre, open-label, parallel-group trial of the tolerability of interferon beta-1a (Rebif) administered by autoinjection or manual injection in relapsing-remitting multiple sclerosis. Mult Scler. 2005;11(5):585–591. | ||
van Onzenoort HA, Menger FE, Neef C, et al. Participation in a clinical trial enhances adherence and persistence to treatment: a retrospective cohort study. Hypertension. 2011;58(4):573–578. | ||
Hart A. Mann-Whitney test is not just a test of medians: differences in spread can be important. BMJ. 2001;323(7309):391–393. | ||
Larsen J, Stovring H, Kragstrup J, Hansen DG. Can differences in medical drug compliance between European countries be explained by social factors: analyses based on data from the European Social Survey, round 2. BMC Public Health. 2009;9:145. | ||
Fernández-Fournier M, Tallón-Barranco A, Chamorro B, Martínez-Sánchez P, Puertas I. Differential glatiramer acetate treatment persistence in treatment-naive patients compared to patients previously treated with interferon. BMC Neurol. 2015;15:141. | ||
Devonshire V, Arbizu T, Borre B, et al. Patient-rated suitability of a novel electronic device for self-injection of subcutaneous interferon beta-1a in relapsing multiple sclerosis: an international, single-arm, multicentre, Phase IIIb study. BMC Neurol. 2010;10:28. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.