Back to Journals » Clinical Interventions in Aging » Volume 12
Multimorbidity as specific disease combinations, an important predictor factor for mortality in octogenarians: the Octabaix study
Authors Ferrer A , Formiga F, Sanz H, Almeda J , Padrós G
Received 25 September 2016
Accepted for publication 17 November 2016
Published 27 January 2017 Volume 2017:12 Pages 223—231
DOI https://doi.org/10.2147/CIA.S123173
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Assumpta Ferrer,1 Francesc Formiga,2,3 Héctor Sanz,4 Jesús Almeda,5,6 Glòria Padrós7
On behalf of the Octabaix Study Group
1Primary Healthcare Department, Centre ‘El Plà’, DAP Metropolitana Sud ICS, 2Geriatric Unit, Internal Medicine Service, Hospital Universitari de Bellvitge, L´Hospitalet de Llobregat, Barcelona, 3Bellvitge Biomedical Research Department Institute, IDIBELL, L’Hospitalet de Llobregat, 4ISGlobal, Barcelona Ctr Int Health Res (CRESIB), Hospital Clínic – Barcelona University, 5Support Unit Research for Primary Care, Primary Health Care Department of Costa Ponent, IDIAP, ICS, 6CIBER Department of Epidemiology Service (CIBERESP), 7Clinical Laboratory Department, L´Hospitalet de Llobregat, Barcelona, Spain
Background: The population is aging and multimorbidity is becoming a common problem in the elderly.
Objective: To explore the effect of multimorbidity patterns on mortality for all causes at 3- and 5-year follow-up periods.
Materials and methods: A prospective community-based cohort (2009–2014) embedded within a randomized clinical trial was conducted in seven primary health care centers, including 328 subjects aged 85 years at baseline. Sociodemographic variables, sensory status, cardiovascular risk factors, comorbidity, and geriatric tests were analyzed. Multimorbidity patterns were defined as combinations of two or three of 16 specific chronic conditions in the same individual.
Results: Of the total sample, the median and interquartile range value of conditions was 4 (3–5). The individual morbidities significantly associated with death were chronic obstructive pulmonary disease (COPD; hazard ratio [HR]: 2.47; 95% confidence interval [CI]: 1.3; 4.7), atrial fibrillation (AF; HR: 2.41; 95% CI: 1.3; 4.3), and malignancy (HR: 1.9; 95% CI: 1.0; 3.6) at 3-year follow-up; whereas dementia (HR: 2.04; 95% CI: 1.3; 3.2), malignancy (HR: 1.84; 95% CI: 1.2; 2.8), and COPD (HR: 1.77; 95% CI: 1.1; 2.8) were the most associated with mortality at 5-year follow-up, after adjusting using Barthel functional index (BI). The two multimorbidity patterns most associated with death were AF, chronic kidney disease (CKD), and visual impairment (HR: 4.19; 95% CI: 2.2; 8.2) at 3-year follow-up as well as hypertension, CKD, and malignancy (HR: 3.24; 95% CI: 1.8; 5.8) at 5 years, after adjusting using BI.
Conclusion: Multimorbidity as specific combinations of chronic conditions showed an effect on mortality, which would be higher than the risk attributable to individual morbidities. The most important predicting pattern for mortality was the combination of AF, CKD, and visual impairment after 3 years. These findings suggest that a new approach is required to target multimorbidity in octogenarians.
Keywords: oldest old, multimorbidity, chronic diseases, mortality, atrial fibrillation, malignancy
Introduction
Multimorbidity is highly prevalent in the elderly, and such coexistence leads to long-term disorders.1 However, health care systems are largely aimed at individual diseases rather than multimorbidity often redundant, impractical, and sometimes even harmful care.2,3 The prevalence of multimorbidity is reported to be 62% among those aged 65–74 years and 82% for those aged ≥85 years.4 Therefore, medical research is needed to assess a more comprehensive clinical approach to multimorbidity and its effects, particularly in the oldest old.5–7
The evaluation of multimorbidity is difficult; thus, consensus regarding the number and types of diseases that should be included in multimorbidity does not exist,8 and prevalence estimates are highest when using an open list of diagnoses, data from general practice (eg, general population or patients from general practice), and a low cutoff point conditions (eg, if multimorbidity is defined by a minimum of two or three diagnoses).4,8 Conversely, the effects of multimorbidity remain uncertain, specifically those related to mortality. In previous studies, beyond a reported effect on mortality at 10 years and 3 years of multimorbidity in young elders9,10 and in octogenarians,11,12 multimorbidity lost its effect when adjusted for functionality. Recent research has begun to focus on more comprehensive perspective rather than the concept of multimorbidity as a summary of indices, in order to understand how morbidities cluster or co-occur in the same individual.13,14 This would be important because the concept of multimorbidity as specific disease-to-disease interactions within combinations may accelerate the development of functional limitations, disability, and mortality.5,10
In light of the above, the aim of this study was to explore the association between the patterns of multimorbidity by specific group diseases and survival after 3 and 5 years of follow-up periods, in an existing population-based cohort study of aging and falling of octogenarians.
Materials and methods
The current data were gathered from the longitudinal data set of Octabaix study project, a 3-year randomized clinical intervention program to prevent falls and malnutrition in 328 community-dwelling inhabitants all born in the year 1924.15,16 The Octabaix project is a prospective population-based study on aging with a primary purpose on falls and malnutrition assessment. All community-dwelling inhabitants born in 1924 (aged 85 years at the time of inclusion) and registered at one of seven primary health care centers in Baix Llobregat in Barcelona, Spain, were contacted. The combined population served by these health care teams included ~210,000 inhabitants of the nearly 800,000 inhabitants in the whole of the Baix Llobregat area. The corresponding referral hospital, at the time the study began, was the Hospital Universitari de Bellvitge. Geriatric assessment was performed, and sociodemographic data were recorded. The study included, from among 487 eligible subjects, 328 noninstitutionalized participants. No criteria related to baseline health or cognitive status was applied to exclude patients. The only exclusion criterion was to be institutionalized. Different reasons for noninclusion were 76 (10.9%) living in unregistered nursing homes as listed, 67 (9.6%) died before the study started, and 66 (9.4%) displaced to another city. The participation rate was 67.5%, and there were no differences among respondents and nonrespondents in terms of gender, health care center, or physician in charge. The study was approved by the institutional ethics committee of the Jordi Gol Institute for Primary Care Research IDIAP. All patients or their caregivers gave written informed consent before enrollment.
Subjects were examined by medical doctors and nurses, specially trained in elderly interviewing to control the inter-rater reliability. The interview was done at the place of residence of participants and included a geriatric assessment and the collection of sociodemographic data. Functional status was measured using the Barthel functional index (BI)17 for the basic activities of daily living (ADL). The total score of the BI ranges from 0 to 100 points (from help needed to be independent in all activities). Cognitive function was measured by the Spanish version of the Mini-Mental State Examination (MEC)18 (lower or equal scoring to 23/35 indicates cognitive impairment). The Charlson Index was used to measure global comorbidity.19 The Charlson score ranges from 0 to a theoretical maximum of 33, depending on the presence of certain diseases with assigned values. The Charlson Comorbidity Index was used to measure overall comorbidity. Scores here range from 0 to a theoretical maximum of 33, depending on the presence of certain diseases with assigned values. Nutritional status was assessed using the Mini-Nutritional Assessment,20 which has a maximum score of 30 and scores of <23.5 classified as a risk of malnutrition. The clinical trial is registered in US National Institutes of Health Clinical Trial: NCT01141166.
Procedure
Multimorbidity was defined as the combination of co-occurred specific chronic conditions within one person. A disease was classified as chronic if it was permanent and caused by nonreversible pathological alterations. All data sources were coded according to the standardized ICD-10. For the purpose of this study, the analysis focused on the 16 most common chronic health conditions:16 hypertension, diabetes mellitus, dyslipidemia, ischemic cardiomyopathy (including myocardial infarction, coronary heart disease, and angina), heart failure, stroke (including transient ischemic attack), chronic obstructive pulmonary disease (COPD (including chronic bronchitis or emphysema and asthma), atrial fibrillation (AF), peripheral arterial disease, Parkinson’s disease, malignancy (including any malignant tumors), dementia, anemia, chronic kidney disease (CKD when the glomerular filtration rate was <60 mL/min/1.73 m2), visual impairment, and deafness.
Mortality, measured as time to all-cause death, was considered the primary outcome. The vital status of the participants was evaluated annually during the 5-year follow-up. Additionally for that purpose, we collected the exact date of death by other electronic clinical registers and if these dates were not available, then by death certificates. Participants who were unavailable for follow-up were censored at the time of dropping out and were included as censored information in the analysis.
Categorical variables are shown as frequencies and percentages while quantitative variables are presented as median and interquartile range due to the nonnormality distribution of the variable (previously assessed by normal probability plots). In the bivariate analysis for baseline characteristics, either the chi-square or Fisher’s exact test was used to compare categorical variables between men and women. The Mann–Whitney test was applied to compare quantitative variables across groups. A first analysis was performed by Kaplan–Meier curves for time to death at the 3- and 5-year follow-up periods for all individual 16 morbidities previously described. The three individual morbidities most associated with death on the highest chi-square from the log-rank test statistic were retained. A similar approach by Kaplan–Meier curves was used for all combinations of two and three morbidities. In these cases, for each of the possible combinations of two and three morbidities, participants of these particular combinations were compared to the rest (eg, in the scenario of two morbidities, participants with both A and B morbidities are compared to the rest including those with none or at most one of two; the same reasoning is applied for three morbidities). On the basis of the chi-square log-rank test statistic performed for each combination, the three morbidities most associated for each group of variables were retained. A second analysis by Cox proportional hazard models was fit for the retained individual morbidity and combinations of co-occurred morbidities. Models adjusted by gender and BI were also fit, and hazard ratios (HRs) with the 95% confidence interval (CI) were estimated. Proportional hazard assumptions were tested in all models performing scaled Schoenfeld residuals and log (−log) transformation in Kaplan–Meier curves. Finally, for the two combined morbidity models retained, the interaction was tested assuming an alpha level of 0.05. All analyses were performed using R software (version 3.3.2; The R Foundation for Statistical Computing, Vienna, Austria).
Results
The sample included 202 women (61.6%) and 174 were widowed (53.0%). Sixty two (19.0%) had more than 6 years of formal education, while the remaining 266 (81.0%) had only primary schooling or no formal education at all. One hundred and seventy-four (53.0%) participants had a caregiver. In terms of functional status, the mean (standard deviation [SD]) BI score was 87.5 (19), whereas the mean of the MEC cognition test was 26.6 (6.8). Of the total sample, 95.1% participants had more than one co-occurring disease of all the selected chronic conditions defined and the median and the interquartile range value of the number of chronic conditions was 4 (3–5) during the study period. Table 1 shows differences in baseline characteristics according to gender. Differences of gender in these morbidities were a greater number of COPD (P=0.016), malignancy (P<0.001), and nutritional risk (P=0.016) in men; whereas, women had more cognitive decline (P=0.040) and falls (P=0.006).
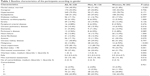  | Table 1 Baseline characteristics of the participants according to gender |
Of the total sample, 59 (18.0%) subjects died by the third year and 146 (44.5%) by the fifth year. Figure 1 shows the individual morbidities and multimorbidity combinations most associated, with time to death at 3- and 5-year follow-up periods, respectively. Tables 2 and 3 show the individual morbidities and disease combinations most associated with time to death. The individual morbidities significantly associated with death were COPD (HR: 2.47; 95% CI: 1.3; 4.7), AF (HR: 2.41; 95% CI: 1.3; 4.3), and malignancy (HR: 1.9; 95% CI: 1.0; 3.6) by 3 years, whereas dementia (HR: 2.04; 95% CI: 1.3; 3.2), malignancy (HR: 1.84; 95% CI: 1.2; 2.8), and COPD (HR: 1.77; 95% CI: 1.1; 2.8) were the most associated with mortality at 5-year follow-up, after adjustment through BI. During the 3-year follow-up period, patterns of multimorbidity groups for two diseases showed an HR of mortality of 3.81 (1.9; 7.4) for AF and CKD, 2.66 (1.5; 4.8) for AF and visual impairment, and 2.40 (1.2; 4.9) for anemia and CKD adjusting by BI. For the group of three diseases, AF, CKD, and visual impairment with an HR of 4.19 (2.2; 8.2) was the most important multimorbidity associated with death (in the BI adjusted model). At the 5-year follow-up period, patterns of multimorbidity for two and three diseases showed a significant HR of death of 2.66 (1.4; 5.0) for anemia and malignancy, 3.24 (1.8; 5.8) for hypertension, CKD, and malignancy, and 2.91 (1.7; 5.0) for dyslipidemia, malignancy, and visual impairment, after adjustment through BI.
Table 4 shows that for the 5-year follow-up period, the most significant interaction was found between dyslipidemia and malignancy (P=0.005). In the other models, no statistical interactions were found. For the 3-year follow-up period, no interaction between either the two retained comorbidity models was found.
Discussion
This study found that multimorbidity patterns of AF, CKD, and visual impairment at 3-year follow-up, whereas hypertension, CKD, and malignancy at 5-year follow-up are the most important predicting factors for mortality. When cancer co-occurred with other conditions, it appeared as an important synergistic factor that intensified mortality risk. Therefore, multimorbidity may lead specific disease combinations to have more than an additive risk on the effect of death.
Several studies have demonstrated the effect of multimorbidity on mortality, such as the Lee et al study21 on population-based community-dwelling adults in the USA and Walter et al22 on hospitalized patients. However, differences between studies existed and methods varied. Therefore, besides the reported influence of the number of diseases included in the definition of multimorbidity, which directly increases the risk of mortality,23 a second reason for these differences may be the choice of the conditions included in multimorbidity indices. These conditions should preferably be related to the (primary) study outcome because of their varying impact on the study.5,22 Thus, our study, with 16 chronic conditions including CKD of a proven impact on mortality,24 reported an important effect on death. Marengoni et al23 in a study consisting of 22 conditions, including arthritis, polymyalgia, or rheumatoid arthritis of a proven impact on disability as well as Wong et al,25 including different psychiatric disorders, reported an association with disability and health-related quality, respectively, rather than on mortality. A third explanation for these differences may be the severity of the disease.8 Thereby, Gené et al26 described among community-dwelling patients of an age similar to our group, a mortality rate was 28.9% at the first year with a global comorbidity index of 2.1, whereas the mortality rate of our sample was 4.9% at the first year and the comorbidity index was 1.4. Interestingly, it should be noted that in this study, the effect of multimorbidity on mortality persisted after adjusting for functionality, unlike other studies.7,27 Probably, our results, which include ADL, support that disability in basic ADL was a less-sensitive predictor of functional decline than instrumental activities28 – as it was utilized in the studies by Marengoni et al and Wong et al.23,25 Furthermore, the effect of disability could modulate the effect of multimorbidity on mortality when the long disease states produce a period of disability along with other conditions, such as loneliness, dependence on a caregiver, and difficulties of access to the care system before death, which were not reflected in the analyses and would influence the main outcome.
Although little is known about the effect of multimorbidity as specific combinations,6 this study found a mortality risk of 4.2 in a specific combination of three diseases at 3 years and, in turn, a mortality risk of 3.2 at the 5-year follow-up, among the oldest old. Similarly, other groups, such as the Incalzi et al29 community study in people aged 78 years and the Christakis and Escarce30 study among 76-year-old critically ill patients, reported a consistent multimorbidity effect on mortality. Furthermore, in this study, AF was the most common arrhythmia in the elderly with a 2.4 global mortality risk, and although CKD by itself was not significant as an individual predictor, in co-occurrence, with AF the mortality risk increased to 3.8. This is important because, due to shared atherosclerotic-structural vascular disease,31 these two conditions impose a significant burden upon health in this group of octogenarians. Moreover, in turn, visual impairment was found as another important mortality predictor with a rate of risk of 4.2, when co-occurring with these conditions, probably as a result of multiple associated geriatric conditions. It should be suggested that in the elderly, an extended assessment of multimorbidity including sensorial capacities is needed.32 In addition, in this group of octogenarians, anemia, described as a predictor of mortality in the oldest old,33 showed a mortality risk of 2.8 in combination with the earlier conditions. Therefore, this finding and the described association between anemia and left-ventricular hypertrophy or progressive loss of kidney function seem to reinforce the idea that anemia could act as a mortality multiplier, especially in patients with CKD, cardiovascular disease, and those with both.34
Regarding the follow-up at 5 years of the cohort, this study revealed that the co-occurrence of specific pairs of diseases in the same individual has an important multiplying or dampening effect on the mortality outcome. Therefore, in our group, the individual disease of cancer has a mortality risk of 1.8. In co-occurrence of cancer with CKD and hypertension, this combination led to a mortality risk of 3.2, which, in turn, is higher than the individual disease expected risk. Similarly, in the study by Newschaffer et al35 for women affected with breast cancer, the effect of comorbidity and cancer showed a higher mortality rate than expected. However, dementia and COPD have an individual described mortality risk of 2.0 and 1.8, respectively, and yet in the subsequent analysis they do not appear in any significant multimorbidity combination, which shows a dampening effect on mortality. For all of the above, this study highlights that, although there has been a downward trend in cancer death rates in elderly people over the last two decades,36 if malignancy co-occurred with other specific diseases in the oldest old subjects, it might to be to targeted, especially because of its synergistic effect on mortality. Furthermore, at 3 years of cardiovascular diseases represented by combinations including AF appeared as one of the most important causes of death, despite at 5 years of malignancy and metabolic diseases, such as anemia and CKD, were the most important causes. Further population-based studies of the elderly are required to corroborate these findings. Finally, the association of the pattern of cardiovascular risk factors, such as hypertension and dyslipidemia, with mortality in this group of very old patients was not surprising, due to their effect as a primary reason for the overall cardiovascular death rates for heart disease and stroke.37,38 Therefore, the notion of a complex cumulative effect of health problems remains critical to the care of many people, and the development of more appropriate guidelines for use in multimorbid persons is required in order to better target interventions,39 especially in elderly patients.
The main strength of the Octabaix study is the use of a community-based sample of the same age group. This sample provides a representative range of the socioeconomic characteristics of older residents in our area, all of whom were registered with a general practitioner and benefitted from a full range of health facilities. However, this strength might also constitute a weakness, since it limits the generalizability of its findings to other populations. Indeed, this study does have several limitations that should be acknowledged. First, our observational cohort study design can provide evidence of predictive association but not of cause of mortality. Another limitation is that we only assessed the occurrence of disease without taking into account its severity or stage, suggesting that further studies should be implemented.
Conclusion
In conclusion, multimorbidity, as specific combinations, is associated with mortality in the oldest old. The multimorbidity pattern of AF, CKD, and visual impairment at 3-year follow-up and the pattern of hypertension, CKD, and malignancy at 5-year follow-up are the strongest predictors of mortality for all causes. Furthermore, cancer has a synergistic effect on mortality and may lead specific disease combinations to have more than an additive risk on the effect of death. These findings contribute to better understanding the needed multimorbidity approach in clinical practice rather than the individual diseases approach, as well as to design future studies of multimorbidity patterns rather than the total account of morbidities, in order to reduce mortality rates of very elderly people, a group that lacks information.
Acknowledgments
The project received a research grant from the Carlos III Institute of Health, Ministry of Economy and Competitiveness (Spain), awarded on the 2009 call under the Health Strategy Action 2013–2016, within the National Research Program oriented to Societal Challenges, within the Technical, Scientific and Innovation Research National Plan 2013–2016, with reference PS09/00552, cofunded with European Union ERDF funds (European Regional Development Fund).
Members of the Octabaix study: T Badia, MD (ABS Martorell Centre), C Fernández, Nurse (CAP Rambla), A Gil, MD (ABS Sant Andreu de la Barca), C Llopart, Social worker (ABS Sant Andreu de la Barca), MJ Megido, Nurse (ABS Just Oliveras), M Sarró, MD (CAP Florida Nord), and A Tobella, MD (ABS Martorell Rural).
Author contributions
AF and FF helped in conception, design, and preparation of manuscript. HS carried out statistical support and drafting of the manuscript. JA contributed to drafting of the manuscript and review of manuscript. GP helped in manuscript drafting and reviewing. Octabaix Study Group collected data and reviewed the manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. | ||
Tinetti ME, Fried T. The end of the disease era. Am J Med. 2004;116(3):179–185. | ||
Guiding principles for the care of older adults with multimorbidity: an approach for clinicians: American geriatrics society expert panel on the care of older adults with multimorbidity. J Am Geriatr Soc. 2012;60(10):E1–E25. | ||
Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35:75–83. | ||
Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, van den Bos GA. Causes and consequences of comorbidity: a review. J Clin Epidemiol. 2001;54(7):661–674. | ||
Quiñones AR, Markwardt S, Botoseneanu A. Multimorbidity combinations and disability in older adults. J Gerontol A Biol Sci Med Sci. 2016;71(6):823–830. | ||
St John PD, Tyas SL, Menec V, Tate R. Multimorbidity, disability, and mortality in community-dwelling older adults. Can Fam Physician. 2014;60(5):e272–e280. | ||
Fortin M, Stewart M, Poitras ME, Almirall J, Maddocks H. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. 2012;10(2):142–151. | ||
Menotti A, Mulder I, Nissinen A, Giampaoli S, Feskens EJ, Kromhout D. Prevalence of morbidity and multimorbidity in elderly male populations and their impact on 10-year all-cause mortality: the FINE study (Finland, Italy, Netherlands Elderly). J Clin Epidemiol. 2001;54(7):680–686. | ||
Byles JE, D’Este C, Parkinson L, O’Connell R, Treloar C. Single index of multimorbidity did not predict multiple outcomes. J Clin Epidemiol. 2005;58(10):997–1005. | ||
Formiga F, Ferrer A, Padros G, Montero A, Gimenez-Argente C, Corbella X. Evidence of functional declining and global comorbidity measured at baseline proved to be the strongest predictors for long-term death in elderly community residents aged 85 years: a 5-year follow-up evaluation, the OCTABAIX study. Clin Interv Aging. 2016;11:437–444. | ||
Landi F, Liperoti R, Russo A, et al. Disability, more than multimorbidity, was predictive of mortality among older persons aged 80 years and older. J Clin Epidemiol. 2010;63(7):752–759. | ||
Vogeli C, Shields AE, Lee TA, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. 2007;22(Suppl 3):391–395. | ||
Holden L, Scuffham PA, Hilton MF, Muspratt A, Whiteford HA. Patterns of multimorbidity in working Australians. Popul Health Metr. 2011;9(1):15. | ||
Ferrer A, Formiga F, Sanz H, de Vries OJ, Badia T, Pujol R. Multifactorial assessment and targeted intervention to reduce falls among the oldest-old: a randomized controlled trial. Clin Interv Aging. 2014;9:383–393. | ||
Formiga F, Ferrer A, Sanz H, et al; Octabaix study members. Patterns of comorbidity and multimorbidity in the oldest old: the octabaix study. Eur J Intern Med. 2013;24(1):40–44. | ||
Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. A simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Md State Med J. 1965;14:61–65. | ||
Lobo A, Saz P, Marcos G, et al. Revalidación y normalización del Mini-Examen Cognoscitivo (primera versión en castellano del Mini mental Status Examination) en la población general geriátrica. Med Clin (Barc). 1999;112:767–774. | ||
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. | ||
Guigoz Y. The mini nutritional assessment (MNA) review of the literature-What does it tell us? J Nutr Health Aging. 2006;10(6):466–485. | ||
Lee SJ, Lindquist K, Segal MR, Covinsky KE. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295(7):801–808. | ||
Walter LC, Brand RJ, Counsell SR, et al. Development and validation of a prognostic index for 1-year mortality in older adults after hospitalization. JAMA. 2001;285:2987–2994. | ||
Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10:430–439. | ||
Bowling CB, Muntner P. Epidemiology of chronic kidney disease among older adults: a focus on the oldest old. J Gerontol A Biol Sci Med Sci. 2012;67:1379–1386. | ||
Wong SYS, Mercer SW, Woo J, Leung J. The influence of multi-morbidity and self-reported socio-economic standing on the prevalence of depression in an elderly Hong Kong population. BMC Public Health. 2008;8:119. | ||
Gené J, Borràs A, Contel JC, et al. Predictors of mortality among elderly dependent home care patients. BMC Health Serv Res. 2013;13:316. | ||
Marengoni A, von Strauss E, Rizzuto D, Winblad B, Fratiglioni L. The impact of chronic multimorbidity and disability on functional decline and survival in elderly persons. A community-based, longitudinal study. J Intern Med. 2009;265:288–295. | ||
Spector WD, Katz S, Murphy JB, Fulton JP. The hierarchical relationship between activities of daily living and instrumental activities of daily living. J Chronic Dis. 1987;40:481–489. | ||
Incalzi RA, Capparella O, Gemma A, et al. The interaction between age and comorbidity contributes to predicting the mortality of geriatric patients in the acute-care hospital. J Intern Med. 1997;242:291–298. | ||
Christakis NA, Escarce JJ. Survival of Medicare patients after enrollment in hospice programs. N Engl J Med. 1996;335:172–178. | ||
de Ruijter W, Westendorp RG, Macfarlane PW, Jukema JW, Assendelft WJ, Gussekloo J. The routine electrocardiogram for cardiovascular risk stratification in old age: the Leiden 85-plus study. J Am Geriatr Soc. 2007;55:872–877. | ||
Crews JE, Campbell VA. Vision impairment and hearing loss among community-dwelling older Americans: implications for health and functioning. Am J Public Health. 2004;94:823–829. | ||
den Elzen WP, Willems JM, Westendorp RG, de Craen AJ, Assendelft WJ, Gussekloo J. Effect of anemia and comorbidity on functional status and mortality in old age: results from the Leiden 85-plus study. CMAJ. 2009;181:151–157. | ||
McCullough PA, Lepor NE. The deadly triangle of anemia, renal insufficiency, and cardiovascular disease: implications for prognosis and treatment. Rev Cardiovasc Med. 2005;6:1–10. | ||
Newschaffer CJ, Bush TL, Penberthy LE, Bellantoni M, Helzlsour K, Diener-West M. Does comorbid disease interact with cancer? An epidemiologic analysis of mortality in a cohort of elderly breast cancer patients. J Gerontol A Biol Sci Med Sci. 1998;53:M372–M378. | ||
Gruber K. Disparities in cancer mortality for elderly poor in the USA. Lancet Oncol. 2015;16:e431. | ||
Diederichs C, Berger K, Bartels DB. The measurement of multiple chronic diseases – a systematic review on existing multimorbidity indices. J Gerontol A Biol Sci Med Sci. 2011;66:301–311. | ||
Postmus I, Deelen J, Sedaghat S, et al. LDL cholesterol still a problem in old age? A Mendelian randomization study. Int J Epidemiol. 2015;44:604–612. | ||
Smith SM, Soubhi H, Fortin M, Hudon C, O’Dowd T. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev Rev. 2012;18(4):CD006560. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




