Back to Journals » Clinical Interventions in Aging » Volume 14
Modified frailty as a novel factor in predicting the response to cardiac resynchronization in the elderly population
Authors Mlynarska A , Mlynarski R , Marcisz C, Golba KS
Received 6 November 2018
Accepted for publication 12 January 2019
Published 25 February 2019 Volume 2019:14 Pages 437—443
DOI https://doi.org/10.2147/CIA.S193577
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Agnieszka Mlynarska,1,2 Rafal Mlynarski,2,3 Czeslaw Marcisz,1 Krzysztof S Golba2,3
1Department of Gerontology and Geriatric Nursing, School of Health Sciences, Medical University of Silesia, Katowice, Poland; 2Department of Electrocardiology, Upper Silesian Heart Centre, Katowice, Poland; 3Department of Electrocardiology and Heart Failure, School of Health Sciences, Medical University of Silesia, Katowice, Poland
Background: The response to cardiac resynchronization therapy (CRT) is an important element of the treatment of advanced heart failure, especially in the geriatric population. The aim of the study was to examine the impact of frailty syndrome on the response to treatment with CRT.
Methods: Two hundred and forty-six patients of 60 years or older (aged 73.35±6.95; 22.4% women) with an implanted CRT were included in this single-center prospective study. There was a 12-month follow-up. The Tilburg Frailty Indicator was used to determine frailty (5 or more points). The response to CRT was evaluated based on an analysis of clinical criteria.
Results: One hundred and sixty-nine of 246 (68.9%) patients were found to be clinical CRT responders. Frailty syndrome was recognized in 173 (70.32%). There were 63.0% responders in the frailty-affected group, whereas there were statistically more responders (79.5%) in the robust group (P=0.0116). In the logistic regression, frailty emerged as an independent predictor of the response to CRT (OR=0.81, 95% CI=0.71–0.92; P=0.0008). The area under the curve of the ROC curve for frailty in the responders to CRT was 0.62. The cut-off value for a designation of frailty was 6 (P=0.0014).
Conclusion: Frailty is a novel independent factor that can be used to predict the clinical response to CRT in the elderly population. Modifying the level of recognition in the Tilburg Frailty Indicator can improve the prediction of a response to CRT.
Keywords: cardiac resynchronization, frailty syndrome, heart failure, outcomes, responders
Introduction
Cardiac Resynchronization Therapy (CRT) is currently a recognized form of treatment for patients with advanced heart failure with an impaired left ventricular systolic function (Heart Failure with a reduced Ejection Fraction – HFrEF).1 In this method, leads are inserted into the left and right ventricles of the heart, as well as into the right atrium if necessary. CRT facilitates a coordinated, simultaneous pacing of the left ventricular and right ventricular. It improves cardiac systolic function, reduces the severity of the failure symptoms, improves the quality-of-life, and reduces morbidity and long-term mortality. However, analyses of the available data have shown that quite a large percentage of patients (25%–50%) do not respond to CRT satisfactorily. There are many predictors of a positive response to CRT, which can be divided into three main groups: the clinical characteristics of the patient, the advancement of the CRT device and the site that the left ventricular lead is implanted, and the programming of the CRT device and the care after the implantation. The effectiveness of CRT has been confirmed in many clinical trials such as COMPANION, CARE-HF, RAFT, REVERSE, and MADIT-CRT.2–5 Despite the positive results of these studies, a group of patients who have undergone CRT do not have significant advantages. Evaluating the effectiveness of resynchronization therapy is difficult due to the fact that it can be distorted by many factors. One of the limitations of assessing the effectiveness of CRT is the subjectivity of the evaluation.6 The response to cardiac resynchronization is also an important element in the treatment of advanced heart failure in the geriatric population.
Elderly patients comprise more than 80% of the population who have been diagnosed with heart failure. Due to the growing number of elderly individuals with diagnosed heart failure, a special approach to their treatment is required. This means that attention must be paid to geriatric conditions such as poor mobility, physical disabilities, and cognitive impairment. All of these factors significantly affect the course of heart failure and may also affect its treatment and prognosis in older patients. Due to its prognostic role, identifying the prevalence of frailty syndrome is crucial in patients with heart failure.7–9 Frailty syndrome is considered to be an important medical syndrome and is defined as a biological condition that is related to age, which is characterized by a decrease in the biological reserves due to the dysregulation of several physiological systems.10
The aim of the study was to examine the impact of frailty syndrome on the response to cardiac resynchronization therapy.
Methods
Two hundred and forty-six elderly patients (mean age=73.35±6.95) with diagnosed heart failure who were hospitalized due to the implantation of CRT-P (pacemaker type) and CRT-D (cardioverter-defibrillator type) resynchronizing systems were included into a single-center prospective study. Elderly is defined as individuals 60 years or older according to the United Nations. There was a 12-month follow-up.
The patients were qualified for CRT implantation according to the class I 2016 European Society of Cardiology guidelines for treating patients with heart failure: left bundle branch block (LBBB) with a QRS >130 ms, an ejection fraction (EF) ≤35% who were undergoing optimal pharmacological therapy.1 Patients with heart failure with a preserved ejection fraction regardless of their New York Heart Association Functional Classification (NYHA class) who had an indication for ventricular pacing and a high degree AV block were excluded. Patients with psychiatric disorders or a previous stroke, those who required intensive cardiac care, and individuals who submitted an incorrect or incomplete questionnaire were also excluded.
Definition of the response to CRT
We decided to use a predefined subjective definition for the cumulative response to cardiac resynchronization 12 months after the implantation of a CRT device. Our definition included:
- a reduction in the NYHA class by at least one
- heart failure hospitalization during follow-up
- a 10% absolute improvement in the base (calculated before CRT implantation) of the left ventricle ejection fraction, which was assessed by an experienced certified echocardiography specialist using the biplane Simpson method.
Patients who had an occurrence of each of the sub points were treated as responders. Patients who died due to the worsening of HF during the follow-up period or who had a heart transplant were considered to be non-responders.11,12
Response to CRT
The patients who were included into the study were divided into two groups depending on their response to resynchronization therapy:
- CRT responders – 169 (68.7%)
- CRT non-responders – 77 (31.3%).
A physical examination, anthropometric examination, and laboratory tests were also performed on all of the patients who were included into the study.
Frailty measurements
In order to diagnose the occurrence of frailty syndrome in all of the patients who were included into the study, the Polish language version of the Tilburg Frailty Indicator (TFI) questionnaire was used. The Tilburg Frailty Indicator is a 15-item tool, which uses a bio-psycho-social approach, and was selected to determine frailty before implantation. The TFI consists of two different parts: the first part includes the sociodemographic characteristics of a participant and the potential determinants of frailty, while the second part addresses the components of frailty, which are divided into three domains: the physical domain, the psychological domain, and the social domain. The TFI scale total score ranges from 0 to 15 – the higher the score, the higher the degree of one’s frailty. A score of 5 or more points was treated as frailty. The scale is highly reliable in identifying frailty patients. The Tilburg Frailty Indicator was answered by the patients themselves (as in the manual for this tool) before CRT implantation.13
Patients were divided into two groups according to the presence of frailty:
- Examined group – frailty affected patients.
- Control group – robust patients, with no presence of frailty symptoms.
The local ethics committee of the Medical University of Silesia approved the study protocol (approval no KNW/0022/KB1/13/17). The study protocol complied with the version of the Helsinki Convention that was current at the time the study was designed. All patients gave written informed consent and were aware of all their rights, including the right to withdraw from the study at any stage of the investigation.
Statistical analyses
In order to check the normality of the data distribution, the Shapiro-Wilk test was used. Comparisons of the two groups were performed using the Student’s t-test when there was a normal distribution of a variable in the groups being analyzed or using the Mann–Whitney test for distributions that were not normal. The chi2 test was also used for selected non-parametric data when applicable. Logistic regression analysis was also used to predict the factors of a CRT response. The results were considered to be significant at P-values <0.05. A receiver operating characteristic (ROC) curve analysis was used to evaluate the diagnostic performance of frailty syndrome. The area under the curve was calculated to reflect and to compare the predictive value of frailty syndrome in order to discriminate the patients who were CRT responders. All of the presented analyses were performed using MedCalc (MedCalc Software, Ostend, Belgium).
Results
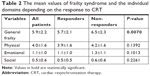
The characteristics of the patients who were included into the study are presented in Table 1. Of the 246, 169 (68.9%) patients were found to be clinical CRT responders. The gender-related difference was not significant: 70.68% men and 65.45% women (P=0.4581). Frailty syndrome was identified in 173 of the 246 (70.32%) patients. There were 109/173 (63.0%) responders in the frailty-affected group, whereas there were statistically more responders, 58/73 (79.5%), in the robust group; P=0.0116. Frailty syndrome occurred in 136/191 (71.20%) men. An effective response to resynchronization therapy – the CRT responders in the group of men identified 90/136 (66.17%) patients with diagnosed frailty syndrome and 45/55 (81.81%) in the robust patients. Men with no diagnosed frailty syndrome had a positive response to resynchronization therapy (P=0.0315) statistically more often. Among the women, frailty syndrome occurred in 37/55 (67.27%) patients. A positive response to the resynchronization therapy was found in 22/37 (59.45%) of the women with diagnosed frailty syndrome and 14/18 (77.78%) women in which frailty syndrome was not identified. Among the women, there was no statistically significant difference in the response to the resynchronization therapy that was dependent on the diagnosis of frailty syndrome (P=0.2991). The mean values of frailty syndrome and the individual domains that were dependent on the response to CRT are shown in Table 2.
In the logistic regression, frailty emerged as an independent predictor of the response to CRT (OR=0.81, 95% CI=0.71–0.92; P=0.0008). Frailty syndrome was also an independent predictor in the response to therapy in the group of patients who had an implanted CRT-D (OR=0.85, 95% CI=0.74–0.98; P=0.0478). Such a relationship was not observed in the group of patients with an implanted CRT-P system.
The ROC curves for frailty in the responders to CRT are presented in Figure 1. The area under the curve was 0.62 (95% CI=0.56–0.68). The cut-off value for a designation of frailty was 6 (P=0.0014). The ROC curves for frailty in the responders to CRT in the men’s group indicated that the area under the curve was 0.62 (95% CI=0.55–0.69). The cut-off value for a designation of frailty was ≤6 (P=0.0033). The ROC curves for frailty in the responders to CRT in the women’s group indicated that the area under the curve was 0.60 (95% CI=0.46–0.73). The cut-off value for a designation of frailty was ≤7; however, no values that were statistically significant (P=0.2260) were obtained. The gender-related ROC curves are presented graphically in Figures 2 and 3. During the 12-month follow-up period, 20.32% of the patients were rehospitalized. The incidence of rehospitalization during the 12-month follow-up was 26.62% in patients who had a frailty level ≥6 compared to 12.38% patients with a frailty level ≤6 (P=0.0075). The Kaplan–Meier curves showed that, depending on the number of TFI points that indicated a predisposition to a response to CRT, patients from the group with ≥6 points underwent re-hospitalization significantly more frequently during the 12-month follow-up compared to the patients who had fewer points on the TFI scale (P=0.0066). The detailed results, depending on the ROC score, are presented in Figure 4.
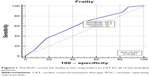  | Figure 1 The ROC curves for frailty in the responders to CRT for all of the included patients. |
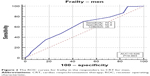  | Figure 2 The ROC curves for frailty in the responders to CRT for men. |
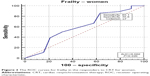  | Figure 3 The ROC curves for frailty in the responders to CRT for women. |
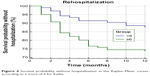  | Figure 4 Survival probability without hospitalization in the Kaplan–Meier curves according to a score of 6 for frailty. |
Discussion
CRT is a very effective therapy for patients with heart failure.14,15 However, 30% of patients do not benefit from CRT implantation, although the proportion of patients who does not respond to treatment varies depending on its definitions and criteria.16,17 The main goals of HF treatment should be to reduce the symptoms of HF, improve the quality-of-life, slow the progression of the disease, reduce the frequency of rehospitalizations and extend a patient’s life. At present, no consensus has been reached regarding the definition for the response to resynchronization therapy.18 Numerous studies have indicated that CRT reduces the morbidity and mortality of patients with heart failure. Decreasing the number of non-responders to CRT is essential for improving overall performance and lowering the benefit–risk ratio. The key is to identify non-responders according to a treatment plan that must be based on a universal definition of the response to CRT and must be carried out regularly.19,20 The response to cardiac resynchronization in octogenarians is also an important problem. Some experts believe that the advantages of CRT in this group may be limited. Meanwhile, there is some research that has documented that octogenarians may have similar advantages. Martens et al21 examined 686 patients, including 178 octogenarians (26%). A higher proportion of deaths that were not cardiovascular was observed in the octogenarians (74%) vs the younger patients (50%; P=0.022) with worsening heart failure rather than malignant tachyarrhythmia being the main cause of cardiac death. In this group, the survival rate was similar to the general age-matched population. Rickard et al,22 who examined 95 octogenarians with CRT, had similar results. In the end, the authors concluded that octogenarians with advanced heart failure have a reasonable mean survival time following CRT. All-cause mortality in this patient population was only modestly worse compared to the general octogenarian population. Verbrugge et al23 also examined the response to CRT in elderly patients (≥70 years) and octogenarians. The improvements in the reverse left ventricular remodeling and functional capacity after CRT are sustained at advanced age. However, the period of time until all-cause mortality or heart failure admission was similar, irrespective of age. All of these researches seem to confirm the fact that patients 80+ of age may be reasonable candidates for cardiac resynchronization, and that this therapy should not be contraindicated by the age of candidates.
After identifying the reason for the lack of response to therapy, the care of a patient must be individualized and comprehensive.18 Frailty syndrome has been identified as a risk factor for rehospitalization due to heart failure, and a routine comprehensive geriatric assessment at the time of the diagnosis of heart failure is recommended. Domingez Rodriguez et al24 showed that a diagnosis of frailty syndrome is an independent factor for rehospitalization due to HF decompensation in a 12-month observation. Similar observations were presented by Lupon et al,25 who showed that patients with frailty had a higher risk of mortality, hospitalizations, and a worsening quality-of-life in a 12-month observation. In our study, we have documented that patients who score points above a set cut-off point have a worse prognosis and no response to the therapy. This observation is important primarily in men, in whom the occurrence of frailty syndrome affected the response to CRT statistically and significantly. We demonstrated that frailty is a predictor of a lack of response to resynchronization therapy in patients over 60 years of age. Similar conclusions were presented by Kubala et al,26 who believed that patients with 10.25 or more points in their ONCODAGE G8 score had more frequent hospitalizations and a higher mortality. In our population, the cut-off was 6 points; however, Kubala et al26 assessed a frailty group using a questionnaire that is used with individuals suffering from oncological diseases, while, in our study, we used a questionnaire that was validated on a group of patients with heart failure and that has high reliability parameters.
In some research, women have shown a higher response to resynchronization therapy compared to men, and this was mainly associated with the age and condition of the respondents, which was not confirmed in our study. The worse response to CRT therapy in women may be due to the specific groups that were included in the study – women over 60 years of age as well as with the severity of frailty syndrome, which in diseases of the cardiovascular system are more common in women than in men. Although the cut-off point in women that predisposed them to a lack of response to CRT was higher, this result was not statistically significant. It seems that frailty syndrome may be one of the missing parameters that should be assessed during the qualification of patients for CRT implantation. An assessment of frailty may be a useful tool for selecting patients who will be responders of resynchronization therapy. We believe that patients with frailty syndrome should have an individualized and intensified plan of control visits and control of adherence to therapeutic recommendations.
Limitations
The response to CRT criteria varies depending on the research. There is a lack of a common, unified definition of a CRT response. The most common criteria that are used in the research are a reduction in the left ventricular systolic volume, an increase in the LVEF, an increase in peak VO2, an improvement of the NYHA class, an improvement in the quality-of-life, an improvement in six-minute walking distance, or a decrease in natriuretic peptides. We selected four of them to describe the response to CRT in the presented research. In our opinion, they are quite comparable and, from the point of view of the patient, describe the clinical and functional status relatively well, which is very important in elderly people. It is possible that changes in the definition of the CRT response could influence the results.
Conclusion
Frailty is a novel independent factor that can be used to predict the clinical response to CRT in the elderly population. Modifying the level of the identification of frailty syndrome in the Tilburg Frailty Indicator improved the prediction of the response to CRT.
Ethics approval
This study was approved by the Medical University of Silesia Ethical Committee (agreement KNW/0022/KB1/13/17).
Informed consent
All patients gave written informed consent and were aware of all their rights, including the right to withdraw from the study at any stage of the investigation.
Acknowledgment
An abstract of this paper was presented at the ACC.18 67th Annual Scientific Session and Expo as a poster presentation with interim findings.27
Disclosure
The authors report no conflicts of interest in this work.
References
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–21200. | ||
Cleland JG, Daubert JC, Erdmann E, et al. Longer-term effects of cardiac resynchronization therapy on mortality in heart failure (the CArdiac REsynchronization-Heart Failure (CARE-HF) trial extension phase). Eur Heart J. 2006;27(16):1928–1932. | ||
Tang AS, Wells GA, Talajic M, et al; Resynchronization-Defibrillation for Ambulatory Heart Failure Trial Investigators. Cardiac-resynchronization therapy for mild-to-moderate heart failure. N Engl J Med. 2010;363(25):2385–2395. | ||
Linde C, Gold MR, Abraham WT, et al. Long-term impact of cardiac resynchronization therapy in mild heart failure: 5-year results from the resynchronization reVErses remodeling in systolic left vEntricular dysfunction (reverse) study. Eur Heart J. 2013;34(33):2592–2599. | ||
Moss AJ, Hall WJ, Cannom DS, et al; MADIT-CRT Trial Investigators. Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med. 2009;361(14):1329–1338. | ||
Boidoł J, Średniawa B, Kowalski O, et al; Triple-Site Versus Standard Cardiac Resynchronisation Trial (TRUST CRT) Investigators. Many response criteria are poor predictors of outcomes after cardiac resynchronization therapy: validation using data from the randomized trial. Europace. 2013;15(6):835–844. | ||
Chaudhry SI, Wang Y, Gill TM, Krumholz HM. Geriatric conditions and subsequent mortality in older patients with heart failure. J Am Coll Cardiol. 2010;55(4):309–316. | ||
Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–397. | ||
Uchmanowicz I, Łoboz-Rudnicka M, Szeląg P, Jankowska-Polańska B, Łoboz-Grudzień K. Frailty in heart failure. Curr Heart Fail Rep. 2014;11(3):266–273. | ||
Rodríguez Mañas L. Determinants of frailty and longevity: are they the same ones? Nestle Nutr Inst Workshop Ser. 2015;83:29–39. | ||
Aarønæs M, Aakhus S, Aass H, et al. Assessment of response criteria to cardiac resynchronization therapy (CRT) and prediction of response. Scand Cardiovasc J. 2010;44(6):337–345. | ||
European Heart Rhythm Association (EHRA); European Society of Cardiology (ESC); Heart Rhythm Society, et al. 2012 EHRA/HRS expert consensus statement on cardiac resynchronization therapy in heart failure: implant and follow-up recommendations and management. Europace. 2012;14:1236–1286. | ||
Uchmanowicz I, Gobbens R, Jankowska-Polanska B, Łoboz-Rudnicka M, Manulik S, Łoboz-Grudzień K. Cross-cultural adaptation and reliability testing of the Tilburg frailty indicator for optimizing care of Polish patients with frailty syndrome. Clin Interv Aging. 2014;9:997–1001. | ||
Naqvi SY, Jawaid A, Goldenberg I, Kutyifa V. Non-response to cardiac resynchronization therapy. Curr Heart Fail Rep. 2018;15(5):315–321. | ||
European Society of Cardiology (ESC), European Heart Rhythm Association (EHRA), Brignole M, Auricchio A, Baron-Esquivias G, et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task Force on cardiac pacing and resynchronization therapy of the European Society of cardiology (ESC). Developed in collaboration with the European heart rhythm Association (EHRA). Eur Heart J. 2013;34(29):2281–2329. | ||
Auricchio A, Prinzen FW. Non-responders to cardiac resynchronization therapy: the magnitude of the problem and the issues. Circ J. 2011;75(3):521–527. | ||
Prinzen FW, Vernooy K, Auricchio A. Cardiac resynchronization therapy: state-of-the-art of current applications, guidelines, ongoing trials, and areas of controversy. Circulation. 2013;128(22):2407–2418. | ||
Daubert C, Behar N, Martins RP, Mabo P, Leclercq C. Avoiding non-responders to cardiac resynchronization therapy: a practical guide. Eur Heart J. 2017;38(19):1463–1472. | ||
Zareba W, Klein H, Cygankiewicz I, et al; MADIT-CRT Investigators. Effectiveness of cardiac resynchronization therapy by QRS morphology in the Multicenter Automatic Defibrillator Implantation Trial-Cardiac resynchronization therapy (MADIT-CRT). Circulation. 2011;123(10):1061–1072. | ||
Goldenberg I, Kutyifa V, Klein HU, et al. Survival with cardiac-resynchronization therapy in mild heart failure. N Engl J Med. 2014;370(18):1694–1701. | ||
Martens P, Verbrugge FH, Nijst P, Dupont M, Mullens W. Mode of death in octogenarians treated with cardiac resynchronization therapy. J Card Fail. 2016;22(12):970–977. | ||
Rickard J, Cheng A, Spragg D, et al. Survival in octogenarians undergoing cardiac resynchronization therapy compared to the general population. Pacing Clin Electrophysiol. 2014;37(6):740–744. | ||
Verbrugge FH, Dupont M, De Vusser P, et al. Response to cardiac resynchronization therapy in elderly patients (≥70 years) and octogenarians. Eur J Heart Fail. 2013;15(2):203–210. | ||
Dominguez-Rodriguez A, Abreu-Gonzalez P, Jimenez-Sosa A, et al. The impact of frailty in older patients with non-ischaemic cardiomyopathy after implantation of cardiac resynchronization therapy defibrillator. Europace. 2015;17(4):598–602. | ||
Lupón J, González B, Santaeugenia S, et al. Prognostic implication of frailty and depressive symptoms in an outpatient population with heart failure. Revista Española de Cardiología. 2008;61(8):835–842. English, Spanish | ||
Kubala M, Guédon-Moreau L, Anselme F, et al. Utility of Frailty Assessment for Elderly Patients Undergoing Cardiac Resynchronization Therapy. JACC Clin Electrophysiol. 2017;3(13):1523–1533. | ||
Mlynarska A, Mlynarski R, Doruchowska-Raczek A, Biernat J, Golba KS. Modified frailty as a novel factor to predict the response for cardiac resynchronization in the elderly population. J Am Coll Cardiol. 2018; 71(11 Suppl):936. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.