Back to Journals » Clinical Ophthalmology » Volume 13
Long-term stability of laser-demarcated macula-sparing rhegmatogenous retinal detachments
Authors Lin J, Sridhar J, Flynn HW Jr
Received 6 February 2019
Accepted for publication 4 April 2019
Published 19 June 2019 Volume 2019:13 Pages 1039—1041
DOI https://doi.org/10.2147/OPTH.S204366
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
James Lin, Jayanth Sridhar, Harry W Flynn Jr
Department of Ophthalmology, Bascom Palmer Eye Institute, Miller School of Medicine, University of Miami, Miami, FL, USA
Abstract: In a subset of patients presenting with rhegmatogenous retinal detachments, demarcation-laser photocoagulation is associated with long-term stability. Three patients with subclinical macula-sparing rhegmatogenous retinal detachments were treated with laser demarcation and had no progression over a follow-up of 3–10 years. One case had spontaneous resolution of retinal detachment after laser demarcation. Rather than observation or surgery, this alternative management strategy can be considered in some patients.
Keywords: demarcation-laser photocoagulation, asymptomatic retinal detachment
Introduction
Demarcation-laser photocoagulation (DLP) is a method that can be used to treat rhegmatogenous retinal detachments (RRDs) by forming a barrier possibly to reduce the chance of further extension of subretinal fluid.1–3 This method of management has been reported for macula-sparing RRD without visual field loss.2 It is less invasive than scleral buckling or vitrectomy, and has the advantage of being time-efficient and inexpensive, as it can be performed easily in the outpatient clinic.4 The authors present three patients in which DLP was used to barricade asymptomatic macular-sparing RRDs, and stability was achieved over follow-up of 3–10 years.
Case reports
Case 1
A 67-year-old male presented with an asymptomatic RRD of the right eye in 2015, was treated with DLP, and subsequently underwent cataract surgery. Three years later in 2018, he presented with worsening vision and distortion in the right eye, with best-corrected visual acuity (BCVA) of 20/200 OD and 20/20 OS. On dilated-fundus exam, there was a macular epiretinal membrane with drusen, as well as stability of the laser-barricaded shallow temporal RD extending from 7 to 11 o’clock, with no breaks evident (Figure 1). The patient underwent pars plana vitrectomy with membrane peeling, and subsequent BCVA was 20/30 1 month after surgery. The postoperative exam 1 month later showed stability of the laser-demarcated RD.
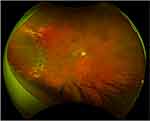 | Figure 1 Case 1: 3-year follow-up of temporal rhegmatogenous retinal detachment treated with demarcation-laser photocoagulation. |
Case 2
A 57-year-old male had had treatment for an asymptomatic chronic RRD of the right eye with DLP and 10 years of follow-up. Upon presentation, BCVA was 20/30 OD, 20/20 OS. Refraction was −6.50 Sph OD and −7.50 Sph OS. The patient was phakic, and on dilated exam there was posterior vitreous detachment with shallow temporal RD extending from 7 to 11 o’clock with no breaks evident, surrounded with laser barricade, as well as a mild epiretinal membrane. Three years later in 2018, the patient had stable vision, and the previous temporal RD in the right eye was noted to be spontaneously resolved, with remaining pigment changes (Figure 2).
 | Figure 2 Case 2: 10-year follow-up of temporal rhegmatogenous retinal detachment treated with demarcation-laser photocoagulation. |
Case 3
A 50-year-old male with a history of myopia after photorefractive keratectomy presented with a non-ischemic central retinal vein occlusion and cystoid macular edema in the left eye. The macular edema was being treated with intravitreal bevacizumab. The patient was phakic and noted to have posterior vitreous detachment with an asymptomatic temporal horseshoe tear at 2:30 and surrounding shallow subretinal fluid extending from 2 to 4 o’clock, for which he received laser demarcation. BCVA was 20/20 OD, 20/30 OS. Three years later, the laser-barricaded RD in the left eye had not progressed, and BCVA remained at 20/30 (Figure 3).
 | Figure 3 Case 3: 3-year follow-up of temporal rhegmatogenous retinal detachment treated with demarcation-laser photocoagulation. |
Discussion
While vitreoretinal surgery is used to manage nearly all macula-sparing RRDs, the use of DLP can be considered for a subset of these detachments, particularly those that are asymptomatic. DLP has been in use since 1968, when Okun and Cibis recommended photocoagulation for limited RDs defined by size.5 The described criteria included width at least twice but not greater than five times the diameter of the largest break, and less than 2 clock hours in size with the posterior extent not beyond the equator. On the other hand, some authors have recommended observation for subclinical or asymptomatic RRDs. In a study by Byer,6 only three of 18 asymptomatic detachments progressed during follow-up of 1–18 years, with none requiring surgery. Likewise, Brod et al7 reported a series of 29 of 31 eyes with asymptomatic RDs that did not progress over a mean 3.4 years' follow-up.
While macula-sparing RRDs can be asymptomatic, many RRDs with demarcation lines or caused by round holes may remain stable without progression. However, some studies have reported that even low-risk RRDs may progress.6,8,9 In particular, Al-Mohtaseb et al4 found that 38.5% of patients with symptomatic RDs treated with DLP required further intervention secondary to progression. Because laser photocoagulation enhances retinal adhesion, it may be an effective treatment for asymptomatic RDs.2,3 Vrabec and Baumal2 found DLP to be an effective treatment, with only one of 34 detachments (2.9%) progressing beyond the laser barrier, and progression was attributable to incomplete demarcation. The primary feature shared among detachments stabilized with DLP was a shallow, relatively tense appearance without associated corrugations. The three cases presented in the current series demonstrate the typical shallow, nonbullous RDs that remained stable over the long term. Interestingly, spontaneous resolution of RD, as seen in case 2, has been previously reported.6,10 One hypothesized mechanism for this would be detached posterior vitreous plugging of the retinal break.11
In conclusion, these three cases demonstrate the stability of DLP for asymptomatic macula-sparing RRDs, all of which were shallow and without corrugations. For this subset of RDs, DLP may be a viable option for patients uncomfortable with observation alone, who have limited access to health care, or who are not candidates for surgery because of systemic comorbidities.
Institutional review
This case series was deemed exempt from full review according to the University of Miami Institutional Review Board. Written informed consent was obtained from all patients, which included for the case details to be published.
Acknowledgment
This work was upported in part by an NIH core grant and an unrestricted grant from Research to Prevent Blindness, New York, NY.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Schepens CL. Subclinical retinal detachments. AMA Arch Ophthalmol. 1952;47(5):593–606.
2. Vrabec TR, Baumal CR. Demarcation laser photocoagulation of selected macula-sparing rhegmatogenous retinal detachments. Ophthalmology. 2000;107(6):1063–1067.
3. Yoon YH, Marmor MF. Rapid enhancement of retinal adhesion by laser photocoagulation. Ophthalmology. 1988;95(10):1385–1388.
4. Al-Mohtaseb Z, Heffez JL, Carvounis PE, Holz ER. LASER demarcation photocoagulation for rhegmatogenous retinal detachments. Eye (Lond). 2010;24(12):1772–1776. doi:10.1038/eye.2010.119
5. Okun EC, Cibis PA. Photocoagulation in “limited” retinal detachment and breaks without detachment. In: McPherson A, editor. New and Controversial Aspects of Retinal Detachment. New York: Harper and Row; 1968:164–172.
6. Byer NE. The natural history of asymptomatic retinal breaks. Ophthalmology. 1982;89(9):1033–1039.
7. Brod RD, Flynn HW
8. Byer NE. Long-term natural history of lattice degeneration of the retina. Ophthalmology. 1989;96(9):1396–1401; discussion 401–2.
9. Davis MD. Natural history of retinal breaks without detachment. Arch Ophthalmol. 1974;92(3):183–194.
10. Hwang JF, Chen SN. Demarcation laser photocoagulation of macular sparing retinal detachments in teenagers. Retina. 2008;28(10):1487–1492. doi:10.1097/IAE.0b013e318183570d
11. Lorenzo J, Capeans C, Suarez A, Pacheco P, Sánchez-Salorio M. Posterior vitreous findings in cases of spontaneous retinal reattachment. Ophthalmology. 2002;109(7):1251–1255.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
