Back to Journals » ClinicoEconomics and Outcomes Research » Volume 8
Long-term outcomes in chronic obstructive pulmonary disease patients: exploring the effects of inhalatory devices and their influence on the outcome
Received 29 September 2014
Accepted for publication 17 November 2014
Published 15 April 2016 Volume 2016:8 Pages 87—95
DOI https://doi.org/10.2147/CEOR.S75132
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Giorgio L Colombo
Valeria Fadda, Dario Maratea
Department of Pharmaceutical Sciences, University of Florence, Sesto Fiorentino, FI, Italy
Purpose: Numerous systematic reviews have examined the outcomes in patients with chronic obstructive pulmonary disease managed with different therapeutic strategies. However, no such studies have specifically focused on the effect of inhalation devices.
Methods: A standard PubMed search was carried out in which we identified all randomized placebo-controlled trials conducted in patients with moderate-to-severe or severe chronic obstructive pulmonary disease. The clinical end points were exacerbations rate, incidence of pneumonia, and mortality. Meta-regression was employed to assess the effect of the device. For the incidence of exacerbations, an equivalence analysis was also carried out.
Results: A total of 37 studies were analyzed. Four different devices were used across these trials (Respimat®, HandiHaler®, Diskus, and Turbuhaler®). Our meta-regression analysis failed to show any significant difference between devices with regard to exacerbation rate. Equivalence was shown for some comparisons (HandiHaler® vs Respimat®), but not for others. In analyzing mortality, Respimat® was shown to worsen this end point in comparison with Turbuhaler® and HandiHaler®. Moreover, Turbuhaler® showed a protective effect over Diskus in the incidence of pneumonia.
Conclusion: The results of our analysis represent the first attempt to explore the effect of the type of device on long-term outcomes. One important limitation was that most drugs were associated with one particular device, and so the effects of drugs and devices could not be reliably differentiated from one another.
Keywords: COPD, inhalation device, moderate-severe, meta-analysis, equivalence
Introduction
Chronic obstructive pulmonary disease (COPD) is the fourth leading cause of death in most industrialized countries and affects about three million people worldwide. COPD is not one single disease, but represents different chronic lung diseases that cause lung airflow limitations. The most common symptoms are breathlessness, excessive sputum production, and a chronic cough.1
Several therapeutic strategies are available for treating COPD and the effectiveness of the different approaches has been investigated by a large number of trials and numerous systematic reviews.2–9 On the other hand, different types of inhalers have been developed for the delivery of these agents (eg, Diskus/Accuhaler, Turbuhaler®, HandiHaler®, and Respimat®), but their role has not yet been fully investigated.
Despite the wide literature on this topic, no analysis has been specifically focused on whether the different devices can influence the clinical outcomes observed in these patients (eg, exacerbation rates or incidence of pneumonia). Some papers in this area have only investigated patients’ preferences or manageability,9–11 or the causal relationship between a single device (Respimat®) and mortality.12,13 However, further studies are clearly needed.
The goal of the present analysis is to summarize the overall evidence available on the therapeutic strategies used in COPD and to investigate the role of the different devices on hard outcomes. In particular, the primary objective of the analysis was to test whether or not the inhalation devices currently in use to deliver topical agents differ from one another in terms of clinical outcomes. Three end points were evaluated (exacerbation rates, mortality, and incidence of pneumonia). The following topical agents were examined: 1) long-acting muscarinic agonists (LAMAs) (tiotropium); 2) long acting beta antagonist (LABA) inhaled corticosteroids (ICS). The secondary objective of our study was to carry out a formal statistical test of equivalence (proof of no difference) between the different devices with regard to the end point of exacerbations.
Methods
Criteria of study eligibility for inclusion in meta-analyses and meta-regressions
Eligible studies included all placebo-controlled randomized controlled trials (RCTs) indexed in PubMed that evaluated topical pharmacological treatments in patients with moderate-to-severe or severe COPD.
Literature search
Our initial search on PubMed was conducted by combining the first index term focused on the disease condition (COPD OR chronic obstructive pulmonary disease) with the second index term focused on the pharmacological treatments (LABA OR long-acting beta agonist) OR (LAMA OR long-acting antimuscarinic) OR (ICS OR inhaled corticosteroid) along with a PubMed filter restricting the extraction to “systematic reviews” and/or “randomized controlled trials”. These searches were repeated using variants of these terms and supplemented by the analysis of the Cochrane Library.
Study selection and data extraction
Studies potentially suitable for our analysis were identified from the abstract and, when necessary, from full texts. Information on the end points was extracted in duplicate by VF and DM; differences were resolved by consensus.
Quality assessment
Two reviewers (VF and DM) assessed the risk of bias in included studies by determining the Jadad score.14 This method addresses three domains (randomization, blinding of participants and personnel, and incomplete outcome data) and generates a score on a scale from 0 to 5.
Data analysis
Our analyses were separately carried out on each of the clinical end points under examination. Each of these analyses was divided into two steps: 1) traditional pair-wise meta-analysis, in which treated patients were compared with controls given placebo according to the design of the original RCTs, and of the clinical end point concerned, and 2) meta-regression, in which we tested whether the type of device, handled as a covariate, had any influence on the clinical end points. Three clinical end points were analyzed: exacerbation rate, mortality, and incidence of pneumonia; all of these end points were dichotomous.
Step 1
Our pair-wise meta-analyses were stratified according to the type of device and were therefore performed in the form of subgroup meta-analyses. The model was a random-effect model implemented according to the Mantel–Haenszel method. All comparisons were expressed as relative risk (RR) along with the respective 95% confidence intervals (CIs). Heterogeneity was quantified using the I2 statistic test. The statistical computer program used for this purpose was the Open Meta-Analyst (OMA) software (version 4.16.12; Tufts University, Medford, MA, USA.
Step 2
For each of the three clinical end points, a meta-regression analysis was carried out to investigate whether or not the specific devices had any influence on the end point under examination. Standard techniques of meta-regression15 were used. Also in this case, the OMA software was employed for all statistical calculations. The devices used for drug delivery in the various RCTs were handled as a covariate for the meta-regression analysis. Each of these meta-regressions was preceded by a standard pair-wise meta-analysis in which the pooled indexes of outcome, along with their 95% CIs, were separately estimated for the patient subgroups corresponding to the devices examined. All meta-regressions were performed by handling the type of device as a categorical covariate; in particular, in keeping with the design of our analysis, a single device was identified as a common comparator, in each meta-regression, for the remaining devices.
Finally, the data on exacerbation rates were incorporated into an analysis of equivalence that was aimed at testing whether the proof of no difference could be demonstrated for the pair-wise comparisons between specific devices. These equivalence tests were based on a well-known approach that, in a Forest plot, combines the traditional horizontal bars (indicating the 95% CI for individual RRs) with an equivalence interval that is between the lower and the upper margins of equivalence (see Ahn et al16 for further details). The margins employed for these analyses were directly obtained from the statistical power sections reported in the original RCTs. In this framework, the superiority of two-sided margins employed in the randomized trials were assumed to represent, at the same time, the margins of therapeutic equivalence.
Results
Literature search and study selection
Our initial search on PubMed retrieved 868 studies (including RCTs and systematic reviews). Among these publications, we identified 37 placebo-controlled RCTs that met all the criteria required for inclusion in our analysis. In the selection process that led us to identify the above 37 RCTs, some trials (N=28) were not included because no details were reported on the specific type of device; others (N=19) were excluded because the end points differed from those examined in our analysis (Figure 1). In regard of the assessment of methodological quality, the great majority of included studies (33 out of 37) were scored 4.
Four different devices were used in these RCTs, namely, Diskus/Accuhaler (eight trials), Turbuhaler® (ten trials), Respimat® (three trials), and HandiHaler® (16 trials). The devices Diskus/Accuhaler and Turbuhaler® were used to deliver fluticasone/salmeterol (eight trials) and budesonide/formoterol (ten trials), respectively; tiotropium (19 trials) was delivered using either Respimat® (three trials) or HandiHaler® (17 trials).
Meta-regression analysis
There were three meta-regression analyses that were investigated, namely, exacerbations, mortality, and pneumonia. In each analysis, a single device was identified as a common comparator for the remaining devices; whenever possible, Respimat® was the reference device; however, in a single analysis in which Respimat® was absent, Turbuhaler® was selected.
Exacerbations
A total of 24 studies were analyzed.17–40 Three therapeutic strategies vs placebo were compared: 1) fluticasone plus salmeterol; 2) budesonide plus formoterol; and 3) tiotropium. More importantly, four devices were used in these 24 RCTs.
The results of the subgroup meta-analysis focused on the different devices (Figure 2) showed the superiority of the agents delivered through the Respimat® and HandiHaler® devices. In contrast, the treatments delivered through the Diskus or the Turbuhaler® devices failed to show any significant difference in comparison with placebo. In the traditional meta-analysis, the pooled rate of exacerbations calculated across the whole series of 24 trials generated a RR of 0.86 (95% CI: 0.80–0.92). The heterogeneity among the studies was at I2=65%. The results of our meta-regression found no significant differences in exacerbations across different devices. However, these results might be biased by the high degree of heterogeneity found among the included studies.
Mortality
A total of 33 pairs of patient arms (included in 29 studies)17–29,31–34,36–48 were studied for each comparison; the number of paired groups exceeded the number of trials included in our analysis because, as shown in Figure 3, some studies contributed four or more patient arms to this meta-analysis. Active treatments were the same as in the previous analysis. According to the pair-wise meta-analysis, no device showed a significant protective effect on mortality in comparison to placebo. The Respimat® device showed a significant detrimental effect for this end point. For the mortality outcome, heterogeneity was absent (I2=0%). The results of our meta-regression showed a significant higher mortality rate of Respimat® over Turbuhaler® (RR =1.68 [95% CI: 1.13–2.48]; P=0.009) and HandiHaler® (RR =1.57 [95% CI: 1.08–2.28]; P=0.018), but not vs Dikus. No significant difference was found between Turbuhaler®, HandiHaler®, and Diskus.
Pneumonia
The information needed for our analysis was available from seven studies30,41,42,46–49 in which two devices were investigated. In the pair-wise meta-analysis, Turbuhaler® did not affect pneumonia (Figure 4). This end point was instead significantly worsened in the patient groups treated with Diskus. In the latter case, heterogeneity was at I2=43%. Finally, our meta-regression found a significant difference favoring Turbuhaler® as compared with Diskus (RR =0.55; 95% CI: 0.31–0.99; P=0.049).
Equivalence analysis
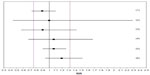
The secondary objective of our analysis was to test equivalence between devices according to the end point of exacerbations. Since all comparisons were based on RR, the lower and upper margins for equivalence were set, respectively, at RR =0.76 and RR =1.32 in keeping with the assumptions previously employed in the trial by Calverley et al26 (in which budesonide/formoterol, either alone or in combination, was compared to placebo). According to the design of our meta-regression, all values of RR that were firstly introduced in our equivalence testing relied on Respimat® as common comparator for the other devices. Hence, three values of RR (HandiHaler® vs Respimat®, Turbuhaler® vs Respimat®, and Diskus vs Respimat®) were directly derived from the results of meta-regression. Then, the values of RR for the three remaining comparisons (HandiHaler® vs Turbuhaler®, HandilHaler® vs Diskus, and Turbulaher® vs Diskus) were determined by changing the reference device; finally, these values were incorporated into the equivalence analysis (Figure S1).
The results of our equivalence testing are presented in the Forest plot shown in Figure 5. According to the prespecified margins, equivalence was demonstrated for the comparison of HandiHaler® vs Respimat®, but not for the other five comparisons.
Discussion
To our knowledge, the previous literature on the effect of inhalation devices in COPD includes only a single study in which different inhalation devices were compared using FEV1 as the outcome measure.50 Brocklebank et al evaluated terbutaline, salbutamol, and ipratropium bromide delivered through hand-held vs nebulizers; however, their results failed to show any significant difference among the devices.
The first RCT, specifically designed in terms of sample size to test the noninferiority between two devices delivering tiotropium, was carried out by Wise et al12 in 2013 (with 17,135 patients randomized to either Respimat® or HandiHaler®). The results of this trial, based on the risk of exacerbations, confirmed the noninferiority target for the risk of death in using Respimat® and failed to show any superiority of Respimat® over HandiHaler®. The trial was undertaken because some systematic reviews had shown an increased risk of death with Respimat® in comparison with HandiHaler®.3,52,53
Overall, the results of our analysis were consistent with those reported in previous systematic reviews on this topic.3,11,13 In fact, we confirmed a significant increase in mortality among patients using Respimat® vs those using HandiHaler®. This conclusion is supported by the results of our meta-regression and by the low degree of heterogeneity found among the included studies. Regarding exacerbations, our analysis confirmed the nonsignificant difference among these two devices and, more importantly, provided the proof of their equivalence. Interestingly enough, our results showed that the differences between HandiHaler®, Respimat®, and Diskus failed to remain within the prespecified margins of equivalence. Finally, since no data from RCTs were available for Diskus and Turbuhaler® devices, our results can only be considered a first step for further insights.
Unfortunately, there was one important drawback limiting the scientific value of our analysis. In fact, a great majority of individual drugs were associated with one particular device; therefore, an unavoidable consequence was that the effects of drugs and devices could not be reliably differentiated from one another. In other words, the effects of the therapeutic interventions in our analysis were attributed to the devices, but these should actually be attributed to the device/drug combinations. While this may be merely a question of wording, in our view, the results of our analysis keep a large part of their interest because they provided a comprehensive and updated picture of the current therapeutic evidence.
As a clue in future perspective, to correctly quantify the device effect, specific studies would be needed, for example, in which tiotropium is delivered by HandiHaler®, Turbuhaler®, or Diskus, as well as studies where a LABA is also delivered by these three devices. At present, no such trials are available, and so the effects of devices cannot be separated from those of the inhaled drugs.
Conclusion
Conclusive results on this issue will require that RCTs are specifically designed to evaluate the causal effect of individual devices on hard outcomes. Meanwhile, our study can be considered a first step forward in this controversial area.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines; 2013. Available from: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2013_Feb20.pdf. Accessed December 30, 2013. | |
Chong J, Karner C, Poole P. Tiotropium versus long-acting beta-agonists for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;9:CD009157. | |
Karner C, Chong J, Poole P. Tiotropium versus placebo for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;7: CD009285. | |
Nannini LJ, Poole P, Milan SJ, Holmes R, Normansell R. Combined corticosteroidand long-acting beta2-agonist in one inhaler versus placebo for chronicobstructive pulmonary disease. Cochrane Database Syst Rev. 2013;10(11):CD003794. | |
Nannini LJ, Lasserson TJ, Poole P. Combined corticosteroid and long-acting beta(2)-agonist in one inhaler versus long-acting beta(2)-agonists for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;9:CD006829. | |
Spencer S, Karner C, Cates CJ, Evans DJ. Inhaled corticosteroids versus long-acting beta(2)-agonists for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2011;7(12):CD007033. | |
Kew KM, Dias S, Cates CJ. Long-acting inhaled therapy (beta-agonists, anticholinergics and steroids) for COPD: a network meta-analysis. Cochrane Database Syst Rev. 2014;3:CD010844. | |
Yang IA, Clarke MS, Sim EH, Fong KM. Inhaled corticosteroids for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;7:CD002991. | |
Lavorini F, Fontana GA. Inhaler technique and patient’s preference for dry powder inhaler devices. Expert Opin Drug Deliv. 2014; 11(1):1–3. | |
van der Palen J, van der Valk P, Goosens M, Groothuis-Oudshoorn K, Brusse-Keizer M. A randomised cross-over trial investigating the ease of use and preference of two dry powder inhalers in patients with asthma or chronic obstructive pulmonary disease. Expert Opin Drug Deliv. 2013;10(9):1171–1178. | |
Dong YH, Lin HH, Shau WY, Wu YC, Chang CH, Lai MS. Comparative safety of inhaled medications in patients with chronic obstructive pulmonary disease: systematic review and mixed treatment comparison meta-analysis of randomised controlled trials. Thorax. 2013;68(1):48–56. | |
Wise RA, Anzueto A, Cotton D, et al; TIOSPIR Investigators. Tiotropium Respimat inhaler and the risk of death in COPD. N Engl J Med. 2013;369(16):1491–1501. | |
Singh S, Loke YK, Enright PL, Furberg CD. Mortality associated with tiotropium mist inhaler in patients with chronic obstructive pulmonary disease: systematic review and meta-analysis of randomised controlled trials. BMJ. 2011;342:d3215. | |
Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. | |
Agarwal R, Aggarwal AN, Gupta D, Jindal SK. Inhaled corticosteroids vs placebo for preventing COPD exacerbations: a systematic review and metaregression of randomized controlled trials. Chest. 2010;137(2):318–325. | |
Ahn S, Park SH, Lee KH. How to demonstrate similarity by using noninferiority and equivalence statistical testing in radiology research. Radiology. 2013;267(2):328–338. | |
Bateman ED, Tashkin D, Siafakas N, et al. A one-year trial of tiotropium Respimat plus usual therapy in COPD patients. Respir Med. 2010; 104(10):1460–1472. | |
Bateman E, Singh D, Smith D, et al. Efficacy and safety of tiotropium Respimat SMI in COPD in two 1-year randomized studies. Int J Chron Obstruct Pulmon Dis. 2010;5:197–208. | |
Beeh KM, Beier J, Buhl R, et al; ATEM-Studiengruppe. Wirksamkeit von Tiotropiumbromid (Spiriva®) bei verschiedenen Schweregraden der chronisch-obstruktiven Lungenerkrankung (COPD) [Efficacy of tiotropium bromide (Spiriva) in patients with chronic-obstructive pulmonary disease (COPD) of different severities]. Pneumologie. 2006; 60(6):341–346. German. | |
Bogdan MA, Aizawa H, Fukuchi Y, Mishima M, Nishimura M, Ichinose M. Efficacy and safety of inhaled formoterol 4.5 and 9 μg twice daily in Japanese and European COPD patients: phase III study results. BMC Pulm Med. 2011;11:51. | |
Brusasco V, Hodder R, Miravitlles M, Korducki L, Towse L, Kesten S. Health outcomes following treatment for six months with once daily tiotropium compared with twice daily salmeterol in patients with COPD. Thorax. 2003;58(5):399–404. | |
Campbell M, Eliraz A, Johansson G, et al. Formoterol for maintenance and as-needed treatment of chronic obstructive pulmonary disease. Respir Med. 2005;99(12):1511–1520. | |
Casaburi R, Mahler DA, Jones PW, et al. A long-term evaluation of once daily inhaled tiotropium in chronic obstructive pulmonary disease. Eur Respir J. 2002;19(2):217–224. | |
Chan CK, Maltais F, Sigouin C, Haddon JM, Ford GT, Group SS. A randomized controlled trial to assess the efficacy of tiotropium in Canadian patients with chronic obstructive pulmonary disease. Can Respir J. 2007;14(8):465–472. | |
Cooper CB, Abrazado M, Legg D, Kesten S. Development and implementation of treadmill exercise testing protocols in COPD. Int J Chron Obstruct Pulmon Dis. 2010;5:375–385. | |
Covelli H, Bhattacharya S, Cassino C, Conoscenti C, Kesten S. Absence of electrocardiographic findings and improved function with once-daily tiotropium in patients with chronic obstructive pulmonary disease. Pharmacotherapy. 2005;25(12):1708–1718. | |
Dusser D, Bravo ML, Lacono P. The effect of tiotropium on exacerbations and airflow in patients with COPD. Eur Respir J. 2006;27(3):547–555. | |
Freeman D, Lee A, Price D. Efficacy and safety of tiotropium in COPD patients in primary care-the SPiRiva Usual CarE (SPRUCE) study. Respir Res. 2007;8:45. | |
Johansson G, Lindberg A, Romberg K, Nordstrom L, Gerken F, Roquet A. Bronchodilator efficacy of tiotropium in patients with mild to moderate COPD. Prim Care Respir J. 2008;17(3):169–175. | |
Mahler DA, Wire P, Horstman D, et al. Effectiveness of fluticasone propionate and salmeterol combination delivered via the Diskus device in the treatment of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166(8):1084–1091. | |
Magnussen H, Bugnas B, Van Noord J, Schmidt P, Gerken F, Kesten S. Improvements with tiotropium in COPD patients with concomitant asthma. Respir Med. 2008;102(1):50–56. | |
Moita J, Bárbara C, Cardoso J, et al. Tiotropium improves FEV1 in patients with COPD irrespective of smoking status. Pulm Pharmacol Ther. 2008;21(1):146–151. | |
Niewoehner DE, Rice K, Cote C, et al. Prevention of exacerbations of chronic obstructive pulmonary disease with tiotropium, a once-daily inhaled anticholinergic bronchodilator: a randomized trial. Ann Intern Med. 2005;143(5):317–326. | |
Powrie DJ, Wilkinson TM, Donaldson GC, et al. Effect of tiotropium on sputum and serum inflammatory markers and exacerbations in COPD. Eur Respir J. 2007;30(3):472–478. | |
Rennard SI, Tashkin DP, McElhattan J, et al. Efficacy and tolerability of budesonide/formoterol in one hydrofluoroalkane pressurized metered-dose inhaler in patients with chronic obstructive pulmonary disease. Results from a 1-year randomized controlled clinical trial. Drugs. 2009; 69(5):549–565. | |
Szafranski W, Cukier A, Ramirez A, et al. Efficacy and safety of budesonide/formoterol in the management of chronic obstructive pulmonary disease. Eur Respir J. 2003;21(1):74–81. | |
Tashkin DP, Celli B, Senn S, et al; UPLIFT Study Investigators. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359(15):1543–1554. | |
Tonnel AB, Perez T, Grosbois JM, Verkindre C, Bravo ML, Brun M. Effect of tiotropium on health-related quality of life as a primary efficacy endpoint in COPD. Int J Chron Obstruct Pulmon Dis. 2008;3(2):301–310. | |
Troosters T, Weisman I, Dobbels F, Giardino N, Valluri SR. Assessing the impact of tiotropium on lung function and physical activity in GOLD Stage II COPD patients who are naive to maintenance respiratory therapy: a study protocol. Open Respir Med J. 2011;5:1–9. | |
Verkindre C, Bart F, Aguilaniu B, et al. The effect of tiotropium on hyperinflation and exercise capacity in chronic obstructive pulmonary disease. Respiration. 2006;73(4):420–427. | |
Calverley P, Pauwels R, Vestbo J, et al; TRial of Inhaled STeroids ANd long-acting beta2 agonists study group. Combined salmeterol and fluticasone in the treatment of chronic obstructive pulmonary disease: a randomised controlled trial. Lancet. 2003;361(9356):449–456. | |
Calverley PM, Bonsawat W, Cseke Z, Zhong N, Peterson S, Olsson H. Maintenance therapy with budesonide and formoterol in chronic obstructive pulmonary disease. Eur Respir J. 2003;22(6):912–919. | |
Hanania NA, Darken P, Horstman D, et al. The efficacy and safety of fluticasone propionate (250 micro g)/salmeterol (50 micro g) combined in the diskus inhaler for the treatment of COPD. Chest. 2003;124(3):834–843. | |
Pauwels RA, Löfdahl CG, Laitinen LA, et al. Long-term treatment with inhaled budesonide in persons with mild chronic obstructive pulmonary disease who continue smoking. European Respiratory Society Study on Chronic Obstructive Pulmonary Disease. N Engl J Med. 1999;340(25):1948–1953. | |
Tashkin DP, Rennard SI, Martin P, et al. Efficacy and safety of budesonide and formoterol in one pressurized metered-dose inhaler in patients with moderate to very severe chronic obstructive pulmonary disease: results of a 6-month randomized clinical trial. Drugs. 2008;68(14):1975–2000. | |
Calverley PM, Anderson JA, Celli B, et al; TORCH investigators. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356(8):775–789. | |
Vestbo J, Sorensen T, Lange P, Brix A, Torre P, Viskum K. Long-term effect of inhaled budesonide in mild and moderate chronic obstructive pulmonary disease: a randomised controlled trial. Lancet. 1999; 353(9167):1819–1823. | |
Barnes NC, Qiu YS, Pavord ID, et al; SCO30005 Study Group. Antiinflammatory effects of salmeterol/fluticasone propionate in chronic obstructive lung disease. Am J Respir Crit Care Med. 2006; 173(7):736–743. | |
Zheng J, Zhong N, Yang L, et al. The efficacy and safety of fluticasone propionate 500 mg/salmeterol 50 mg combined via diskus/accuhaler in Chinese patients with chronic obstructive pulmonary disease (COPD). Chest. 2006;130(4):182s. | |
Brocklebank D, Ram F, Wright J, et al. Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature. Health Technol Assess. 2001;5(26):1–149. | |
Voshaar T, Lapidus R, Maleki-Yazdi R et al. A randomized study of tiotropium Respimat Soft Mist inhaler vs. ipratropium pMDI in COPD. Respiratory Medicine. 2008;102(1):32–41. | |
Verkindre C, Bart F, Aguilaniu B, et al. The effect of tiotropium on hyperinflationand exercise capacity in chronic obstructive pulmonary disease. Respiration. 2006;73(4):420–427. | |
Mahler DA, Wire P, Horstman D et al. Effectiveness of fluticasone propionate and salmeterol combination delivered via the diskus device in the treatment of chronic obstructive pulmonary disease.American Journal of Respiratory Critical Care Medicine. 2002;166(8):1084–1091. |
Supplementary materials
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.