Back to Journals » Clinical Ophthalmology » Volume 9
Lead time for appointment and the no-show rate in an ophthalmology clinic
Authors McMullen M, Netland P
Received 3 February 2015
Accepted for publication 24 February 2015
Published 18 March 2015 Volume 2015:9 Pages 513—516
DOI https://doi.org/10.2147/OPTH.S82151
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Michael J McMullen, Peter A Netland
Department of Ophthalmology, University of Virginia School of Medicine, Charlottesville, VA, USA
Purpose: The purpose of this study was to determine if there is a correlation between the time in advance an appointment is scheduled and the no-show rate.
Methods: This was a cross-sectional study conducted in an outpatient ophthalmology clinic. Appointment data were analyzed for 51,529 ophthalmology appointments in the computerized scheduling database during a 12-month period.
Results: The average no-show rate was 21.7% and 6.6% for resident- and faculty-clinic, respectively (P<0.001). The no-show rate increased, and the likelihood an appointment would be kept decreased as the time in advance an appointment was scheduled increased. With a lead time for appointment of 0–2 weeks, the average no-show rate was 9.1% and 2.4% for the resident- and faculty-clinic, respectively. With a lead time for appointment of 6 months, the average no-show rate increased to 38.3% (P<0.001) and 6.9% (P<0.001) for the resident- and faculty-clinic, respectively. A predicted no-show rate model showed approximately 2% reduction of the no-show rate for 10% increase of the proportion of patients scheduled within 2 weeks, potentially reducing the no-show rate by nearly 60% with all appointments scheduled 0–2 weeks in advance.
Conclusion: Clinic no-show rate increased as appointment lead time increased. Predictive models suggest that the implementation of a short-term appointment scheduling strategy may reduce the overall clinic no-show rate, particularly in clinic populations with a high no-show rate.
Keywords: compliance, clinic scheduling, appointment time, appointment access, advance access, open access scheduling
Introduction
Minimizing the no-show rate and improving access to care are challenges faced by many entities in the health care provision and public health fields. Variability in the no-show rate generates difficulty in scheduling patients and patient resources effectively, increasing wait times, and reducing clinic efficiency. Effective strategies for creating a predictably low no-show rate may keep wait times low and increase clinic efficiency, thereby improving access to care. Short-term appointment scheduling strategies, such as “open access” and “advanced access,” have been shown to decrease the no-show rate and improve access to care, although the impact on clinical outcome is uncertain.1,2 While telephone reminders have been shown to improve ophthalmic follow-up adherence in the pediatric patient population,3,4 studies exploring the application of short-term appointments in the ophthalmology clinic are lacking. Our purpose was to evaluate the relationship between the time in advance an appointment is scheduled and the no-show rate.
Subjects and methods
This was a cross-sectional retrospective study that pooled appointment data contained within the computerized scheduling database at the University of Virginia Eye Clinic. Data for 51,529 appointments for a 12-month period were retrieved for both resident and faculty physician clinics, including twelve resident physician providers and twelve attending physician providers. Reminder phone calls (TeleVox Software, Mobile, Alabama, USA) and appointment reminder letters were sent to all patients prior to their appointments. Only individual physician clinics were considered, and generic subspecialty clinics with no assigned provider were excluded (3,144 appointments). Walk-in patients seen on the same day and patients seen over the weekend were excluded (1,730 appointments). The outcome of a given appointment had been coded in the scheduling database as attended, canceled, rescheduled, or no-show, and was recorded for all appointments meeting the inclusion criteria. Patients who were no-shows were contacted to reschedule appointments, but the reason for not keeping the initial appointment or whether they had been seen elsewhere was not assessed. Both initial and follow-up visits were combined and analyzed. We analyzed 46,655 appointments that met the inclusion criteria, including 14,066 and 32,589 appointments in the resident- and faculty-clinics, respectively.
For the purposes of this study, the lead time of an appointment was defined as the time between the scheduled appointment date and the date the appointment created in the computer system. Both variables were generated by the computerized scheduling database. The no-show rate was defined as the number of no-shows divided by the sum of the number of no-shows and the total number of appointments kept. Patients were scheduled with a maximum lead time of 12 months and 6 months in the faculty- and resident-clinic, respectively. No patient-specific identifying information was collected for the purposes of this study.
The predicted no-show rate model for the resident-clinic was calculated by fixing the percent of all appointments that were scheduled 0–2 weeks in advance and reducing the number of appointments for each of the other lead times proportionally. The known no-show rate for each lead time was then applied to the model distribution in order to calculate the overall predicted no-show rate as the percent of appointments scheduled 0–2 weeks in advance varied. Statistical analysis was performed using the comparison of proportions test (Z-test).
Results
At 6 months lead time for appointment, the likelihood that a given scheduled appointment was kept and not canceled, rescheduled, or resulted in a no-show, was 58.8% and 41.1% for faculty and resident patients, respectively (Figure 1). Appointments that were identified by the scheduling system as canceled or rescheduled were not counted as a no-show. The average no-show rate was 21.7% and 6.6% for resident patients and faculty patients, respectively (P<0.001). The daily no-show rate was higher and more variable in the resident clinic than the faculty clinic, with variances of 86.5% and 15.2%, respectively.
With a lead time for appointment of 0–2 weeks, the average no-show rate was 9.1% and 2.4% for the resident- and faculty-clinic, respectively. As shown in Figure 2, the no-show rate increased as the lead time increased. With a lead time of 6 months to appointment, the no-show rate was significantly greater compared with 0–2 weeks lead time, increasing to 38.3% (P<0.001) and 6.9% (P<0.001) at 6 months for resident and faculty patients, respectively. Subgroup analyses by sex and age showed similar results (data not shown). The trend toward increasing no-show rates continued in the faculty clinics, which included appointments up to 12 months.
The lead time model distribution predicted that the no-show rate in the resident clinic would decrease by 1.7% points for every 10% increment of appointments scheduled with 0–2 weeks lead time (Figure 3). According to this model, the no-show rate would be reduced in the resident clinic population by nearly 60% if all appointments were scheduled 0–2 weeks in advance.
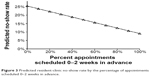  | Figure 3 Predicted resident-clinic no-show rate by the percentage of appointments scheduled 0–2 weeks in advance. |
Discussion
A high no-show rate at the clinic and variability in the no-show rate can lead to clinic over and under staffing, generate variable high wait times, reduce access to clinics, and decrease clinic efficiency. Our clinics and others will often target a threshold less than 5%–10%, in order to avoid disruption of clinic operations. In our study, the no-show rate increased as the appointment lead time increased. This correlation was much more pronounced in the resident clinic population, where the no-show rate was high and variable, than in the faculty clinic population, where the no-show rate was lower and less variable. We did not evaluate the reasons for the difference in the no-show rate between the resident- and faculty-clinics, which may have been related to socioeconomic or other variables of the patient population, including a higher rate of uninsured patients in the resident clinic compared with the faculty clinic.
In our clinic population, we use an automated voice phone message and letters as appointment reminder methods. The use of text message reminders have increased compliance by reducing nonattendance in pediatric cataract patients3 and in a general ophthalmology clinic.4 Text messaging systems have also been useful for improving follow-up for vision care in patients with diabetes.5 In an evidence-based review, mobile phone text message reminders were found to be effective in increasing attendance at health care appointments compared with no reminders, with similar results to voice telephone reminders.6 While using appointment reminder systems, a barrier encountered regarding compliance with ophthalmic follow-up care is the difficulty in contacting patients.7 In our study, we did not assess the impact of telephone reminders or letters on clinic no-show rate, although we assume the rate of no-shows would have been higher without these reminders.
The implementation of an “advanced or open access” style scheduling system whereby schedule slots are reserved for appointments with a 0–2-week lead time may reduce the overall clinic no-show rate,1,2 particularly in a clinic population with a high and variable no-show rate, such as our resident clinic. This may allow for a more predictable clinic flow and reduced periods of over and under staffing throughout the course of a clinic day, improving clinic efficiency, and reducing patient wait time. In this system, patients who need longer times to their appointment (for glaucoma or other chronic problems) can be scheduled at the appropriate time, but patients seeking earlier appointments may have improved access. Depending on the patient population, partial rather than complete use of open-access scheduling may avoid unfilled appointments. Our study data were analyzed in a model to explore the potential improved compliance with reduced lead time to appointment, supporting the concept of open access scheduling. Our results suggest that other methods of improving access to appointments, including adding providers or improving clinic efficiency, would likely reduce the no-show rate.
Limitations of this study include the fact that it was a cross-sectional study, and did not assess the effect of actual implementation of a short-term appointment scheduling strategy. The potential impact on clinical outcome and patient satisfaction was not considered, and we did not evaluate the influence of telephone or letter reminders on follow-up rates. We did not account for differences in follow-up rates for acute and chronic ophthalmic problems, the patient’s diagnosis, the time of day or week, and whether the appointment was physician- or patient-initiated. Moreover, we did not determine whether the longer times to appointment were for follow-up medical care or whether these patients could have been discharged from specialty clinic care.
Conclusion
Despite these limitations, our study showed that the no-show rate increased as the lead time increased, especially in the resident clinic. Predictive models suggest that same-day or “advanced access” scheduling strategy may reduce the no-show rate. Also, our results suggest that other improvements to access for appointments would be expected to reduce no-show rates in clinics.
Disclosure
The authors report no conflicts of interest in this work. The authors have no proprietary interest in this material.
References
Rose KD, Ross JS, Horwitz LI. Advanced access scheduling outcomes: a systematic review. Arch Intern Med. 2011;171:1150–1159. | ||
Degani N. Impact of advanced (open) access scheduling on patients with chronic diseases: an evidence-based analysis. Ont Health Technol Assess Ser. 2013;13(7):1–48. | ||
Lin H, Chen W, Luo L, et al. Effectiveness of a short message reminder in increasing compliance with pediatric cataract treatment: a randomized trial. Ophthalmology. 2012;119:2463–2470. | ||
Brannan SO, Dewar C, Taggerty L, Clark S. The effect of short messaging service text on non-attendance in a general ophthalmology clinic. Scott Med J. 2011;56:148–150. | ||
Zangalli CS, Murchison AP, Hale N, et al. An education- and telephone-based intervention to improve follow-up to vision care in patients with diabetes: a prospective, single-blinded, randomized trial. Am J Med Qual. Epub 2014 Sept 30. | ||
Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, Atun R, Car J. Mobile phone reminders for attendance at healthcare appointments. Cochrane Database Syst Rev. 2013;12:CD007458. | ||
Williams S, Wajda BN, Alvi R, McCauley C, Martinez-Helfman S, Levin AV. The challenges to ophthalmologic follow-up care in at-risk pediatric populations. J AAPOS. 2013;17:140–143. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.