Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 12
Knowledge And Attitudes Of Pharmacy Students Towards Pharmacogenomics Among Universities In Jordan And West Bank Of Palestine
Authors Jarrar Y , Mosleh R, Hawash M , Jarrar Q
Received 12 July 2019
Accepted for publication 9 September 2019
Published 7 October 2019 Volume 2019:12 Pages 247—255
DOI https://doi.org/10.2147/PGPM.S222705
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Yazun Jarrar,1 Rami Mosleh,2 Mohammed Hawash,2 Qais Jarrar3
1Department of Pharmacy, College of Pharmacy, Al-Zaytoonah University of Jordan, Amman, Jordan; 2Department of Pharmacy, Faculty of Medicine and Health Sciences, An-Najah National University, Nablus 00970, Palestine; 3Department of Pharmaceutical Science, Al-Isra’a University, Amman, Jordan
Correspondence: Yazun Jarrar
Department of Pharmacy, College of Pharmacy, Al-Zaytoonah University of Jordan, PO Box 130, Amman 11733, Jordan
Tel +9626795930283
Email [email protected]
Background: Testing by pharmacogenomics (PGx) aims to reduce the side-effects of medicines and to optimize therapy.
Aim: To ascertain the knowledge and attitudes towards PGx among pharmacy students in Jordan and West Bank of Palestine (WBP).
Methods: This cross-sectional study focused on pharmacy students from five universities in Jordan and WBP. Students were asked to answer an online survey comprising 30-closed ended questions measuring the knowledge and attitudes towards PGx.
Results: The total number of respondents to the questionnaire was 466. Most (96.1%) respondents knew that genetic variations can affect the drug response. Most students stated that the total number of lectures mentioning PGx was fewer than three. Most (>80%) respondents answered that they knew that human genetics can affect the response, inter-individual variation, and ethnic variations in the drug response. However, their knowledge about US Food and Drug Administration recommendations regarding PGx testing of commonly used drugs was weak. Also, 60.3% of respondents stated that the information they received about PGx was insufficient. Most (>92.7%) students wished to know more about PGx and believed that PGx is helpful in choosing the appropriate drug.
Conclusion: Pharmacy students had fair knowledge and good attitudes towards PGx. These factors could aid application of PGx in clinical practice in Jordan and WBP.
Keywords: pharmacogenomics, Jordan, West Bank of Palestine, knowledge, pharmacy students
Introduction
Pharmacogenomics (PGx) combines pharmacology and genomics to study the effect of genetic variants on the response to drug treatment.1 These genetic variants can influence the pharmacokinetics and interactions between the drug and molecular targets, thereby influencing the efficacy and unwanted side-effects induced by drug therapy.2
PGx aims to reduce the inter-individual variation in drug response by providing the appropriate drug at the correct dose.1 Use of the anticoagulant warfarin is an example of PGx testing. To avoid excessive bleeding, it is recommended to reduce the warfarin dose in patients with genetic variants, such as cytochrome (CYP) 2C9*2, *3 in Caucasians, CYP2C9*5, *6, *8, and *11 in Africans,3 and vitamin K epoxide reductase (VKORC1)-1639G>A.4
In addition to warfarin, the Food and Drug Administration (FDA) in the USA has provided clinical evidence supporting the importance of PGx testing in the labeling of many drugs.5 The Clinical PGx Implementation Consortium supported by the Pharmacogenomics Knowledge Base has developed a database for guiding clinicians to make pharmacotherapy decisions based on PGx information.6,7
However, PGx testing is not practiced widely in pharmacotherapy. One of the major barriers against implementation of PGx in clinical practice is the weak knowledge of PGx among medical-health professionals (including pharmacists).8 Therefore, the emergence of developing medical education on PGx has been highlighted. The International Society of Pharmacogenomics recommends ≥4 credit ours of PGx teaching to be offered to medical students.9
In the USA, several pharmacy training programs have implemented PGx in their curricula after the American Council on Pharmacy Accreditation set PGx as a requirement in the pharmacy curriculum.10 In Europe, PGx testing is implemented and practiced in clinical treatment.11 In addition, many universities and conferences have introduced educational programs in PGx, such as the summer schools of the European Society of Pharmacogenomics and Personalized Therapy (https://esptnet.eu/). In Bosnia and Herzegovina, Mahmutovic et al found positive attitudes towards genetic testing and “personalized” medicine in students enrolled in biomedicine courses.12
In developing countries, including Middle Eastern countries, PGx is not practiced in pharmacotherapy. Some studies have shown that Middle Eastern Arab populations have different genetic variants in their drug-metabolizing enzymes when compared with neighboring African, European and Asian populations.13,14
The first step in PGx awareness among medical professionals is to evaluate the current knowledge, attitudes, and practice toward PGx. Then, strategies can be put into place to improve the awareness and implementation of PGx in clinical treatment. Jarrar et al.15 investigated the perception of primary-health physicians in Jordan towards PGx. They found that internists had fair knowledge and a positive attitude toward PGx, but that it is not practiced due to a small number of validated PGx biomarkers and absence of simple and inexpensive PGx testing.
In Jordan and West Bank of Palestine (WBP), PGx testing is not practiced except in few cases (though medication errors and the prevalence of the adverse effects of drugs are high in these two countries).16,17 Pharmacists also have a major role in personalized pharmacotherapy in Jordan and WBP.18 However, PGx as a course is not included in the curricula of pharmacy schools, except in the Master of Science of Pharmacology at the University of Jordan (http://medicine.ju.edu.jo). Undergraduate pharmacy students may learn about some base concepts of PGx during pharmacology lecturers, but whether this knowledge is sufficient for implementation in clinical practice is questionable. Many pharmacy schools in Jordan and WBP provide two sub-programs: Pharmaceutical Science (PS) and Doctor of Pharmacy (DoP). The major difference between these two programs is that the DoP program provides more clinical courses with medical cases discussing the inter-individual variation in the drug response.19
The current knowledge and attitudes of pharmacy students toward PGx have not been evaluated in Middle Eastern Arab countries, a knowledge gap that we tried to fill in the present study.
Materials And Methods
This was a questionnaire-based cross-sectional study done online. The online copy is available as a Google™ document (https://docs.google.com/forms/d/1wO_ncL0mqHK9GbltHkLmAkm12PhEgCeRzXVkvXPTyJc/edit).
The response to the questionnaire was opened between 1 February and 29 April 2019. Eligible participants were students in PS or DoP from Jordan or WBP.
Nine-hundred students were asked to complete the online questionnaire, which was announced by the participant researchers in five universities: University of Jordan, Al-Zaytoonah University of Jordan, and Isra’a University in Jordan; An-Najah National University and Birzeit University in WBP.
The sample size was calculated according to the Daniel formula.20 The confidence interval (CI) was 95% and the significance level was set as α = 0.05. The expected prevalence in the sample with a characteristic of interest was 0.5. The total number of pharmacy students in the five universities was 6000. We estimated that a sample size of 360 was representative of the pharmacy students from Jordan and WBP. We recruited a sample size of 466 pharmacy students to increase the statistical robustness of our study. To ensure that we received >360 responses, we asked 900 students to complete the online questionnaire. In addition, the five universities selected are the top-ranked and major universities in Amman (capital of Jordan) and WBP. These universities have pharmaceutical academic programs and agreed to participate in our study. Among the selected universities, only the University of Jordan and An-Najah National University has two pharmacy programs: PS and DoP. In addition, the number of students in the PS program was twofold higher than the number of DoP students among University of Jordan and An-Najah National University. Accordingly, we estimated that the number of DoP students was ~15% of the total number of pharmacy students among the selected universities. Participation was voluntary and participants were informed that they had the option to not answer questions.
At the beginning of the questionnaire, there was an introductory section describing the purpose and objectives of our study. The survey consisted of 30 close-ended questions with answers of yes/no/I am not sure, categorized into four parts: (i) demographic characteristics of the student; (ii) basic and clinical PGx knowledge; (iii) exposure to PGx education; (iv) attitudes towards PGx. Some of these questions were adopted from similar studies that were undertaken in the USA,21 Zimbabwe22 and Bosnia and Herzegovina,12 with some modifications being made to make the questionnaire easier to understand by pharmacy students. In addition, we developed other questions which could help assessment of PGx knowledge, such as exposure to PGx education and PGx knowledge. “The effect of genetic variants on pharmacotherapy” was used instead of “PGx” in some of the questions to ensure that the participant dealt with the actual meaning rather than the terminology of PGx.
Before the questionnaire was sent to students, it was reviewed by three experts in pharmacogenomics and pharmacy education in Jordan and WBP. Then, the questionnaire was sent to 30 students (as a pilot study) for identification errors and misunderstood questions. The Cronbach alpha of PGx knowledge was 0.72, which indicated consistency in the questionnaire.
The study protocol was approved by the ethics committee of An-Najah National University (Institutional Review Board number 16-02-2019). In addition, the Ethics Committee of Al-Zaytoonah University approved the study to be conducted among pharmacy students in Jordan. All students provided written informed consent to be involved in the study.
Categorical variables (demographics and knowledge and attitudes about PGx) are expressed as frequencies and percentages. Descriptive analysis was undertaken using2 tests, Student’s t-tests and ANOVA (if needed). The Spearman test was used to calculate the correlation coefficient between the categorical data. Corresponding 95% CIs were calculated using a significance level of 5% for all statistical tests. Missing data were excluded from the analysis. Statistical analyses were carried out using SPSS v25 (IBM, Armonk, NY, USA).
Results
Demographic Data Of Participants
We received 466 responses to the online questionnaire (52%). One-hundred and ninety (40.8%) responses were from WBP and 262 (56.2%) responses were from Jordan. The highest number of responses was received from Al-Zaytoonah University of Jordan, 140 (30%), followed by 131 (28.1%) from An-Najah National University, 76 (16.3%) from University of Jordan, 59 (12.7%) from Isra’a University and 49 (10.5%) from Birzeit University (Table 1). Also, 360 (77.3%) respondents were women and 78 (16.7%) respondents were men. Regarding the academic program, 82 (17.6%) respondents were DoP and 382 (82%) respondents were PS students.
 |
Table 1 Demographic Data Of The Participating Students |
The percentage of respondents according to the academic grade is shown in Table 1. Achievement of the average academic mark is also shown in Table 1.
Exposure To PGx Education
Most students (n = 342, 73.4%) knew about PGx through their university education, 94 (20.2%) respondents knew about PGx through social media, and 12 (2.6%) students heard about PGx through scientific conferences (Table 2). Most students (n = 372, 79.8%) answered that they studied about PGx during university lectures. One-hundred and eighty-five (39.7%) students answered that they learnt about PGx in one course, 85 (18.2%) students learnt about PGx in two courses, 80 (17.2%) students learnt about PGx in more than two courses, and 108 (23.2%) students did not learn about PGx in any course during pharmaceutical studies at university. Most students (n = 258, 55.36%) responded that the number of total lectures in which PGx was mentioned fewer than three, 104 (22.3%) students answered that they took 3–5 lectures in PGx, 53 (11.4%) students learnt PGx in 6–10 lectures, and 42 (9%) students learnt about PGx in >10 lectures.
 |
Table 2 Educational Exposure To PGx |
Basic Knowledge Of PGx
A total of 448 (96.1%) respondents answered that they knew that human genetics can affect the drug response (Table 3). Many of the students (n = 433, 92.9%) answered that they knew that inter-individual variation in the drug response might be due to genetic factors. In addition, 410 (88%) responded that they knew that there were ethnic variations in the drug response. Most pharmacy students (n = 383, 82.2%) knew that genetic variants can affect the pharmacokinetic parameters of the drug, and 365 (78.3%) students knew that the interaction between the drug and its target may be influenced by variants in drug-target genes. Furthermore, 374 (80.3%) of respondents answered that some patients are at high risk of drug-induced toxicity due to inherited genetic variations, and 392 (84.1%) students responded that some patients do not respond to drug therapy due to certain genetic variants. Three-hundred and nineteen students (68.5%) responded that the drug response can be predicted through pharmacogenetic testing. When we compared the level of PGx knowledge among students, depending on the participating university, we found that An-Najah National University students had a significantly weaker knowledge of PGx (p < 0.05, ANOVA) in comparison with students from other universities (Table 4).
 |
Table 3 PGx Knowledge Among Participant Pharmacy Students In Jordan And West Bank Of Palestine (n = 466) |
 |
Table 4 Comparison Of Basic PGx Knowledge Of Participating Students Depending On The Participating University, Sex And Academic Year |
Knowledge About Specific Validated PGx Testing
The percentage of students who knew that CYP2C9 variants affected the response to warfarin was 59.2% (Table 5). In addition, 184 (39.5%) students answered that the response to warfarin is affected by VKORC1. Only 149 (31.97%) students knew that the gene for the endothelial growth factor receptor influences the response to kinase inhibitors (e.g., erlotinib). Lastly, 79 (17%) students knew that the FDA provides clinical evidence for PGx testing in the labeling of many drugs.
 |
Table 5 Knowledge About PGx Testing Recommended By The US FDA (n = 466) |
Attitudes Towards PGx Education
We found that 281 (60.3%) of respondents thought that the PGx information they received during their university education was not sufficient to enable them to understand the effects of genetic variants on the drug response. Only 183 (39.27%) students stated that the lecturer delivered information on PGx in a clear way (Table 2). Four-hundred and twenty-one (92.2%) students believed that PGx was helpful for pharmacists in choosing the correct drug at the appropriate dose. Most students (n = 432, 92.7%) wanted to know more about PGx. In addition, 82.4% of students were willing to apply PGx testing in clinical practice. However, only 31.5% wanted to study, in a postgraduate program, the science underpinning PGx. The attitudes towards PGx testing are shown in Table 6.
 |
Table 6 Attitudes Towards PGx Testing (n = 466) |
Factors Correlated With PGx Knowledge
We found that the number of courses and lectures in PGx correlated significantly (p < 0.05) with the level of PGx knowledge (Table 7). The academic year, university, and average marks achieved also correlated significantly (p value < 0.05) with the level of PGx knowledge. In addition, students who learnt about PGx from university courses had a significantly stronger level of PGx knowledge (p < 0.05, ANOVA) than students who learnt about PGx from scientific conferences and social media.
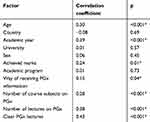 |
Table 7 Factors Correlated With PGx Knowledge |
Factors Correlated With PGx Attitudes
The attitude towards PGx was strongly correlated (p < 0.05) with PGx knowledge. Regression analyses revealed that the academic program (PS or DoP) and PGx knowledge were significantly (p < 0.05) correlated with attitudes towards PGx (Table 8).
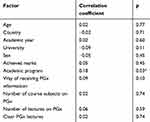 |
Table 8 Factors Correlated With Attitudes Toward PGx |
Discussion
There is a global trend to increase implementation of PGx testing in clinical practice. The acceptance of PGx testing among medical professionals is dependent upon the level of PGx knowledge.23
Several academic and research centers for PGx are distributed among the continents. In addition, some universities provide a postgraduate program in PGx (e.g., Manchester University, Manchester, UK). Among Middle Eastern Arab countries, practice of PGx is very limited to some specialist cancer centers.24 In addition, no academic or research centers specialize in PGx research/education. The situation in Jordan and WBP is not exceptional from other Middle Eastern countries.
We investigated the current knowledge and attitudes towards PGx among pharmacy students attending elite universities in Jordan and WBP. In general, students had a strong basic knowledge (Table 3) and positive attitudes (Table 6) towards PGx, even though the number of PGx courses/lectures is lower than that recommended by the International Society of Pharmacogenomics.9 Nevertheless, the knowledge among students towards certain commonly used drugs listed by the FDA and which require PGx testing was weak. These findings suggest that: (i) there is a strong desire to apply PGx in clinical practice in Jordan and WBP; (ii) the curricula of pharmacy departments in universities should be improved through implementation of more clinical cases which require PGx testing before and during drug treatment. Hopefully, improving PGx knowledge will prepare pharmacists to implement PGx testing in pharmacotherapy.
The level of PGx knowledge among pharmacy students in Jordan and WBP was stronger than that reported among medical-health students in Bosnia, where 45% of students were aware of different ethnicity-based aspects and only 50% had heard about PGx.12 In the present study, >80% of students in Jordan and WBP were aware of inter-individual and ethnic variations in the drug response, though the background of the participating students in these countries was different. Furthermore, the results regarding knowledge towards PGx among pharmacy students in Jordan and WBP were close to the data found in a survey done by pharmacy students in the Netherlands: most of the students had high expectations toward PGx, but only 12.8% felt adequately informed.25 Collectively, the PGx knowledge among pharmacy students in Jordan and WBP was strong in comparison with that in European and developed countries.
Most of the respondents in the present study were women. This sample was representative of current pharmacy students, whereby there are 3–4-times more women than men. This high women:men ratio has also been reported in pharmacy colleges in the USA.26 We found that women had a significantly stronger (p < 0.05, Student’s t-test) knowledge of PGx than men. This finding was because female students had significantly higher (p < 0.05, Student’s t-test) average academic marks than male students. The average academic marks correlated significantly with PGx knowledge (Table 7).
In general, there was no significant difference in knowledge of and attitudes towards PGx between students from Jordan and WBP. However, students from An-Najah National University (which is located in WBP) had the lowest score for PGx knowledge (Table 4). This finding was because most students from An-Najah National University had fewer than three lectures on PGx. We found that number of lectures and courses on PGx correlated positively and significantly with PGx knowledge among pharmacy students (Table 7).
The different pharmacy curricula affected attitudes towards PGx. DoP students had significantly (p < 0.05) better attitudes towards PGx than PS students. This observation may have been because DoP students practice clinical pharmacotherapy and personalized therapy more than PS students (who concentrate more on the pharmaceutical industry and marketing).
Ejilat et al found that Jordanian pharmacists have strong knowledge and attitudes towards PGx.27 We found that Jordanian pharmacy students had strong knowledge and good attitudes towards PGx. These results may indicate that pharmaceutical education in Jordanian universities had a major role in improving the knowledge and attitudes towards PGx among pharmacy students and, hence, pharmacists.
The academic year affected PGx knowledge (p < 0.05, ANOVA) and was found to correlate positively with PGx knowledge (Table 7). We found that Master of Science Students had significantly (p < 0.05) stronger PGx knowledge than undergraduate students. First-grade students had the weakest knowledge of PGx. This finding might have been because Master of Science Students as well as fifth- and fourth-grade students received more lectures and courses regarding PGx, whereas more junior students were not fully exposed to the pharmacology of the drugs that require PGx testing.
Although students had, in general, strong knowledge and good attitudes towards PGx, their knowledge of FDA recommendations regarding PGx testing of commonly used drugs (e.g., warfarin) was weak. This finding may indicate that the pharmaceutical curricula of the participating universities in Jordan and WBP did not contain clinical examples of PGx testing, and that training programs in clinical pharmacotherapy do not include validated PGx biomarkers. These can be considered to be weak points in PGx education and hamper future strategies regarding implementation of PGx in clinical practice.
Most students learnt about PGx from their university education (Table 2). In addition, students who learnt about PGx during university had a significantly (p < 0.05, ANOVA) stronger knowledge of PGx than students who knew about PGx from other sources. This finding may indicate the important role of university education in improving knowledge of PGx.28,29
Pharmacy students in Jordan and WBP did not know about specific clinical cases in which PGx testing can be used to optimize therapy. Based on our findings, on 2–3 August/2019, we conducted a workshop in the Association of Pharmacy in Amman on clinical implementation of PGx testing in clinical practice. We hope to remove the major barrier in PGx implementation: weak knowledge about PGx testing.
Our study had four main limitations. First, we did not investigate other barriers against implementation of PGx testing in clinical practice. Second, we included universities from one city in Jordan. Third, we recruited only pharmacy students and excluded medical students, who can contribute to future PGx practice. Finally, we did not ask students about molecular principles in PGx testing and interpretation of such results.
Conclusion
Pharmacy students among five universities in Jordan and WBP had fair knowledge and positive attitudes toward PGx. The curricula of pharmacy education in the participating universities should be reviewed and improved through implementation of more clinical cases that require PGx testing.
Acknowledgment
The authors highly appreciate all colleagues who helped in distribution of the online questionnaire among pharmacy students.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Aneesh TP, Sekhar S, Jose A, Chandran L, Zachariah SM. Pharmacogenomics: the right drug to the right person. J Clin Med Res. 2009;1(4):191–194.
2. Roden DM, Wilke RA, Kroemer HK, Stein CM. Pharmacogenomics: the genetics of variable drug responses. Circulation. 2011;123(15):1661–1670. doi:10.1161/CIRCULATIONAHA.109.914820
3. Johnson JA, Gong L, Whirl-Carrillo M, et al. Clinical pharmacogenetics implementation consortium guidelines for CYP2C9 and VKORC1 genotypes and warfarin dosing. Clin Pharmacol Ther. 2011;90(4):625–629. doi:10.1038/clpt.2011.185
4. Jarrar YB, Lee SJ. Molecular functionality of CYP2C9 polymorphisms and their influence on drug therapy. Drug Metabol Drug Interact. 2014;29(4):211–220. doi:10.1515/dmdi-2014-0001
5. Wang B, Canestaro WJ, Choudhry NK. Clinical evidence supporting pharmacogenomic biomarker testing provided in US Food and Drug Administration drug labels. JAMA Intern Med. 2014;174(12):1938–1944. doi:10.1001/jamainternmed.2014.5266
6. Brown JT, Bishop JR, Sangkuhl K, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for CYP2D6 genotype and atomoxetine therapy. Clin Pharmacol Ther. 2019. doi:10.1002/cpt.1409
7. Moriyama B, Obeng AO, Barbarino J, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines for CYP2C19 and voriconazole therapy. Clin Pharmacol Ther. 2017;102(1):45–51. doi:10.1002/cpt.583
8. Haga SB, Moaddeb J. Comparison of delivery strategies for pharmacogenetic testing services. Pharmacogenet Genomics. 2014;24(3):139–145. doi:10.1097/FPC.0000000000000028
9. Gurwitz D, Lunshof JE, Dedoussis G, et al. Pharmacogenomics education: international society of pharmacogenomics recommendations for medical, pharmaceutical, and health schools deans of education. Pharmacogenomics J. 2005;5(4):221–225. doi:10.1038/sj.tpj.6500312
10. Kisor DF, Farrell CL. Expanding pharmacist and student pharmacist access to genetics/genomics/pharmacogenomics competency education. J Med Educ Curric Dev. 2019;6:2382120519834325. doi:10.1177/2382120519834325
11. Blagec K, Koopmann R, Crommentuijn-van Rhenen M, et al. Implementing pharmacogenomics decision support across seven European countries: the Ubiquitous Pharmacogenomics (U-PGx) project. J Am Med Inform Assoc. 2018;25(7):893–898. doi:10.1093/jamia/ocy005
12. Mahmutovic L, Akcesme B, Durakovic C, et al. Perceptions of students in health and molecular life sciences regarding pharmacogenomics and personalized medicine. Hum Genomics. 2018;12(1):50. doi:10.1186/s40246-018-0182-2
13. Jarrar YB, Balasmeh AA, Jarrar W. Sequence analysis of the N-acetyltransferase 2 gene (NAT2) among Jordanian volunteers. Libyan J Med. 2018;13(1):1408381. doi:10.1080/19932820.2017.1408381
14. Zihlif M, Imraish A, Irshaid YM. Frequency of certain single-nucleotide polymorphisms and duplication of CYP2D6 in the Jordanian population. Genet Test Mol Biomarkers. 2012;16(10):1201–1205. doi:10.1089/gtmb.2011.0102
15. Jarrar YB. Perception of primary care physicians’ toward pharmacogenetics in Jordan. Jordan Med J. 2019;53(3):81–89.
16. Al-Qerem WJ, Al-Sheikh I, El Maadani A. The prevalence of drug-drug interactions and polypharmacy among elderly patients in Jordan. Biomed Res. 2018;29(12):1–6.
17. Al-Ramahi R, Raddad AR, Rashed AO, et al. Evaluation of potential drug-drug interactions among palestinian hemodialysis patients. BMC Nephrol. 2016;17:96. doi:10.1186/s12882-016-0317-4
18. Nazer LH, Tuffaha H. Health care and pharmacy practice in Jordan. Can J Hosp Pharm. 2017;70(2):150–155.
19. Dhingra S, Kumria R. A case report on the significance of clinical pharmacy services in India. Clin Case Rep. 2014;2(3):86–87. doi:10.1002/ccr3.63
20. Daniel WW. Biostatistics, a Foundation for Analysis in the Health Sciences.
21. Benzeroual KE, Shah B, Shinde S. Pharmacogenomics: assessing educational exposure, confidence in knowledge and training elements of pharmacists. Per Med. 2012;9(4):387–393. doi:10.2217/pme.12.44
22. Muzoriana N, Gavi S, Nembaware V, Dhoro M, Matimba A. Knowledge, attitude, and perceptions of pharmacists and pharmacy students towards pharmacogenomics in Zimbabwe. Pharmacy (Basel). 2017;5(3):
23. Zhang SC, Bruce C, Hayden M, Rieder MJ. Public perceptions of pharmacogenetics. Pediatrics. 2014;133(5):e1258–1267. doi:10.1542/peds.2013-2112
24. Albassam A, Alshammari S, Ouda G, Koshy S, Awad A, Rovers J. Knowledge, perceptions and confidence of physicians and pharmacists towards pharmacogenetics practice in Kuwait. PLoS One. 2018;13(9):e0203033. doi:10.1371/journal.pone.0203033
25. Bank PC, Swen JJ, Guchelaar HJ. A nationwide cross-sectional survey of pharmacy students on pharmacogenetic testing in The Netherlands. Pharmacogenomics. 2018;19(4):311–319. doi:10.2217/pgs-2017-0175
26. Taylor DA, Taylor JN. The pharmacy student population: applications received 2012–13, degrees conferred 2012–13, fall 2013 enrollments. Am J Pharm Educ. 2014;78(7):S2. doi:10.5688/ajpe787S2
27. Al Ejielat R, Ejielat Z, Andrawes S, Mhaidat NM. An evaluation of the knowledge, opinions, expectations and concerns toward pharmacogenomics among Jordanian pharmacists. Per Med. 2016;13(2):143–154. doi:10.2217/pme.15.50
28. Marcinak R, Paris M, Kinney SRM. Pharmacogenomics education improves pharmacy student perceptions of their abilities and roles in its use. Am J Pharm Educ. 2018;82(9):6424. doi:10.5688/ajpe6161
29. Patel RV, Chudow M, Vo TT, Serag-Bolos ES. Evaluation of pharmacy students’ knowledge and perceptions of pharmacogenetics before and after a simulation activity. Curr Pharm Teach Learn. 2018;10(1):96–101. doi:10.1016/j.cptl.2017.09.012
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
