Back to Journals » Clinical Ophthalmology » Volume 14
iStent Trabecular Microbypass Stent Implantation with Phacoemulsification in Patients with Open-Angle Glaucoma: 6-Year Outcomes
Authors Ferguson TJ , Mechels KB, Dockter Z, Bleeker A , Ibach M , Schweitzer J, Berdahl JP
Received 1 February 2020
Accepted for publication 17 April 2020
Published 2 July 2020 Volume 2020:14 Pages 1859—1866
DOI https://doi.org/10.2147/OPTH.S247910
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Tanner J Ferguson,1 Keegan B Mechels,1 Zachary Dockter,2 Adam Bleeker,2 Mitch Ibach,3 Justin Schweitzer,3 John P Berdahl3
1Cole Eye Institute, Cleveland Clinic, Cleveland, OH, USA; 2University of South Dakota Sanford School of Medicine, Sioux Falls, SD, USA; 3Vance Thompson Vision, Sioux Falls, SD, USA
Correspondence: Tanner J Ferguson Email [email protected]
Purpose: To investigate the long-term safety and efficacy of an iStent trabecular microbypass stent in combination with cataract surgery in eyes with primary open-angle glaucoma (POAG).
Setting: Private practice; Sioux Falls, South Dakota.
Design: Retrospective, consecutive case series.
Methods: This case series included eyes implanted with a single trabecular microbypass stent in combination with phacoemulsification in patients with mild to severe POAG. Data were collected preoperatively and at day 1, week 1, month 1, and up to 6 years postoperatively. Primary outcome measures included mean intraocular pressure (IOP) and number of glaucoma medications. Safety was noted by assessing the incidence of IOP spikes and need for additional surgery.
Results: The study comprised 411 eyes. Mean IOP was reduced to 14.9± 4.2 mmHg compared to 18.8± 5.6 mmHg at baseline at 6 years postoperative. The mean number of medications was reduced to 1.2± 1.0 from 1.4± 1.1 at baseline. In eyes with severe stage of disease, there was a mean IOP reduction > 6 mmHg at 6 years postoperative. Eyes with baseline IOP ≥ 18 mmHg achieved a more robust reduction in IOP. Fifteen eyes underwent a secondary glaucoma procedure. There were no intra- or postoperative complications.
Conclusion: Trabecular microbypass stent implantation in combination with cataract surgery provides a sustained IOP reduction in eyes with mild-to-severe POAG. The degree of IOP reduction was more significant in eyes with higher baseline IOP and severe stage of disease.
Keywords: microinvasive glaucoma surgery, MIGS, trabecular microbypass stent, surgical glaucoma, primary open-angle glaucoma
Introduction
Glaucoma is a leading cause of irreversible blindness globally, and disease burden is only expected to worsen with an estimated 111 million cases by 2040.1 Current approaches to treatment are focused on decreasing intraocular pressure (IOP), the only modifiable risk factor associated with the development and progression of open-angle glaucoma (OAG).2 Early in the disease process, ocular hypotensive pharmacotherapy has been an effective first-line treatment.3 However, topical therapies carry issues related to not only the tolerability, but also the consistency in drug administration, leading to poor compliance with therapy.4,5 While traditional surgical filtering procedures such as trabeculectomies and tube shunts remain options, they carry a significant risk profile.6,8
Minimally invasive glaucoma surgery (MIGS) is an established and growing space of new treatment options for primary and secondary OAG that offers a superior safety profile to traditional glaucoma procedures and can safely be combined with cataract surgery, as well as other MIGS procedures.9,10 The introduction of MIGS has stimulated a more proactive, interventional approach in the treatment of mild-to-moderate glaucoma, reducing the burden and minimizing the problems typically observed with topical glaucoma medications.11,12 MIGS procedures are safe and preserve the flexibility for future surgical intervention.13,14 The first FDA-approved MIGS device, the trabecular microbypass stent (iStent, Glaukos Corp.), was introduced in 2012 and has been extensively studied in patients with primary open-angle glaucoma, particularly in the short-term.15,18 There have been few studies, however, reporting long-term data in these patients.19
This study aims to investigate the long-term safety and efficacy of the trabecular microbypass stent placed in combination with cataract surgery in patients with POAG with outcomes out to 6 years postoperative. As stated previously, while short-term effectiveness and safety is widely known, longer term data is scarce and minimal. This study represents a continuation and expansion of a previous retrospective, consecutive case series that provided results out to 24 months, published in 2016.16
Methods
Study Design
Consecutive patients implanted with a single trabecular microbypass stent in combination with cataract surgery were included in this retrospective case series. Patients included had a preoperative diagnosis of mild-to-severe primary open-angle glaucoma. Staging of disease was based on the American Academy of Ophthalmology preferred practice pattern guidelines consistent with optic nerve and visual field changes (mild: no changes on white-on-white 24–2; moderate: changes in one hemifield and not within 5 degrees of fixation; severe: changes in both hemifields or changes within 5 degrees of fixation in at least one hemifield).3 No cases were excluded. This study was designed to mimic typical clinical use of the device and provide real-world long-term data. This was a retrospective case series that collected data from procedures that had already occurred and was de-identified; therefore, no informed consent process was utilized. The University of South Dakota Institutional Review Board approved this study.
Surgical Technique
The surgical technique in this study is identical to what was initially described in the previous study that evaluated outcomes through 24 months postoperatively.16
Postoperative Medications and Follow-Up
Postoperatively, patients were prescribed antibiotics for 1 week, a daily non-steroidal anti-inflammatory drug for 4 weeks and a topical steroid for 4 weeks. Patients were kept on their preoperative ocular hypotensive medications for at least 1 week and the decision to remove/stop medications was based on clinical judgment. As opposed to the prospective, restrictive clinical trials, no specific guidelines were utilized postoperatively to guide the decision to add or remove ocular hypotensive medications.
Preoperative data were used to establish a baseline, typically 1–2 weeks before the surgery. Postoperatively, data were collected from the following time points to compare to baseline: 1 day, 1 week, months 1, 3, and 6, as well as yearly out to 6 years postoperatively. At each time point, the data collected included IOP in addition to number and type of medications used. A consistent cohort group, a subgroup of eyes with 6-year data available, was also established to directly compare the eyes with 6-year postoperative data to baseline.
Outcome Measures and Safety Evaluation
The main outcome measures in the study were mean IOP as well as the mean number of ocular hypotensive (glaucoma) medications. Combination glaucoma medications (eg, dorzolamide-timolol) were logged as two medications in the data set. The baseline IOP, collected via Goldmann applanation tonometry, was obtained from the visit immediately prior to surgery and was based on a single measure. To evaluate the safety of the procedure, the need for additional surgery was noted in addition to the incidence of IOP spikes above baseline greater than or equal to 15 mmHg at any time point postoperatively. The type of secondary glaucoma procedure was also noted and eyes that underwent an additional procedure were included in the data set until the point of secondary intervention.
Statistical Analyses
A parametric paired t-test procedure was used to determine the significance of the mean change in IOP from baseline to all time points 6 months postoperatively (eg, 1 year, 2 years, etc.). To compare the mean change in the number of glaucoma medications, parametric paired t-test procedures were also employed to compare values at baseline versus postoperative time points. All the statistical analyses in this paper were carried out using SAS software (Version 9.4, SAS Institute, Cary, NC, USA). An α level of 0.05 was considered statistically significant.
Results
This retrospective, consecutive case series included 411 eyes in a clinical, real-world setting that underwent successful implantation of one trabecular microbypass stent (iStent) in combination with cataract surgery. At 6 years postoperatively, data was available for 120 of the 411 eyes included at baseline. In the data set, 247 of the 411 eyes were female and 164 were male. Table 1 demonstrates a summary of the preoperative characteristics of the study population.
 |
Table 1 This Table Demonstrates Baseline Subject Characteristics of All Eyes Included in the Study. Preoperative Characteristics |
Efficacy: Intraocular Pressure and Medications
Figure 1 shows the mean IOP and number of glaucoma medications for all eyes included in the retrospective chart review. Through 6 years postoperatively, the mean IOP and number of medications were collected and analyzed at each postoperative time point. At baseline, the mean IOP was 18.8±5.6 mmHg and the mean number of glaucoma medications was 1.4±1.1. At 6 months postoperatively, the IOP was 14.9±3.9 mmHg (P<0.01). This reduction was largely sustained with the mean IOP remaining <15.5 mmHg at each time point out to 6 years after surgery with a mean IOP of 14.9±4.2 mmHg (P<0.01). For medication use, the mean number of medications was 0.7±1.0 at 1 year postoperatively. At 3 years postoperatively, the mean number of medications was 0.9±1.1, increased from 0.8±1.1 at 2 years postoperatively. At 6 years postoperatively, the mean number of medications was 1.2±1.0 (P>0.05).
 |
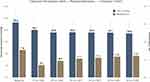
Figure 1 This figure demonstrates the mean IOP and number of glaucoma medications for all eyes included in the study out to 6 years postoperative. The error bars represent standard deviation. |
This study utilized a consistent cohort to directly compare the eyes with data available at 6 years postoperative to baseline. The mean IOP and glaucoma medications for the consistent cohort is shown in Figure 2. In this cohort, the baseline characteristics included a mean IOP of 18.6±6.4 mmHg and a mean of 1.6±1.1 medications. At 3 years postoperatively, the mean number of medications was 1.1±1.0 and the mean IOP was 15.3±3.7 mmHg. Six years after surgery, the mean IOP was reduced from baseline by 20% to 14.9±4.2 and the mean number of drops was 1.2±1.1. In the consistent cohort, eyes on ≥1 medication(s) at baseline decreased the number of medications from a mean of 1.9±0.9 at baseline to 1.4±1.1 at 6 years postoperative. In addition, eyes in the consistent cohort with a baseline IOP ≥18 mmHg had a year 6 mean IOP of 15.9±4.7 compared to 23.2±5.9 mmHg at baseline.
This study also stratified results based on baseline IOP, baseline number of medications, and glaucoma severity. In eyes with a baseline IOP ≥18 mmHg, the mean IOP prior to surgery was 22.5±4.6 mmHg. At 1 year postoperatively, the mean IOP was 16.6±4.2 mmHg and this reduction in pressure was maintained to 6 years postoperatively with a mean IOP of 15.9±4.7 mmHg (P<0.01). For medication use in this cohort, the mean number of medications was 1.0±1.0 (P>0.05) at 6 years postoperatively, down from 1.3±1.1 at baseline.
As mentioned previously, primary open-angle glaucoma severity was staged based on the AAO preferred practice pattern guidelines. In eyes with mild (n=234) stage of disease, prior to the surgery, the mean IOP was 19.0±5.5 and the mean number of medications was 1.1±1.0. At 3 years postoperative, mean IOP was 15.9±3.8 (P<0.01) and medications were reduced to 0.6±1.0 (P<0.05). At 6 years after surgery, the mean IOP was 16.4±3.9 mmHg (14% reduction from baseline) and the mean number of drops was 0.9±1.0 (P>0.05). In the moderate (n=93) stage of the disease subgroup, the mean year 6 IOP was reduced to 13.3±3.9 (P<0.01) mmHg (25% reduction) compared to 17.8±4.9 mmHg at baseline and the year 6 number of medications was 1.3±1.0 (P>0.05) versus 1.4±0.9 at baseline. In the severe (n=84) POAG subgroup, the mean IOP at 6 years was 13.0±3.9 (P<0.01) mmHg compared to 19.3±6.4 mmHg at baseline (33% reduction); the mean number of medications at 6 years was 1.7±1.3 (P>0.05), down from 2.1±1.3 at baseline. Figure 3 shows the comparison of IOP and medication reduction stratified by disease severity.
In the subset of eyes (n=159) being actively treated with ≥2 medication(s) at baseline, the year 6 mean number of medications was 1.7±1.2 (P<0.01), down from 2.6±0.7 preoperatively (35% reduction). In the subgroup of eyes with ≥3 glaucoma medications preoperatively, the mean medication burden was reduced to 2.0±1.0 (P<0.01) at year 6 compared to 3.2±0.6 preoperatively (1.2 medication decrease). In eyes not being treated with medication prior to the surgery, the mean number of medications was increased to 0.5±0.7 at 6 years postoperatively.
Proportional IOP analyses were also performed. At baseline, 59% of eyes had a baseline value ≤18 mmHg and 26% had baseline IOP ≤15 mmHg. By 1 year postoperative, the proportion of eyes with ≤18 mmHg increased to 81% and the proportion of eyes with ≤15 mmHg increased to 53%. In both subgroups, these values demonstrated stability out to 6 years postoperative with 83% of eyes at ≤18 mmHg and 53% of eyes remaining at ≤15 mmHg. These results are shown in Figure 4.
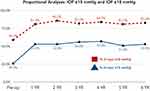 |
Figure 4 This figure demonstrates the IOP proportional analyses including the percentage of eyes at each time point with IOP ≤15 mmHg and IOP ≤18 mmHg. |
The magnitude of IOP reduction was also evaluated based on the baseline IOP in the consistent cohort (eyes with 6 year data available). To compare the magnitude of IOP reduction, the 6 year IOP was logged and compared to baseline. In eyes with a baseline IOP of 18–20 mmHg (n=23), the mean reduction in pressure was 3.6 mmHg at 6 years. In the subset of eyes with a baseline IOP ≥21 mmHg (n=36), the mean reduction in IOP was 9.7 mmHg, more than double than was observed in eyes with a baseline IOP 18–20 mmHg. Eyes with a baseline IOP <18 mmHg did not achieve a meaningful reduction in IOP at 6 years postoperatively with a 0.2 mmHg decrease in pressure.
Safety Profile
All patients included in the study had successful implantation of the device without perioperative complications. Over the 6-year follow-up period, no patients had sight-threatening complications including no hypotony, maculopathy, retinal detachment, or endophthalmitis. Twenty-five (6%) eyes had an of IOP increase ≥15 mmHg above baseline in the postoperative period, most of which occurred in the first month postoperatively and responded to topical therapy. Fifteen eyes (4%) underwent a secondary glaucoma procedure, with nine undergoing a secondary MIGS procedure and six undergoing a filtering procedure. No other ocular adverse events were identified postoperatively. Specifically, there were no reports of stent obstruction, hypotony, or inflammatory sequelae such as peripheral anterior synechiae.
For visual outcomes, at 6 years postoperative, 94% of eyes had corrected-distance visual acuity (CDVA) of 20/40 or better. Additionally, 75% of eyes achieved a vision of 20/25 CDVA or better at this time point.
During the 6-year follow-up period, 26 of the eyes included in the study died, all of which were unrelated to implantation of the device.
Discussion
The introduction of MIGS has altered the management of open-angle glaucoma, particularly those with mild–moderate stage of disease needing additional IOP reduction not achievable with conservative treatment options, but do not yet warrant the need for an aggressive filtering procedure and associated risks.20 MIGS has been demonstrated to be of particular value for reducing medication use. Owing to the recognized side effects of topical medication use and the reduced adherence with >1 drop, reduction of the medication burden in any capacity has long-term benefits for patients.21,23 Over the past decade, the MIGS category has grown immensely with devices targeting different anatomical regions for IOP reduction, enabling clinicians to provide an individualized approach to treatment. The wealth of options currently available may contribute to indecision from clinicians when choosing a procedure and, thus, it remains critical to continue investigating the different devices to identify whether certain patient- or disease-specific factors exist to tailor the MIGS device selection process.10,13
The short-term safety and efficacy of the trabecular microbypass stent in combination with cataract surgery is well documented by numerous studies; however, long-term data is scarce with the vast majority of studies demonstrating outcomes out to 12–36 months postoperative.17,24,26 Given the significant risks associated with traditional filtering glaucoma surgery as well as the propensity of the initial IOP reduction in laser trabeculoplasty to fade with time, the long-term data from these studies are of increasing utility.6,8,27,28 This study contains results out to six years post-operatively, making it one of the longest follow-up periods to date for trabecular microbypass stents in eyes with open-angle glaucoma. This study includes eyes with mild-to-severe stage of disease and the large sample size permitted comparison of the safety/efficacy of the procedure based on disease severity. Given the lack of studies evaluating MIGS devices in severe stage of open-angle glaucoma,29 the results of this study also provide additional insight into the use of MIGS in this patient population.
The study preceding this long-term study showed a meaningful reduction in IOP and medication use out to 24 months postoperatively.16 The results of this present study highlight the sustainable IOP-lowering ability of the trabecular microbypass stent in combination with cataract surgery with results out to 6 years postoperatively. In this study, the mean IOP at 6 years was 14.9±4.2 mmHg and the IOP remained <15.5 mmHg at all time points postoperatively, down from 18.8±5.6 mmHg at baseline, demonstrating the sustained pressure reduction. Furthermore, the proportion of eyes with IOP ≤15 mmHg at 1 year (53%) was maintained and stable through 6 years postoperative. For medication use, although there was an overall decrease in the medication burden at 6 years postoperative, there was an upward trend of medication use starting at 3 years postoperative. At 2 and 3 years postoperative, the mean number of medications was 0.9±1.1 and 1.1±1.0, respectively. At the year 6 time point, the mean number of medications was 1.2±1.1, down 21% from baseline. The long-term results of this study also highlight the use of this device in eyes with severe stage of disease, which has been previously demonstrated out to 24 months postoperative in a prior study exclusively evaluating severe POAG from the same practice. In this present study, there was an impressive IOP reduction, >6 mmHg, in this population down to 13.0±3.9 mmHg at 6 years postoperative.
With respect to the long-term safety of this procedure, the safety profile observed through 6 years was not markedly dissimilar than what was demonstrated through the first 24 months. The short-term safety profile of the trabecular microbypass stent has been corroborated by multiple studies.15,26 The long-term data is important as the trabecular microbypass stent avoids the well-documented later complications of filtering surgeries (ie, bleb-related issues, hypotony, astigmatism).30,31 Long-term safety is important to consider and recognize as quality-of-life is proposed as a notable benefit of the MIGS procedures, particularly with respect to the trabecular microbypass stent.10
The IOP-lowering benefit of cataract surgery alone has been established by numerous studies32 including the Ocular Hypertension Treatment Study (OHTS).33 In the OHTS trial, patients undergoing phacoemulsification alone achieved a 17% decrease in IOP and the reduction in IOP was proportional to baseline IOP with eyes <22.3 mmHg achieving an 11% reduction in IOP. In the OHTS trial, the mean baseline IOP was 23.9 mmHg, which makes it difficult to compare to the results of this study given the lower baseline IOP in our study (18.8 mmHg). However, recognizing that IOP reduction is proportional to baseline IOP, the 20% reduction at 6 years from baseline in the consistent cohort in this study suggests the trabecular microbypass stent augments the IOP reduction observed with phacoemulsification alone, which is consistent with prior studies demonstrating the IOP-lowering ability of the stent alone.24,34
While these results continue to be promising for the treatment of OAG, this study is not without limitations. The design of this study was open-label and nonrandomized. It was also retrospective in nature which prohibits a uniform follow-up pattern that contributes to missing data at specific time points. The loss to follow-up is a drawback of the study and it’s possible that patients lost to follow-up may have undergone an additional procedure elsewhere which limits our conclusions related to the long-term safety profile of the device. However, given that this was a retrospective case series ranging from 2012 to 2015, over 30% of cases were taken from 2014/2015 and thus 6-year data was not available for these eyes. Despite these limitations, this study provides a large sample size and the longest follow-up data to date evaluating the safety and efficacy of this device in conjunction with cataract surgery. Moreover, this study was a consecutive case series that did not utilize inclusion or exclusion criteria and is representative of a typical clinician’s real-world patient population.
To our knowledge, this long-term study presents the longest follow-up data of a study evaluating the iStent trabecular microbypass stent and represents the largest sample size published to date with >400 eyes included. The large sample size of this study enabled stratification of results based on glaucoma severity and baseline characteristics that provides valuable insight. The findings of this study support the use of the device in mild-to-severe stage of disease. Moreover, eyes with a higher baseline IOP (eg, ≥18 mmHg) achieve a more robust reduction in IOP. Despite being retrospective, this study provides important insight regarding the long-term safety and efficacy of the trabecular microbypass stent in combination with cataract surgery.
Acknowledgment
This work was presented at the 2019 American Society of Cataract and Refractive Surgeons (ASCRS) Annual Meeting, San Diego, CA, USA.
Disclosure
Drs. Ferguson, Ibach, Schweitzer, and Berdahl are consultants and speakers for Glaukos Corp. Tanner J Ferguson reports personal fees from Glaukos outside the submitted work and consultancy for Equinox Ophthalmic, Inc. Mitch Ibach reports consulting and lecture honoraria from Glaukos outside the submitted work. Justin Schweitzer reports personal fees from Glaukos during the conduct of the study and outside the submitted work and consultant and lecturer honorarium from Glaukos. John P Berdahl reports grants from Glaukos during the conduct of the study and personal fees from Glaukos outside the submitted work. The authors report no other possible conflicts of interest in this work.
References
1. Tham Y-C, Li X, Wong TY, Quigley HA, Aung T, Cheng C-Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–2090. doi:10.1016/j.ophtha.2014.05.013
2. Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression: results from the early manifest glaucoma trial. Arch Ophthalmol. 2002;120(10):1268–1279. doi:10.1001/archopht.120.10.1268
3. Prum BE, Rosenberg LF, Gedde SJ, et al. Primary open-angle glaucoma preferred practice pattern(®) guidelines. Ophthalmology. 2016;123:p41–111. doi:10.1016/j.ophtha.2015.10.053
4. Boland MV, Ervin A-M, Friedman DS, et al. Comparative effectiveness of treatments for open-angle glaucoma: a systematic review for the U.S. preventive services task force. Ann Intern Med. 2013;158(4):271–279. doi:10.7326/0003-4819-158-4-201302190-00008
5. Tsai JC. A comprehensive perspective on patient adherence to topical glaucoma therapy. Ophthalmology. 2009;116(11 Suppl):S30–6. doi:10.1016/j.ophtha.2009.06.024
6. Jampel HD, Musch DC, Gillespie BW, Lichter PR, Wright MM, Guire KE. Perioperative complications of trabeculectomy in the collaborative initial glaucoma treatment study (CIGTS). Am J Ophthalmol. 2005;140(1):16–22. doi:10.1016/j.ajo.2005.02.013
7. Chen J, Gedde SJ. New developments in tube shunt surgery. Curr Opin Ophthalmol. 2019;30(2):125–131. doi:10.1097/ICU.0000000000000549
8. Rulli E, Biagioli E, Riva I, et al. Efficacy and safety of trabeculectomy vs nonpenetrating surgical procedures: a systematic review and meta-analysis. JAMA Ophthalmol. 2013;131(12):1573–1582. doi:10.1001/jamaophthalmol.2013.5059
9. Lavia C, Dallorto L, Maule M, Ceccarelli M, Fea AM. Minimally-invasive glaucoma surgeries (MIGS) for open angle glaucoma: a systematic review and meta-analysis. PLoS One. 2017;12(8):e0183142. doi:10.1371/journal.pone.0183142
10. Shah M. Micro-invasive glaucoma surgery – an interventional glaucoma revolution. Eye Vis Lond Engl. 2019;6(1):29. doi:10.1186/s40662-019-0154-1
11. Tsai T, Robin AL, Smith JP. An evaluation of how glaucoma patients use topical medications: a pilot study. Trans Am Ophthalmol Soc. 2007;105:
12. Gupta R, Patil B, Shah BM, Bali SJ, Mishra SK, Dada T. Evaluating eye drop instillation technique in glaucoma patients. J Glaucoma. 2012;21(3):189–192. doi:10.1097/IJG.0b013e31820bd2e1
13. Saheb H, Ahmed I, Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol. 2012;23(2):96–104. doi:10.1097/ICU.0b013e32834ff1e7
14. Grace M, Richter ALC. Minimally invasive glaucoma surgery: current status and future prospects. Clin Ophthalmol Auckl NZ. 2016;10:189–206. doi:10.2147/OPTH.S80490
15. Craven ER, Katz LJ, Wells JM, Giamporcaro JE. Cataract surgery with trabecular micro-bypass stent implantation in patients with mild-to-moderate open-angle glaucoma and cataract: two-year follow-up. J Cataract Refract Surg. 2012;38(8):1339–1345. doi:10.1016/j.jcrs.2012.03.025
16. Ferguson TJ, Berdahl JP, Schweitzer JA, Sudhagoni RG. Clinical evaluation of a trabecular microbypass stent with phacoemulsification in patients with open-angle glaucoma and cataract. Clin Ophthalmol Auckl NZ. 2016;10:1767–1773. doi:10.2147/OPTH.S114306
17. Vold SD, Voskanyan L, Tetz M, et al. Newly diagnosed primary open-angle glaucoma randomized to 2 trabecular bypass stents or prostaglandin: outcomes through 36 months. Ophthalmol Ther. 2016;5(2):161–172. doi:10.1007/s40123-016-0065-3
18. Samuelson TW, Katz LJ, Wells JM, Duh Y-J, Giamporcaro JE. Randomized evaluation of the trabecular micro-bypass stent with phacoemulsification in patients with glaucoma and cataract. Ophthalmology. 2011;118(3):459–467. doi:10.1016/j.ophtha.2010.07.007
19. Neuhann TH, Hornbeak DM, Neuhann RT, Giamporcaro JE. Long-term effectiveness and safety of trabecular microbypass stent implantation with cataract surgery in patients with glaucoma or ocular hypertension: five-year outcomes. J Cataract Refract Surg. 2019;45(3):312–320. doi:10.1016/j.jcrs.2018.10.029
20. Shah M, Law G, Ahmed IIK. Glaucoma and cataract surgery. Curr Opin Ophthalmol. 2016;27(1):51–57. doi:10.1097/ICU.0000000000000224
21. Baudouin C, Renard J-P, Nordmann J-P, et al. Prevalence and risk factors for ocular surface disease among patients treated over the long term for glaucoma or ocular hypertension. Eur J Ophthalmol. 2012;23(1):47–54. doi:10.5301/ejo.5000181
22. Baudouin C, Liang H, Hamard P, et al. The ocular surface of glaucoma patients treated over the long term expresses inflammatory markers related to both T-helper 1 and T-helper 2 pathways. Ophthalmology. 2008;115(1):109–115. doi:10.1016/j.ophtha.2007.01.036
23. Robin AL, Novack GD, Covert DW, Crockett RS, Marcic TS. Adherence in glaucoma: objective measurements of once-daily and adjunctive medication use. Am J Ophthalmol. 2007;144(4):533–540. doi:10.1016/j.ajo.2007.06.012
24. Donnenfeld ED, Solomon KD, Voskanyan L, et al. A prospective 3-year follow-up trial of implantation of two trabecular microbypass stents in open-angle glaucoma. Clin Ophthalmol Auckl NZ. 2015;9:2057–2065. doi:10.2147/OPTH.S91732
25. Belovay GW, Naqi A, Chan BJ, Rateb M, Ahmed IIK. Using multiple trabecular micro-bypass stents in cataract patients to treat open-angle glaucoma. J Cataract Refract Surg. 2012;38(11):1911–1917. doi:10.1016/j.jcrs.2012.07.017
26. Myers JS, Masood I, Hornbeak DM, et al. Prospective evaluation of two istent® trabecular stents, one istent supra® suprachoroidal stent, and postoperative prostaglandin in refractory glaucoma: 4-year outcomes. Adv Ther. 2018;35(3):395–407. doi:10.1007/s12325-018-0666-4
27. Juzych MS, Chopra V, Banitt MR, et al. Comparison of long-term outcomes of selective laser trabeculoplasty versus argon laser trabeculoplasty in open-angle glaucoma. Ophthalmology. 2004;111(10):1853–1859. doi:10.1016/j.ophtha.2004.04.030
28. Neuhann TH. Trabecular micro-bypass stent implantation during small-incision cataract surgery for open-angle glaucoma or ocular hypertension: long-term results. J Cataract Refract Surg. 2015;41(12):2664–2671. doi:10.1016/j.jcrs.2015.06.032
29. Ferguson T, Swan R, Ibach M, Schweitzer J, Sudhagoni R, Berdahl JP. Evaluation of a trabecular microbypass stent with cataract extraction in severe primary open-angle glaucoma. J Glaucoma. 2018;27(1):71–76. doi:10.1097/IJG.0000000000000825
30. Delbeke H, Stalmans I, Vandewalle E, Zeyen T. The effect of trabeculectomy on astigmatism. J Glaucoma. 2016;25(4):e308–e312. doi:10.1097/IJG.0000000000000236
31. Higashide T, Ohkubo S, Sugimoto Y, Kiuchi Y, Sugiyama K. Persistent hypotony after trabeculectomy: incidence and associated factors in the collaborative bleb-related infection incidence and treatment study. Jpn J Ophthalmol. 2016;60(4):309–318. doi:10.1007/s10384-016-0450-4
32. Poley BJ, Lindstrom RL, Samuelson TW. Long-term effects of phacoemulsification with intraocular lens implantation in normotensive and ocular hypertensive eyes. J Cataract Refract Surg. 2008;34(5):735–742. doi:10.1016/j.jcrs.2007.12.045
33. Mansberger SL, Gordon MO, Jampel H, et al. Reduction in intraocular pressure after cataract extraction: the ocular hypertension treatment study. Ophthalmology. 2012;119(9):1826–1831. doi:10.1016/j.ophtha.2012.02.050
34. Ferguson TJ, Ibach M, Schweitzer J, et al. Trabecular microbypass stent implantation in pseudophakic eyes with open-angle glaucoma: long-term results. J Cataract Refract Surg. 2019;45(4):414–420. doi:10.1016/j.jcrs.2012.03.025
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.