Back to Journals » Medical Devices: Evidence and Research » Volume 14
Intramedullary Nail Breakage and Mechanical Displacement in Patients with Proximal Femoral Fractures: A Commercial and Medicare Supplemental Claims Database Analysis
Authors Chitnis AS, Ray B, Sparks C , Grebenyuk Y, Vanderkarr M, Holy CE
Received 29 October 2020
Accepted for publication 16 December 2020
Published 9 February 2021 Volume 2021:14 Pages 15—25
DOI https://doi.org/10.2147/MDER.S288188
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Abhishek S Chitnis,1 Bidusee Ray,2 Charisse Sparks,3 Yuriy Grebenyuk,4 Mollie Vanderkarr,4 Chantal E Holy1
1Real World Data Sciences, Medical Device Epidemiology, Johnson & Johnson, New Brunswick, NJ, USA; 2Mu-Sigma, Bangalore, India; 3DePuy Orthopedics, Inc., West Chester, PA, USA; 4Health Economics and Market Access, DePuy Synthes, West Chester, PA, USA
Correspondence: Abhishek S Chitnis
Real World Data Sciences, Medical Device Epidemiology, Johnson & Johnson Co., 410 George Street, New Brunswick, NJ, 08901, USA
Email [email protected]
Objective: This study evaluated the rates and patterns of intramedullary nail (IMN) breakage and mechanical displacement for proximal femur fractures and the factors associated with their occurrence.
Patients and Methods: Patients with subtrochanteric, intertrochanteric, or basicervical femoral neck fractures treated with IMN from 2016 to 2019 were identified from commercial and Medicare supplemental claims databases and were followed for up to two years. Kaplan–Meier analysis estimated the cumulative incidence of and patterns of breakage/mechanical displacement. Multivariable Cox regression models evaluated the factors associated with breakage/mechanical displacement.
Results: A total of 11,128 patients had IMN fixation for subtrochanteric, intertrochanteric, or basicervical femoral neck fractures: (mean SD) age 75.6 (16.4) years, 66.2% female, 74.3% Medicare supplemental vs 26.7% commercial insurance. Comorbidities included hypertension (62.9%), osteoporosis (27.3%), cardiac arrhythmia (23.1%), diabetes (30.7%), and chronic pulmonary disease (16.3%). Most fractures were closed (97.2%), intertrochanteric or basicervical femoral neck (80.1%), and not pathological (91.0%). The cumulative incidence of nail breakage over two years was 0.66% overall, 1.44% for combination fractures, 1.16% for subtrochanteric fractures, and 0.49% for intertrochanteric or basicervical fractures. The cumulative incidence of mechanical displacement was 0.37% overall, 0.43% for subtrochanteric fractures, 0.42% for combination fractures, and 0.36% for intertrochanteric or basicervical femoral neck fractures. Half of the breakages occurred within five months after surgery and half of the mechanical displacements occurred within 75 days. Age 50– 64 (vs 75+) and subtrochanteric or pathological fracture were more commonly associated with nail breakage. Complicated hypertension was more commonly associated with mechanical displacement.
Conclusion: The incidence of IMN breakage and mechanical displacement in US commercial and Medicare supplemental patients with proximal femur fractures from 2016 to 2019 was low (0.66% and 0.37%, respectively up to two years). Age 50– 64 (vs 75+) and subtrochanteric or pathological fracture were more commonly associated with breakage. Complicated hypertension was associated with mechanical displacement.
Keywords: intramedullary nailing, IMN, complications, breakage, mechanical displacement, retrospective claims database evaluation
Introduction
Proximal femoral fractures account for a large proportion of hospitalizations among trauma cases, and their clinical burden and costs place a great strain on society.1–4 Intertrochanteric fractures occur in the area between the greater and lesser trochanter and are the most common type of hip fracture, accounting for nearly half of all hip fractures.5 Subtrochanteric fractures, which occur in the area within 5 cm distal to the lesser trochanter, are prone to nonunion and malunion and require proper reduction before and during fixation to ensure favorable results.6 Basicervical femoral neck fractures occur between the base of the femoral neck and the trochanteric region7 and may be regarded as an intermediate form due to their anatomical location.8,9 A variety of options for fixation may be considered for basicervical femoral neck fractures.7 Many questions still remain regarding the optimal management of proximal femoral fractures.6 The choice of implant depends upon the fracture pattern, the age of the patient, and the patient’s existing comorbidities.6
Intramedullary nailing (IMN) has been used to treat proximal femoral fractures for more than 80 years10,11 and an increasing trend in IMN utilization has been observed over the past two decades. Data from the US Veterans Affairs found that IMN utilization increased from 1998 to 2005, varying geographically.12 A subsequent analysis of Medicare data showed increasing utilization of IMN vs sliding hip screw from 2005 to 2011 (46.9% to 79.1%).13 A previous evaluation by our research group using commercial and Medicare supplemental data found that IMN was the most common treatment for fractures of the femur over the past four years and IMN utilization rates have been constant during that time.14
IMN fixation can be challenging given the inherent nature of many of the patients’ fractures and the health status of much of the patient population.15 Complications of IMN reported in the literature include malalignment, cutout, infection, false drilling, wrong lag screw length, drill bit breakage, malrotation of the femoral diaphysis, elongation of the femur, impaired bone healing, periprosthetic fracture, fracture collapse, implant failure, lag screw intrapelvic migration, neurovascular injury, secondary varus deviation, pain, and refracture. Implant device fracture is rare (range in published literature from 0.2% to 5.6%16–18), however it is often a tragic event as revision is very complex and difficult in this typically vulnerable patient population.15
Implant breakage usually occurs at the level of the lag screw aperture,15 although the nail itself may also break, usually at distal barrel taper or at the nail lag screw aperture.15,19–21 Reasons for the breakage may be excessive premature weight bearing or prolonged cyclical loading (eg, with nonunion).19–21 Mechanical displacement of IMN occurs when there is problematic movement of the IMN (eg, rotation, angulation, etc) that may be associated with malreduction and subsequently fracture malunion, nonunion, or shortening.22,23
Rates of nail breakage or mechanical displacement following surgical repair of proximal femoral fractures with IMN are not well established as these depend on multiple factors such as fracture type, patient comorbidities, surgical approach, and the type of IMN.19–21 A better understanding of the rates and patterns of occurrence of IMN breakage and mechanical displacement would be helpful to evaluate the magnitude of these problems and possibly how to avoid them. The objective of this study was to use administrative claims data to evaluate the rates of, and factors associated with, IMN breakage and mechanical displacement in patients with subtrochanteric, intertrochanteric, or basicervical femoral neck fractures.
Patients and Methods
Data Sources
This study used US administrative claims data from >300 large self-insured US employers and >25 US health plans included in the IBM MarketScan® Commercial and Medicare Supplemental Research Database. Commercial data constitutes individuals ≤65 years of age (primary insured, spouse, or dependent) and Medicare supplemental data includes patients with Medicare government health insurance (≥65 years of age) with supplemental private insurance. The database includes demographic and enrollment information (ie, age, gender, US geographic region, US type of health insurance payer, employment status, monthly enrollment status, and mental health carve-out information), inpatient and outpatient medical (ie, length of stay, service date and duration, type of provider, place of service, payment, deductible, copayment), and outpatient pharmacy claims (ie, national drug codes, therapeutic class, date of dispensing, days supplied and quantity, and amounts paid). International Classification of Diseases, 9th and 10th Revisions, Clinical Modification (ICD-9-CM and ICD-10-CM) diagnosis and procedure codes are utilized.
Patient Population
Patients with IMN fixation for subtrochanteric, intertrochanteric, or basicervical femoral neck fractures between 2016 and 2019 were identified from the database. Patient data were collected were for up to two years (maximum) postsurgery. Inclusion criteria were: age ≥18 years, femur fracture hospitalization with IMN repair between 2016 and 2019 (date of hospitalization for the fracture repair procedure=index date), diagnosis for intertrochanteric, basicervical femoral neck or subtrochanteric femur fractures on or 30 days prior to index hospitalization, and enrollment pre-index (baseline). Exclusion criteria were: baseline long bone fractures, amputation during index hospitalization, or polytrauma (multiple bone fractures during index hospitalization).
Study Measures
Baseline Demographic and Clinical Characteristics
Patient demographics included age, sex, insurance coverage, census region, and year of index hospitalization. Baseline comorbidity (ie, comorbid conditions present prior to implantation of the nails) was assessed using the Elixhauser Comorbidity Index, an aggregate measure of comorbidity that includes 31 comorbidity indicators. Higher values on Elixhauser are associated with greater comorbidity. Prior research has shown that Elixhauser scores are associated with risk of mortality and health care utilization. Individual baseline comorbidities and injury severity scores were also assessed. Fracture characteristics evaluated included open fractures, pathological fractures, and the location of the fracture.
Outcome Measures
Two primary outcomes were evaluated for IMN fixation of subtrochanteric, intertrochanteric, or basicervical femoral neck fractures in the study: (1) nail breakage, defined as a subsequent hospitalization with ≥1 ICD-10 diagnosis code for breakdown of internal device and ≥1 ICD-10 procedure code for femur fracture repair or device removal from femur occurring concomitantly within the same inpatient hospitalization; and (2) nail mechanical displacement, defined as a subsequent hospitalization with ≥1 ICD-10 diagnosis code for displacement of internal device and ≥1 ICD-10 procedure code for femur fracture repair or device removal from femur occurring concomitantly within the same inpatient hospitalization.
Statistical Analyses
Study variables were analyzed descriptively using counts and proportions (dichotomous variables) and means and standard deviations (continuous variables). A Kaplan–Meier analysis estimated the cumulative incidence of breakage and mechanical displacement over the two-year period, for all patients overall by fracture type. Patients were censored if they died or at the end of the study period. Two separate multivariable Cox regression models evaluated the factors associated with nail breakage and mechanical displacement. HRs, 95%CI, and p-values were reported.
Results
A total of 11,128 patients from the longitudinal database received IMNs for subtrochanteric, intertrochanteric, or basicervical femoral neck fractures between 2016 and 2019 and were included in the study.
Baseline Demographic and Clinical Characteristics
Mean (SD) age of patients was 75.6 (16.4) years and two-thirds of the patients (66.2%) were female (Table 1). Three-quarters of the patients (74.3%) were from the Medicare supplemental database, more than three-quarters (77.7%) were employees, and most had preferred provider organization (PPO) insurance (47.4%) or comprehensive insurance (28.5%). A greater proportion of the patients were from the South (37.5%) and Midwest (28.6%) census regions of the US and a greater proportion of patients had surgery in 2016 (32.8%) or 2017 (26.2%).
 |
Table 1 Baseline Demographic Characteristics of Patients Undergoing IMN Fixation in the Database from 2016 to 2019 |
Major comorbidities for patients with IMN fixation were hypertension (uncomplicated 52.7% and complicated 10.2%), osteoporosis (27.3%), cardiac arrhythmia (23.1%), diabetes (uncomplicated 17.1% and complicated 13.6%), chronic pulmonary disease (16.3%), hypothyroidism (16.2%), and peripheral vascular disorders (15.2%) (Table 2). One-third of patients (33.5%) had an Elixhauser comorbidity score of 1–2, one-quarter of patients (25.1%) had a score of 3–4, and one-fifth each of patients had Elixhauser comorbidity scores of 0 (21.5%) and >5 (19.9%). The mean (SD) Elixhauser comorbidity score was 2.7 (2.4), the mean (SD) FCI score was 2.5 (2.0), the mean (SD) CCI score was 1.7 (2.1), and the mean (SD) new injury severity score was 23.4 (5.9). Most fractures were closed fractures (97.2%), intertrochanteric or basicervical femoral neck (80.1%), 12.5% were a combination of (intertrochanteric or basicervical femoral neck) and subtrochanteric and 7.4% were subtrochanteric, and not pathological (91.0%) (Table 2). Mean (SD) length of stay (LOS) per patient with IMN fixation was 6.4 (4.7) days.
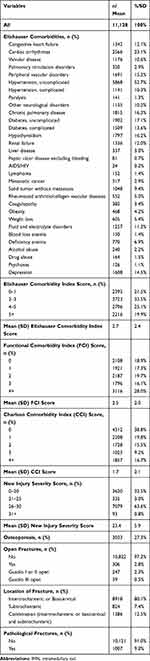 |
Table 2 Baseline Clinical Characteristics of Patients Undergoing IMN Fixation in the Database from 2016 to 2019 |
IMN Breakage
The cumulative incidence of breakage of IMN for proximal femoral fractures over two years was only 0.66% overall (Figure 1). The incidence of nail breakage was highest with combination fractures (1.44%), followed by subtrochanteric fractures (1.16%) and intertrochanteric or basicervical fractures (0.49%).
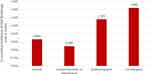 |
Figure 1 Cumulative incidence of nail breakage over two years by fracture type for patients undergoing IMN fixation. |
Among patients with nail breakage, a Kaplan–Meier curve presenting the timing of IMN nail breakage to two years is shown in Figure 2. Half of the nail breakages occurred within the first five months after surgery (range: 116–460 days), and the remaining breakages occurred at a constant rate over the remaining 18 months.
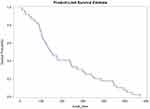 |
Figure 2 Timing of IMN breakage over two years for patients with breakage. |
A multivariable Cox regression model evaluated the factors associated with a breakage of IMN for proximal femoral fractures. Age 50–64 (vs 75+), subtrochanteric fracture, and pathological fracture were more commonly associated with nail breakage. Peptic ulcer disease excluding bleeding was marginally significantly associated with nail breakage. Employee (ie, the policyholder or individual with the health insurance vs spouse/other) was negatively associated with nail breakage (Table 3).
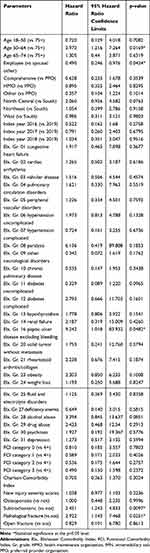 |
Table 3 Multivariable Cox Regression Model of Factors Associated with IMN Breakage Among Patients in the Database from 2016 to 2019 |
IMN Mechanical Displacement
Using Kaplan–Meier analysis, the cumulative incidence of mechanical displacement of IMN for proximal femoral fractures over 2 years was only 0.37% overall (Figure 3). The incidence of mechanical displacement was higher with subtrochanteric (0.43%) and combination (0.42%) fractures, and lower with intertrochanteric or basicervical femoral neck fractures (0.36%).
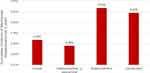 |
Figure 3 Cumulative incidence of mechanical displacement over two years by fracture type for patients undergoing IMN fixation in the database from 2016 to 2019. |
Figure 4 presents the Kaplan–Meier analysis showing the timing of IMN mechanical displacement over two years among patients with mechanical displacement. Half of the mechanical displacements occurred within the first 75 days after surgery (range 116–460 days), and most of the remaining breakages occurred within the first year after surgery.
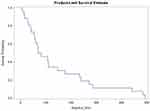 |
Figure 4 Timing of IMN mechanical displacement for patients with mechanical displacement. |
The factors associated with mechanical displacement of IMN for proximal femoral fractures were also evaluated with a multivariable Cox regression model. Only complicated hypertension was associated with mechanical displacement (Table 4).
 |
Table 4 Multivariable Cox Regression Model of Factors Associated with IMN Mechanical Displacement Among Patients in the Database from 2016 to 2019 |
Discussion
Many patients undergoing IMN fixation for proximal femoral fractures in the commercial and Medicare supplemental claims database had comorbid illness including hypertension, osteoporosis, cardiac arrhythmia, diabetes, chronic pulmonary disease, and peripheral vascular disorders. Most fractures were closed fractures (97.2%) and not pathological (91.0%). In regard to fracture location, 80.1% were intertrochanteric or basicervical, 12.5% were a combination of intertrochanteric/basicervical femoral neck and subtrochanteric, and 7.4% were subtrochanteric.
The cumulative incidence of implant breakage over two years in patients with IMN fixation for proximal femoral fractures was 0.66% overall and was highest with combination fractures (1.44%), followed by subtrochanteric fractures (1.16%) and intertrochanteric or basicervical femoral neck fractures (0.49%). Half of the IMN breakages occurred within the first five months after surgery. These observed rates are towards the lower end of the range of rates of IMN breakage reported in the published literature (0.2–5.6%),16–18 possibly due to improved health care technologies and practices over the years.
Understanding the factors associated with IMN breakage is helpful for potentially improving our understanding of how these events can be avoided. Multiple factors such as fracture type, patient comorbidities, surgical approach, and the type of IMN may affect the likelihood of nail breakage.19–21,24–26 Subtrochanteric fractures, which occur in the area within 5 cm distal to the lesser trochanter, are prone to nonunion and malunion and require proper reduction before and during fixation to ensure favorable results.6 Reasons for the breakage may also be attributed to excessive premature weight bearing or prolonged cyclical loading (eg, with nonunion).19–21
The current study found that age 50–64 (vs 75+) and subtrochanteric or pathological fracture were more often associated with IMN breakage. These factors are mostly consistent with a study in the UK from 2004 to 2013 by Johnson et al15 who found that younger age, low American Society of Anesthesiologists (ASA) score, subtrochanteric fracture, and pathological fracture were independent nail fracture risk factors in proximal femoral fractures. These authors suggested that “The links between both youth and low ASA suggest that nail failure may be a more prominent feature of moderate to high demand patients.”15
In regard to the types of proximal femoral fractures more commonly associated with IMN breakage, the findings that subtrochanteric and pathological fractures were more commonly associated with IMN breakage observed in the current study are also consistent with Johnson et al.15 A higher rate of IMN breakage in pathologic fractures was also observed by Willeumier et al27 who found that 8% of patients with femoral metastases experienced breakage between 2000 and 2015 at five centers in the Netherlands. Only 7.4% of the fractures treated with IMN in the database were subtrochanteric and only 9% were pathological.
The cumulative incidence of mechanical displacement of IMN for proximal femoral fractures over two years was 0.37% overall and was higher with subtrochanteric (0.43%) and combination (0.42%) fractures, and lower with intertrochanteric or basicervical fractures (0.36%). Half of the mechanical displacements occurred within the first 75 days after surgery. We are not aware of any previously published studies that evaluated mechanical displacement of IMN in proximal femoral fractures; however, the quality of fracture reduction has been shown to be an important factor affecting the revision rate in patients with mechanical complications after osteosynthesis with proximal femoral nail for trochanteric fractures.28 The current study is also unique in its finding that the only factor associated with mechanical displacement was complicated hypertension.
Closer follow-up of patient subgroups who may be at increased risk of IMN breakage and mechanical displacement of proximal femoral fractures might be beneficial until bony union has been achieved.15 Johnson et al also suggest that other treatment options such as proximal femoral replacement may be considered for higher risk patients (eg, pathological fracture).15
The utilization of administrative claims data has limitations as the data are collected for reimbursement purposes and biases may exist (eg, changes in coding over time, financial incentives, etc).29,30 Claims data also may have errors and may be missing clinical variables of relevance.29,30 Event rates derived from claims data are limited to those in which a corrective procedure occurs. For example, some patients may prefer to live with a mechanical displacement rather than undergo elective revision, and these cases of mechanical displacement would not be identified from the claims database. Furthermore, the specificity of the events and reasons for their occurrence are also not available in claims data. For example, for mechanical displacement, the ICD-10 codes do not provide information on the exact nature or cause of the mechanical displacement (eg, cut-out, cut through, etc). Finally, it is important to note that data were derived from commercial and Medicare supplemental claims databases and may not reflect patients with other types of US health care insurance or patients in other countries.
Conclusions
The prevalence of IMN breakage and mechanical displacement were low in US commercial and Medicare supplemental patients with subtrochanteric, intertrochanteric, or basicervical femoral neck fractures of the femur from 2016 to 2019. Age 50–64 (vs 75+) and subtrochanteric or pathological fracture were more commonly associated with nail breakage and complicated hypertension was more commonly associated with mechanical displacement. It may be beneficial to advise closer follow-up of some subgroups of patients until bony union has been achieved.
Abbreviations
ASA, American Society of Anesthesiologists; Elx., Elixhauser Comorbidity Index; FCI, Functional Comorbidity Index; FDA, Food and Drug Administration; GERD, gastroesophageal reflux disease; Gr, Grade; HMO, health maintenance organization; ICD-9/10-CM, International Classification of Diseases, 9th/10th Revision, Clinical Modification; IMN, intramedullary nailing; LOS, length of stay; NDCs, national drug codes; PPI, proton pump inhibitors PPO, preferred provider organization; VASQIP, Veterans Affairs Surgical Quality Improvement Program.
Data Sharing Statement
The data that support the findings of this study are available but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors (Abhishek S Chitnis) upon reasonable request and with permission of the database owner.
Ethics Approval and Informed Consent
Ethics approval from an Institutional Review Board and informed consent were not required for this study as it used data from an anonymous, de-identified, administrative claims database compliant with the Health Insurance Portability and Accountability Act of 1996.
Acknowledgments
Editorial assistance with the manuscript was provided by Natalie Edwards, Health Services Consulting Corporation, Boxborough, MA, USA.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
The study was funded by Johnson & Johnson (JnJ). Company employees and a contractor were involved in the conduction of the study and the preparation of the manuscript. The authors had full control of the manuscript and provided their final approval of all content.
Disclosure
ASC, CS, YG, MV, and CEH are employees of JnJ and own stock in the company, DePuy Synthes is a part of JnJ family of companies. BR is affiliated with Mu-Sigma and was a contractor with JnJ at the time of the study. The authors report no other conflicts of interest in this work.
References
1. Liporace FA, Egol KA, Tejwani N, Zuckerman JD, Koval KJ. What’s new in hip fractures? Current concepts. Am J Orthop (Belle Mead NJ). 2005;34(2):66–74.
2. Keene GS, Parker MJ, Pryor GA. Mortality and morbidity after hip fractures. BMJ (Clinical Research Ed. 1993;307(6914):1248–1250.
3. Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51(3):364–370. doi:10.1046/j.1532-5415.2003.51110.x
4. Metcalfe D, Salim A, Olufajo O, et al. Hospital case volume and outcomes for proximal femoral fractures in the USA: an observational study. BMJ Open. 2016;6(4):e010743. doi:10.1136/bmjopen-2015-010743
5. Canale ST, Beaty JH. Campbell’s Operative Orthopaedics e-Book. Elsevier Health Sciences; 2012.
6. Mittal R, Banerjee S. Proximal femoral fractures: principles of management and review of literature. J Clin Orthop Trauma. 2012;3(1):15–23. doi:10.1016/j.jcot.2012.04.001
7. Kweon SH, Lee SH, Kook SH, Choi YC. Outcomes of cephalomedullary nailing in basicervical fracture. Hip Pelvis. 2017;29(4):270–276. doi:10.5371/hp.2017.29.4.270
8. Lieberman JR. AAOS Comprehensive Orthopaedic Review 3. Lippincott Williams & Wilkins; 2019.
9. Sharma A, Sethi A, Sharma S. Comparative analysis of treatment of basicervical femur fractures in young adults with CCS, DHS, and PFN. Rev Bras Ortop. 2018;53(6):783–787. doi:10.1016/j.rbo.2017.08.009
10. Born CT, Pidgeon T, Taglang G. 75 years of contemporary intramedullary nailing. J Orthop Trauma. 2014;28:S1–S2. doi:10.1097/BOT.0000000000000163
11. Vecsei V, Hajdu S, Negrin L. Intramedullary nailing in fracture treatment: history, science and küntscher’s revolutionary influence in Vienna, Austria. Injury. 2011;42(Suppl 4):S1–S5. doi:10.1016/S0020-1383(11)00419-0
12. Radcliff TA, Regan E, Cowper Ripley DC, Hutt E. Increased use of intramedullary nails for intertrochanteric proximal femoral fractures in veterans affairs hospitals: a comparative effectiveness study. J Bone Joint Surg Am. 2012;94(9):833–840. doi:10.2106/JBJS.I.01403
13. Werner BC, Fashandi AH, Gwathmey FW, Yarboro SR. Trends in the management of intertrochanteric femur fractures in the United States 2005–2011. Hip Int. 2015;25(3):270–276. doi:10.5301/hipint.5000216
14. Chitnis AS, Ray B, Sparks C, Grebenyuk Y, Vanderkarr M, Holy CE. Long bone fractures: treatment patterns and factors contributing to use of intramedullary nailing. Expert Rev Med Devices. 2020;17(7):731–737. doi:10.1080/17434440.2020.1779055
15. Johnson NA, Uzoigwe C, Venkatesan M, et al. Risk factors for intramedullary nail breakage in proximal femoral fractures: a 10-year retrospective review. Ann R Coll Surg Engl. 2017;99(2):145–150. doi:10.1308/rcsann.2016.0297
16. Alvarez DB, Aparicio JP, Fernández EL, Múgica IG, Batalla DN, Jiménez JP. Implant breakage, a rare complication with the gamma nail. A review of 843 fractures of the proximal femur treated with a gamma nail. Acta Orthop Belg. 2004;70(5):435–443.
17. Iwakura T, Niikura T, Lee SY, et al. Breakage of a third generation gamma nail: a case report and review of the literature. Case Rep Orthop. 2013;2013:172352. doi:10.1155/2013/172352
18. Abram SG, Pollard TC, Andrade AJ. Inadequate ‘three-point’ proximal fixation predicts failure of the gamma nail. Bone Joint J. 2013;95–B(6):825–830.
19. Erez O, Dougherty PJ. Early complications associated with cephalomedullary nail for intertrochanteric hip fractures. J Trauma Acute Care Surg. 2012;72(2):E101–E105. doi:10.1097/TA.0b013e31821c2ef2
20. Rollo G, Rinonapoli G, Pichierri P, Bisaccia M, Caraffa A, Meccariello L. Breakage in two points of a short and undersized “affixus” cephalomedullary nail in a very active elderly female: a case report and review of the literature. Case Rep Orthop. 2018;2018:9580190.
21. Rollo G, Tartaglia N, Falzarano G, et al. The challenge of non-union in subtrochanteric fractures with breakage of intramedullary nail: evaluation of outcomes in surgery revision with angled blade plate and allograft bone strut. Eur J Trauma Emerg Surg. 2017;43(6):853–861. doi:10.1007/s00068-016-0755-5
22. Jiang L, Zheng Q, Pan Z. What is the fracture displacement influence to fracture non-union in intramedullary nail treatment in subtrochanteric fracture? J Clin Orthop Trauma. 2018;9(4):317–321. doi:10.1016/j.jcot.2018.04.002
23. Santolini E, West R, Giannoudis PV. Risk factors for long bone fracture non-union: a stratification approach based on the level of the existing scientific evidence. Injury. 2015;46(Suppl 8):S8–S19. doi:10.1016/S0020-1383(15)30049-8
24. Bisaccia M, Caraffa A, Rinonapoli G, et al. Feasibility and value of non-locking retrograde nail vs. locking retrograde nail in fixation of distal third femoral shaft fractures: radiographic, bone densitometry and clinical outcome assessments. Med Glas (Zenica). 2020;17(1):163–169. doi:10.17392/1097-20
25. Lanzetti RM, Caraffa A, Lupariello D, et al. Comparison between locked and unlocked intramedullary nails in intertrochanteric fractures. Eur J Orthop Surg Traumatol. 2018;28(4):649–658. doi:10.1007/s00590-018-2143-9
26. Maiettini D, Bisaccia M, Caraffa A, et al. Feasibility and value of radiographic union score hip fracture after treatment with intramedullary nail of stable hip fractures. Acta Inform Med. 2016;24(6):394–396. doi:10.5455/aim.2016.24.394-396
27. Willeumier JJ, Kaynak M, van der Zwaal P, et al. What factors are associated with implant breakage and revision after intramedullary nailing for femoral metastases? Clin Orthop Relat Res. 2018;476(9):1823–1833. doi:10.1007/s11999.0000000000000201
28. Koyuncu S, Altay T, Kayali C, Ozan F, Yamak K. Mechanical failures after fixation with proximal femoral nail and risk factors. Clin Interv Aging. 2015;10. doi:10.2147/CIA.S96852
29. Patel AA, Singh K, Nunley RM, Minhas SV. Administrative databases in orthopaedic research: pearls and pitfalls of big Data. J Am Acad Orthop Surg. 2016;24(3):172–179. doi:10.5435/JAAOS-D-13-00009
30. Bohl DD, Singh K, Grauer JN. Nationwide databases in orthopaedic surgery research. J Am Acad Orthop Surg. 2016;24(10):673–682.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
