Back to Journals » Open Access Emergency Medicine » Volume 13
Implementation of a Provider in Triage and Its Effect on Left without Being Seen Rate at a Community Trauma Center
Authors Sember M, Donley C , Eggleston M
Received 6 December 2020
Accepted for publication 9 March 2021
Published 29 March 2021 Volume 2021:13 Pages 137—141
DOI https://doi.org/10.2147/OAEM.S296001
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Hans-Christoph Pape
Maria Sember, Chad Donley, Matthew Eggleston
Department of Emergency Medicine, Mercy Health Youngstown Hospital, Youngstown, OH, USA
Correspondence: Chad Donley
Department of Emergency Medicine, Mercy Health Youngstown Hospital, 1044 Belmont Avenue, Youngstown, OH, 44504, USA
Tel +1 330-480-3667
Fax +1-330-729-7961
Email [email protected]
Introduction: Emergency department (ED) overcrowding is a nationally recognized problem and multiple strategies have been proposed and implemented with varying levels of success. It has caused patients to present to the ED but leave without being seen (LWBS). These patients suffer delayed diagnosis, delayed treatment, and ultimately increased morbidity and mortality. In efforts to decrease the number of patients who leave without being seen, one proposed solution is to place a provider in triage to evaluate these patients at the initial point of contact.
Methods: A retrospective chart review was conducted on patient’s presenting to the Emergency Department from October through January for the years 2013 through 2017. A list of all patient dispositions for each study month was analyzed and compared for the 4 consecutive years with the implementation of an Advanced Practice Provider (APP) in triage.
Results: A total of 2162 patients dispositioned as LWBS during the entire study period of October 2013 through January 2017 were enrolled in the analysis. After implementation of a provider in triage, there was a 39% overall decrease (95% CI 0.005) in patients who left the ED before completion of treatment. There was a 69% reduction (95% CI 0.005) in patients who left before seeing the provider in triage. After seeing the provider, we saw an 83% reduction (95% CI< 0.001) in LWBS. Overall, our initial LWBS rate was found to be 5%, and after implementation of a provider in triage that rate decreased to 1%.
Discussion: The addition of a provider in triage decreased our LWBS rate from 5% to 1%. The addition of a provider in triage also helped identify sick patients in the waiting room and helped facilitate more rapid assessment of ED patients on arrival.
Keywords: LWBS, triage, provider, ED overcrowding, walkouts, LWOTs, PIT
Introduction
With the dynamic changes in healthcare today, patients are increasing utilizing the Emergency Department (ED) as a source of primary care.2 This is especially true in inner city and underserved populations, such as Youngstown, Ohio. Weinick et al found that 13.7–27.1% of all emergency department visits in the United States could be managed in physician offices, clinics, and urgent care centers at a savings of $4.4 billion annually.3 With finite resources and fixed physical space, this influx of patients can lead to a multitude of problems. One of the most prevalent consequences is ED overcrowding. It is a nationally recognized problem,1 but despite previous strategies being proposed and implemented, this is still a challenge today.4,5 With ever-increasing volumes of patients presenting for evaluation, there is even more pressure placed on EDs to “move” patients through the department faster. Hospital administration tracks numerous metrics including door to physician times and ED patient length of stay (LOS). Trying to improve these throughput times is a complex process made even more difficult when the hospitals have high admission rates and limited inpatient bed capacity. Increased ED volumes coupled with lack of physical inpatient space results in boarding of patients in the Emergency Department.6 All these bottlenecks further increase the likelihood of a patient leaving without being seen (LWBS).7
The most dangerous patient in the ED is the untriaged patient. When large numbers of patients present to the ED simultaneously, it is difficult to quickly and effectively evaluate them. Patients may be critically ill but go undetected while awaiting nurse triage, leading to delay in care and increased morbidity and mortality.8 While ED triage has historically been a fixed process,9 more flexible models have been proposed. Researchers have suggested that having a trained medical provider assessing these patients at the point of initial contact will more rapidly discover some of these lurking conditions.6 One such strategy is to allow a nurse to initiate a standard set of orders in triage based on the patient’s chief complaint. These order sets vary between facilities and are approved by their respective medical directors.10 This model attempts to bridge the time gap from patient arrival to seeing the physician and having orders pending.11,12 However, their chief complaint may not be reflective of their symptoms or story. More information can be gathered with pointed questions and a focused physical exam from another clinician, such as a Physician Assistant or Nurse Practitioner (referred collectively as an advanced practice provider (APP)). Previous strategies used a nurse in triage to implement protocol orders, but LWBS rates were still on the rise. Though ED throughput and improvement of time-dependent quality metrics have always been of interest to hospitals and leadership teams, more focus has been on those patients who initially register to be seen in the ED but then leave without being seen. Patients choosing to leave the department lead to problems with delayed diagnosis, delayed treatment, and ultimately increased morbidity and mortality. Garland conducted a study that stated those who initially were LWBS but then came back to the ED were triaged at a high acuity and had an increased mortality.13 Our proposed solution to help combat this problem is placing a provider in triage, an APP, to assess patients at their initial time of presentation. It is important for a provider to take the time to ask more in-depth questions about a chief complaint and perform a focused history and physical. This can be done in triage by an APP and would assist in discovering ill patients in the waiting room to more promptly begin the treatment process. There are additional published data that examines the effect of this intervention and its decrease in LWBS rate.14,15 With this in mind, St. Elizabeth Youngstown Hospital decided to implement a similar program.
Methods
After receiving approval from Mercy Health St. Elizabeth Youngstown Hospital Institutional Review Board (IRB), we performed a retrospective chart review from October 2013 through January 2017 at St. Elizabeth Youngstown Hospital. The IRB waiver of informed consent was granted based on this being a retrospective study with minimal risk to the participants and without adversely affecting their rights and welfare. All data results were reported in a de-identified and summarized format. The data was kept on a password-protected computer and in encrypted files. The study was conducted in compliance with the declaration of Helsinki.
This facility historically sees increased patient volumes and experiences ED boarding of admitted in-patients between October and January, so these 4 months were analyzed and compared for 4 consecutive years with the implementation of an APP in triage. A list of all patient dispositions for each study month was generated using the electronic medical record (EPIC), and these dispositions were categorized as either “LWBS-before-triage”, “LWBS-after-triage”, or “Eloped.” The stages of patient interactions in the ED were as follows. Stage 1: patient sign in, stage 2: patient is triaged by a nurse, stage 3: patient is seen by a provider in triage, stage 4: patient is seen in the main ED by a physician. In the LWBS-before-triage category, the patient left the ED after stage 1. The LWBS-after-triage is when the patient left after stage 2. The Eloped category contained those patients who left after stage 3 or 4. These patients would have diagnostic testing pending but did not stay for the results or completion of their care. In November 2015 we implemented a provider in triage during peak hours, specifically a nurse practitioner or physician assistant, who could perform a brief exam, place orders, or rapidly discharge low acuity patients directly from triage. The pre-study period started in October 2013 and included 9 months of data during which a nurse would triage and place protocol orders, but there was no APP in triage. Post intervention had 7 months of data ending in January 2017. A total of 2162 patients dispositioned as LWBS during the entire study period of October 2013 through January 2017 were enrolled in the analysis. If there was a change in the disposition, it was accounted for in the data analysis. Patient volumes and staffing were consistent throughout the study period.
Results
After implementation of a provider in triage beginning in November 2015, there was a 39% overall decrease (95% CI 0.005) in patients who left the ED before completion of treatment, as shown in Figure 1. Inappropriate disposition combines LWBS-before-triage, LWBS-after-triage, and elopement. There was a 69% reduction (95% CI 0.005) in patients who left before seeing the provider in triage, as shown in Figure 2. After seeing the provider, we saw an 83% reduction (95% CI<0.001) in LWBS, as depicted in Figure 3. However, our elopement rate did increase by 67% (95% CI −0.003), as Figure 4 shows. Overall, our initial LWBS rate was found to be 5%, and after implementation of a provider in triage that rate decreased to 1%.
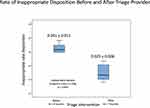 |
Figure 1 Rate of inappropriate disposition before and after provider-in-triage implementation. |
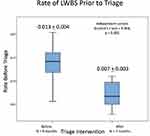 |
Figure 2 Rate of LWBS prior to triage, before and after provider-in-triage implementation. |
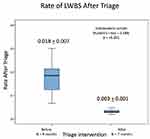 |
Figure 3 Rate of LWBS after triage before and after provider-in-triage implementation. |
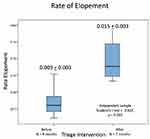 |
Figure 4 Rate of elopement before and after provider-in-triage implementation. |
Discussion
St. Elizabeth Youngstown Hospital is a level 1 trauma center and sees, on average, about 53,000 ED visits per year. Our initial LWBS rate before the study was 5%, which equates to approximately 2650 patients that have LWBS. After the implementation of a provider in triage in November 2015, the rate decreased to 1%, or approximately 560 patients. Thus, we were now able to start care from triage for 2160 patients that would have previously left the ED. The addition of a provider in triage has not only helped identify sick patients in the waiting room and get them evaluated quicker but it helps us disposition the patients in a timely manner once they are taken to the main ED.
When the data is further divided into categories for LWBS-before-triage, LWBS-after-triage, and Eloped, additional conclusions can be drawn. Figure 1 shows that overall there was a 39% decrease in patients who left the ED. It is labeled inappropriate disposition due to the fact that they left before seeing a nurse, a provider, or not staying to the completion of their treatment. The next category was LWBS-before-triage, in which we saw a 69% reduction after the implementation of a provider in triage. Having the provider in triage allows them to start an initial evaluation sooner and see more patients in the waiting room. If the patient had a low acuity complaint, this also gave our provider the opportunity to treat them and discharge the patient directly from the triage area.
Our greatest reduction was seen in LWBS-after-triage, which was 83%. This is where we expected most of our change to be because of the provider placing orders for lab work and imaging. This was also useful in identifying the patients who were more ill to ensure that they were sent to the main ED quicker for further evaluation. As previously stated, the most dangerous patient is the one that is not seen. With this provider-in-triage model, we experienced improved efficiency in moving patients through the department and dispositioning them. Based on patient experience surveys, patients had improved satisfaction that orders could be placed early in triage and speak with a provider.11 When they did arrive in the main ED, physicians were then able to more smoothly assume responsibility of care to go over lab results and continue the workup.
There were also some patients who, after speaking with a provider in triage and who had labs and imaging pending, left the ED because they did not want to wait for the results. We observed an increase in our elopement rate of 67%. Future research will investigate this increase, evaluating the average LOS before and after the implementation of a provider in triage to see if the LOS increased the likelihood of a patient to elope. Research has shown that there is a positive correlation between LOS and the LWBS rate.16 Other factors that may have contributed to the overall increase in elopement rate are the door-to-room times and door-to-doctor times, which have also been proven to influence LWBS rates.17
Limitations
There are several limitations of this study. This was a fairly small sample of 2162 patients, and a larger data set is preferred. There is also variability between the providers in triage, how fast they see patients, and what they order for lab work and imaging. Also, the provider’s decision on patient acuity level affects how quickly they are seen. As stated before, there is an association between LOS and LWBS rate. While we cannot control the hospital volume, it does affect us in the ED and how quickly we can get admitted patients upstairs before we have multiple holds in the ED. As hospital volume increases, so too does a patient’s LOS and the time needed to have them roomed to see another provider. This change in our triage model supports our goals to decrease the LWBS rate and to closely evaluate more patients from the moment they walk into the ED.
Conclusion
This study shows an overall statistically significant reduction in patients who left the ED before their care was completed. There was a significant decrease in the LWBS rate after seeing a provider in triage, but there was also an increase in patients who eloped from the ED. We observed an overall 39% reduction in the total number of patients who left prior to the completion of their treatment. We also achieved our goal of reduction in the hospital’s LWBS rate, which went from 5% to 1% after implementation of a provider in triage.
Disclosure
Dr Chad Donley reports grants from LECOMT Research Support Grant, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Derlet R, Richards J, Kravitz R. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med. 2001;8(2):151–155. doi:10.1111/j.1553-2712.2001.tb01280.x
2. Walls CA, Rhodes KV, Kennedy JJ. The emergency department as usual source of medical care: estimates from the 1998 National Health Interview Survey. Acad Emerg Med. 2002;9(11):1140–1145. doi:10.1111/j.1553-2712.2002.tb01568.x
3. Weinick RM, Burns RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health Aff. 2010;29(9):1630–1636. PMID:20820018; PMCID: PMC3412873. doi:10.1377/hlthaff.2009.0748
4. Trzeciak S, Rivers EP. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J. 2003;20(5):402–405. doi:10.1136/emj.20.5.402
5. Derlet R, Richards J. Overcrowding in the nation’s emergency departments: complex cases and disturbing effects. Ann Emerg Med. 2000;35(1):63–68. doi:10.1016/S0196-0644(00)70105-3
6. Love RA, Murphy JA, Lietz TE, Jordan KS. The effectiveness of a provider in triage in the emergency department: a quality improvement initiative to improve patient flow. Adv Emerg Nurs J. 2012;34(1):65–74. doi:10.1097/TME.0b013e3182435543
7. Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16(1):1–10. doi:10.1111/j.1553-2712.2008.00295.x
8. Atzema CL, Austin PC, Tu JV, Schull MJ. Emergency department triage of acute myocardial infarction patients and the effects on outcomes. Ann Emerg Med. 2009;52(6):736–745. doi:10.1016/j.annemergmed.2008.11.011
9. Beveridge R, Ducharme J, Janes L, Beaulieu S, Walter S. Reliability of the Canadian emergency department triage and acuity scale: interrater agreement. Ann Emerg Med. 1999;34(2):155–159. doi:10.1016/s0196-0644(99)70223-4
10. Douma M, Drake C, O’Dochartaigh D, Smith K. A pragmatic randomized evaluation of a nurse-initiated protocol to improve timeliness of care in an urban emergency department. Ann Emerg Med. 2016;68(5):546–552. doi:10.1016/j.annemergmed.2016.06.019
11. Hwang C, Payton T, Weeks E, Plourde M. Implementing triage standing orders in the emergency department leads to reduced physician-to-disposition times. Acad Emerg Med. 2016:6. Article ID 7213625. doi:10.1155/2016/7213625
12. Retezar R, Bessman E, Ding R, Zeger SL, McCarthy ML. The effect of triage diagnostic standing orders on emergency department treatment time. Ann Emerg Med. 2011;57(2):89–99.e2. doi:10.1016/j.annemergmed.2010.05.016
13. Garland A, Ramsey CD, Fransoo R, et al. Rates of readmission and death associated with leaving hospital against medical advice: a population-based study. CMAJ. 2013;185(14):1207–1214. doi:10.1503/cmaj.130029
14. Holroyd BR, Bullard MJ, Latoszek K, et al. Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial. Acad Emerg Med. 2007;14(8):702–708. doi:10.1197/j.aem.2007.04.018
15. Wiler J, Gentle C, Halfpenny J, et al. Optimizing emergency department front-end operations. Ann Emerg Med. 2010;55(2):142–160. doi:10.1016/j.annemergmed.2009.05.021
16. Carron PN, Yersin B, Trueb L, Gonin P, Hugli O. Missed opportunities: evolution of patients leaving without being seen or against medical advice during a six-year period in a Swiss tertiary hospital emergency department. Biomed Res Int. 2014;2014:690368. doi:10.1155/2014/690368
17. Pielsticker S, Whelan L, Arthur AO, Thomas S. Identifying patient door-to-room goals to minimize left-without-being-seen rates. West J Emerg Med. 2015;16(5):611–618. doi:10.5811/westjem.2015.7.25878
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
