Back to Journals » Therapeutics and Clinical Risk Management » Volume 13
Impact of T1 slope on surgical and adjacent segment degeneration after Bryan cervical disc arthroplasty
Authors Yang P, Li Y, Li J, Shen Y
Received 6 April 2017
Accepted for publication 7 August 2017
Published 29 August 2017 Volume 2017:13 Pages 1119—1125
DOI https://doi.org/10.2147/TCRM.S138990
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang

Peng Yang,1 Yongqian Li,2,3 Jia Li,2,3,* Yong Shen2,3,*
1Department of Neurosurgery, Affiliated Hospital of North China University of Science and Technology, Tangshan, 2Department of Orthopedic Surgery, 3Key Laboratory of Orthopedic Biomechanics of Hebei Province, the Third Hospital of Hebei Medical University, Shijiazhuang, People’s Republic of China
*These authors contributed equally to this work
Background: This retrospective study investigated an association between preoperative T1 slope and surgical and adjacent segment degeneration (SASD) after Bryan cervical disc arthroplasty (BCDA) in patients with cervical degenerative disc disease.
Methods: Based on preoperative standing lateral radiographs, 90 patients were classified according to T1 slope that was higher or lower than the 50th percentile (high T1 or low T1, 28 and 62 patients, respectively). Patients were also classified as SASD or non-SASD (38 and 52 patients, respectively) determined by radiographs at final follow-up. Visual analog scale (VAS) and Neck Disability Index (NDI) scores for neck and arm pain were noted, and changes in the sagittal alignment of the cervical spine (SACS), functional spinal unit (FSU) angle, and FSU range of motion (ROM) were also noted. Univariate and multivariate logistic regression analyses were performed to determine the risk factors for SASD.
Results: The overall rate of SASD was 42.2% (38/90). The SACS, FSU angle, FSU ROM, and SASD rates of the high T1 and low T1 slope groups were significantly different at the last follow-up. The NDI and VAS scores of the high T1 slope group were significantly greater than those of the low T1 slope. The multivariate logistic regression analysis showed that high T1 slope and endplate coverage discrepancy (ie, residual space behind the prosthesis) were significant risk factors for SASD after BCDA.
Conclusion: High T1 slope and endplate coverage discrepancy were associated with SASD after BCDA. Patients with a high preoperative T1 slope have a smaller FSU angle and more neck pain after BCDA.
Keywords: Bryan cervical disc arthroplasty, surgical and adjacent segment degeneration, T1 slope, endplate coverage discrepancy, risk factor, clinical outcomes
Introduction
Anterior cervical discectomy and fusion (ACDF) is used to treat cervical degenerative disc disease and has proved clinically efficacious.1,2 Yet an alternative to fusion is Bryan cervical disc arthroplasty (BCDA), which preserves motion of the cervical disc and decreases the incidence of surgical and adjacent segment degeneration (SASD). Many studies have reported the excellent clinical and radiologic results of BCDA at early-to-intermediate follow-ups.3–5
Nevertheless, SASD is a postoperative complication after BCDA, which is contrary to its fundamental target. SASD after BCDA includes osteophyte formation, narrowing of the disc space, and ossification of the anterior or posterior longitudinal ligament, all of which may require revision surgery. Several risk factors have been associated with the development of SASD after BCDA, including advanced age, male sex, surgical techniques, indications, preoperative high-intensity signal in the spinal cord, and multilevel BCDA.6–8 Yi et al9 reported that 69 of 170 patients (40.6%) experienced new osteophyte formation after arthroplasty. Walraevens et al10 found that after treatment of single-level cervical disk disease with the Bryan cervical disc, almost 8% of patients were immobilized owing to new osteophyte formation. Very recently, Yanbin et al11 reported heterotopic ossification at 69.0% (29/42; 33 patients) and SASD at 47.6% (30/42) of the total surgical levels.
An important method to evaluate cervical sagittal balance is according to the T1 slope, defined as the sagittal angle between a horizontal line and the cephalad endplate of T1 in a standing lateral radiograph. A previous study found that a high T1 slope was predictive of kyphotic changes occurring after cervical laminoplasty,12 which led to greater cervical lordosis to maintain a horizontal gaze. However, until now there has been little consistent evidence regarding an association between T1 slope and SASD after BCDA. An investigation is warranted to determine if the T1 slope may be a risk factor for SASD after BCDA, as this may influence methods for prevention.
It is our hypothesis that the T1 slope will predict SASD after BCDA, influencing the mechanical dynamics of the cervical spine and adversely affecting the clinical outcome. To determine this, the present retrospective study investigated an association between the degree of preoperative T1 slope, as measured on radiographs, and the rate of postoperative SASD in patients with cervical degenerative disc disease after BCDA.
Methods
The Regional Ethics Committee of Third Hospital of Hebei Medical University approved this retrospective study. Patient consent to review medical records was not required, as all data were de-identified. All methods were conducted in accordance with the approved guidelines. This material has not been published and is not under consideration elsewhere.
Study population
This retrospective study initially included 101 consecutive patients who underwent single-level BCDA for cervical degenerative disc diseases between January 2005 and January 2010. The inclusion criteria were radiculopathy, myelopathy or both due to single-level disc herniation or spondylosis (C3-C7), which was not responsive to appropriate nonsurgical treatment of ≥3 months. Patients with any of the following were excluded from this analysis: spinal infections; previous cervical spine surgery; marked cervical instability; severe spondylosis; disc height loss at the level to be treated; ossification of the posterior longitudinal ligament; and bridging osteophytes.
Surgical technique
The appropriate size of the prosthesis (Medtronic Sofamor Danek) was determined by preoperative templating and radiographic studies. All surgical procedures were performed by the same surgeon using the anterior approach via a right-sided skin incision. The posterior longitudinal ligament was excised completely. For the purpose of adequate decompression, the spinal canal and neuroforamen were also decompressed. The endplates were prepared using the Bryan disc milling technique, which creates 2 concave surfaces. Then after endplate preparation, we used saline to irrigate the operative site before insertion of the devices.
Analytical design
Clinical data were collected preoperatively and postoperatively at 3, 6, 12, 24, 36, and 72 months. When the follow-up was longer than 6 years, the last data available were used for statistical analysis. The visual analog scale (VAS) and Neck Disability Index (NDI) were used to determine neck and arm pain. Functional status was judged by the modified Japanese Orthopedic Association (JOA) scoring system.
Radiographic data included static and dynamic flexion/extension lateral images. SASD was evaluated from radiographs by 2 independent doctors who were blinded to the clinical outcomes. SASD included new anterior, posterior, or enlarging osteophyte formation and calcification of the anterior longitudinal ligament, or a disc space narrowing to <30% of the intervertebral disc space.
Based on the last follow-up radiographs and VAS, NDI, and JOA scores, the patients were classified as having or not having, SASD (the SASD and non-SASD groups, respectively). The preoperative T1 slope was measured as the angle between a horizontal line and a line tangent to the cephalad endplate of T1 in a standing lateral radiograph. For the purposes of this study, the T1 slopes were considered higher or lower than the 50th percentile (the high T1 and low T1 groups, respectively).
The sagittal alignment of the cervical spine (SACS) was defined as the angle formed by the lines tangent to the caudal endplates of C2 and C7 in standing lateral radiographs (Figure 1). The functional spinal unit (FSU) angle was also examined on lateral radiographs, and was formed by the tangent lines drawn at the superior endplate of the cephalad vertebral body and at the inferior endplate of the caudal body. The range of motion (ROM) was determined by drawing lines between the superior endplate of the adjacent cephalad vertebral body and the inferior endplate of the adjacent caudal vertebral body in dynamic flexion/extension lateral images.
The distance between the vertebral endplate and implant shell on the lateral view was measured (Figure 2).
Statistical analysis
Statistical analyses were performed using SPSS software (SPSS Inc., version 22.0; Chicago, IL, USA). The significance of differences between measurements taken at baseline and at final follow-up was analyzed using the paired sample t-test. The independent t-test or chi-square test were used to identify significant differences between groups. Multivariate logistic regression analysis was used to determine risk factors related to SASD. In all analyses, significance was defined as P<0.05. Results are presented as mean ± standard deviation.
Results
The study population (n=90) consisted of 42 men and 48 women whose age was 43.3±5.9 years at the final follow-up (Table 1). Three patients were excluded due to incomplete radiographic or clinical data, and 8 patients were lost to follow-up. The follow-up period was 6.6±0.3 years. The BCDA was implanted at the C4-3, C4-5, C5-6, and C6-7 levels in 4, 18, 40, and 28 patients, respectively. At the final follow-up, there was no implant migration, subsidence, loosening, or other implant-related complications and no patient needed additional surgery, on either the arthroplasty level or adjacent levels, for recurrent symptoms. In all, 38 (42.2%) of the 90 studied patients developed postoperative SASD (Table 1). All the patients had significant improvement in neurological function during the follow-up period.
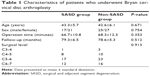  | Table 1 Characteristics of patients who underwent Bryan cervical disc arthroplasty |
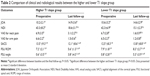
There were 28 and 62 patients in the high and low T1 slope groups, respectively. At the last follow-up, the high T1 and low T1 slope groups were significantly different in terms of SACS, FSU angle, FSU ROM, and rate of SASD (P<0.05). The patients in the high T1 group had more lordosis before the surgery and also experienced more SASD (Figure 3). The rate of SASD in the high T1 group (67.9%; 19/28) was significantly higher than that in the low T1 group (36.6%; 19/62). Both the NDI and VAS scores of the high T1 group were significantly greater than that of the low T1 group, although the VAS scores specifically for arm pain were comparable (Table 2).
The SASD and non-SASD groups were comparable in demographics, clinical outcomes, and JOA scores at the final follow-up (P>0.05). The NDI and VAS scores for neck pain were slightly higher in the SASD group than in the non-SASD group, but the difference did not reach significance. The T1 slopes of the SASD group (30.3°±2.6°) and non-SASD group (21.9°±3.1°) were also similar. The FSU ROM was relatively good at the final follow-up, but the FSU ROM of the SASD group (5.8°±1.6°) was significantly less than that of the non-SASD group (8.3°±2.7°). The preoperative FSU angles of the SASD and non-SASD groups were 0.2°±4.6° and 1.2°±3.2°, respectively, while at the final follow-up, the FSU angles were 3.6°±5.1° and 5.8°±2.1°, respectively (P<0.05). The endplate coverage discrepancy of the SASD group (residual space behind the prosthesis; 2.53±0.37 mm) was significantly greater than that of the non-SASD group (0.63±0.21 mm; P<0.05; Table 3).
To compare the relative influence of these variables on the rate of SASD, multiple logistic regression analysis was performed. With a P-value <0.1, in the univariate analysis the following were analyzed as dependent variables by a forward stepwise method: high T1 slope, FSU ROM, endplate coverage discrepancy, and FSU angle. The analysis determined that high T1 slope (odds ratio [OR] =2.848, 95% CI =1.342–6.033, P<0.05) and endplate coverage discrepancy (OR =1.032, 95% CI =1.009–1.076, P<0.05) were significant risk factors for SASD after BCDA, with high T1 slope conveying the greater relative risk.
Discussion
SASD after BCDA can adversely affect the mechanical dynamics of the cervical spine and clinical outcome. We investigated whether the preoperative T1 slope is associated with the development of SASD after BCDA, and followed up patients for close to 6 years. Clinical results of the BCDA were excellent, with no related complications or repeated surgeries. The overall rate of post-implant SASD was 42.2%, that is, 38 of 90 patients. According to the regression analyses, high T1 slope carried the highest relative risk for SASD, followed by endplate coverage discrepancy (residual space behind the prosthesis).
BCDA has the advantage of preserving ROM at the index level, compared with ACDF. If the motion of the Bryan disc is limited after severe degeneration, the Bryan disc itself may function similarly to the cage in ACDF.
SASD after BCDA is common, but its etiology remains unclear. In China, Zhang et al13 reported a 1.8% reoperation rate after BCDA during a 2-year follow-up, while the reoperation rate after ACDF was 5.7%. However, in a prospective study by Sasso et al14 with a 4-year follow-up, the rates of reoperation after BCDA or ACDF were comparable. Chang et al15 recently reviewed the rates of reoperation after fusion and arthroplasty, which were 6.0% and 3.1%, respectively. This highlights the difference in SASD rates associated with these procedures.
Theoretically, osteophyte formation and narrowing of the disc space due to spinal cord or nerve root compression may occur after arthroplasty, resulting in myelopathy or radiculopathy. However, in this present series, no patient required additional surgery for recurrent symptoms, on either the arthroplasty or adjacent levels, although SASD was observed in 38 (42.2%) of the 90 subjects. Rather, all the patients had significant improvement in neurological function. The NDI and VAS scores for neck pain of the patients in the SASD group were slightly higher than those of the patients in the non-SASD group, but the difference was not statistically significant. Therefore, an association between neck pain and SASD needs to be studied further.
Explanations for SASD after BCDA have been proposed,15,16 but its development appears to be multifactorial and the exact cause remains unclear. From our univariate analysis, the factor that carried the highest relative risk was high T1 slope. The T1 slope is considered a landmark for evaluating cervical sagittal balance and is closely associated with SACS for maintaining cervical horizontal balance.17,18 Knott et al17 found that a T1 slope >25° was associated with ≥10 cm of positive sagittal imbalance, and patients with a high T1 slope required greater lordosis and energy expenditure to attain a horizontal balance.
The effects of varying degrees of T1 slope at any particular SACS, and vice versa, may be profound. If a cervical spine had a higher T1 slope and lower SACS, it become bent over horizontally under a kyphotic force. On the other hand, patients with a lesser T1 slope need a moderately lower SACS to keep cervical sagittal balance. Loss of normal SACS may induce abnormal movement and accelerate degeneration of the cervical spine.
Cervical sagittal imbalance after surgery may risk pain and disability.19 In the present study, patients in the high T1 slope group had significantly higher NDI and neck pain scores, compared with patients in the low T1 slope group. A high T1 slope may be due to cervical sagittal imbalance. It is likely that the SACS cannot compensate sagittal balance at higher T1 slopes, whereas in patients with a low T1 slope, SACS is compensated. Furthermore, a high T1 slope may tend to aggravate postoperative FSU kyphosis, which accelerates degeneration of the cervical spine. FSU kyphosis limits ROM of the FSU and is associated with postoperative neck pain. The kyphotic force caused by uncompensated high T1 slope may fatigue the paravertebral muscles and accelerate SASD, resulting in greater postoperative neck pain.
In the present study, the modified surgical technique that we used and described should increase FSU lordosis and prevent segmental kyphosis. This modified technique increases the FSU angle and compensates sagittal balance in patients with a high T1 slope. Therefore, we suggest that appropriate overcorrection of FSU lordosis may be indicated for patients with a high T1 slope; during surgery, the anterior part of the endplate should be milled appropriately. It is recommended that the Bryan disc be inserted parallel to the angle of the disc space. This promotes hyperlordosis of the FSU, which compensates sagittal balance in patients with a high T1 slope.
From our univariate analysis of the risk factors for SASD after BCDA, we identified endplate coverage discrepancy as the second important risk factor after high T1 slope. Endplate coverage discrepancy means that there is residual space behind the prosthesis, which may provide conditions for osteophyte formation. The abnormal cervical biomechanics caused by endplate coverage discrepancy may encourage SASD after BCDA. The shortage in the metallic shell would cause exposure of the vertebral body endplate.
In the present study, the endplate coverage discrepancies of the SASD group and non-SASD groups were 2.53±0.37 mm and 0.63±0.21 mm, respectively, a significant difference between the groups. SASD may be due to inflammation of the vertebral body and prosthetic biomechanics after inappropriate surgical techniques. However, the metallic endplate shell can block ectopic bony outgrowth at the edge. Therefore, it is important to adapt the metallic shell to sufficiently cover the vertebral endplate. A detailed correlation between SASD and endplate coverage discrepancy needs further investigation.
It has been proposed that bone dust that remains after endplate preparation by the Bryan disc milling technique during surgery is the most important factor inducing new or enlarged osteophyte formation after BCDA.20,21 Alternatively, ossification may be a degenerative inflammatory reaction of normal bone and biomechanics of the device, rather than a surgical complication.7 Leung et al20 demonstrated a correlation between ossification and FSU ROM, with male sex and age as significant risk factors. Tu et al22 analyzed 107 levels of BCDA with a minimum 2-year follow-up, and found that surgical techniques influenced SASD and the FSU ROM after BCDA. In our present study, we found that the FSU ROM of the SASD and non-SASD groups was 5.8°±1.6° and 8.3°±2.7°, respectively. However, the multivariate logistic regression analysis did not indicate that the FSU ROM was a risk factor of SASD. This result may be due to the small number of patients in the study.
In this study, we have reported the influence of high T1 slope on clinical outcomes after BCDA, which may not be applicable to other cervical artificial discs prostheses. Furthermore, the study population is relatively small, which limits the statistical power of the conclusions. To know the exact cause of SASD, a larger group of patients treated with BCDA and a multi-segment operative technique are required. The specific mechanisms of endplate coverage discrepancy, and the insert angle in patients with high T1 slope, require further study. Biomechanical studies of the degenerative process in SASD after arthroplasty are needed to help identify pathogenesis. A prospective multi-center study with long-term follow-up would certainly provide more useful information.
Conclusion
This study found that risk factors of SASD after BCDA include high T1 slope and endplate coverage discrepancy. Patients with a high T1 slope have a smaller FSU angle and more neck pain after BCDA.
Disclosure
The authors report no conflicts of interest in this work.
References
Park MS, Kelly MP, Lee DH, Min WK, Rahman RK, Riew KD. Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine J. 2014;14(7):1228–1234. | ||
Phillips FM, Lee JY, Geisler FH, et al. A prospective, randomized, controlled clinical investigation comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion. 2-year results from the US FDA IDE clinical trial. Spine (Phila Pa 1976). 2013;38(15):E907–E918. | ||
McAfee PC, Cappuccino A, Cunningham BW, et al. Lower incidence of dysphagia with cervical arthroplasty compared with ACDF in a prospective randomized clinical trial. J Spinal Disord Tech. 2010;23(1):1–8. | ||
Nabhan A, Ishak B, Steudel WI, Ramadhan S, Steimer O. Assessment of adjacent-segment mobility after cervical disc replacement versus fusion: RCT with 1 year’s results. Eur Spine J. 2011;20(6):934–941. | ||
Zechmeister I, Winkler R, Mad P. Artificial total disc replacement versus fusion for the cervical spine: a systematic review. Eur Spine J. 2011;20(2):177–184. | ||
Qi M, Chen H, Cao P, Tian Y, Yuan W. Incidence and risk factors analysis of heterotopic ossification after cervical disc replacement. Chin Med J (Engl). 2014;127(22):3871–3875. | ||
Lee JH, Jung TG, Kim HS, Jang JS, Lee SH. Analysis of the incidence and clinical effect of the heterotopic ossification in a single-level cervical artificial disc replacement. Spine J. 2010;10(8):676–682. | ||
Kim HJ, Kelly MP, Ely CG, Dettori JR, Riew KD. The risk of adjacent-level ossification development after surgery in the cervical spine: are there factors that affect the risk? A systematic review. Spine (Phila Pa 1976). 2012;37(22 Suppl):S65–S74. | ||
Yi S, Shin DA, Kim KN, et al. The predisposing factors for the heterotopic ossification after cervical artificial disc replacement. Spine J. 2013;13(9):1048–1054. | ||
Walraevens J, Demaerel P, Suetens P, et al. Longitudinal prospective long-term radiographic follow-up after treatment of single-level cervical disk disease with the Bryan Cervical Disc. Neurosurgery. 2010;67(3):679–687; discussion 687. | ||
Yanbin Z, Yilong Z, Yu S, Feifei Z, Zhongjun L. Application of cervical arthroplasty with Bryan cervical disc: 10 years follow-up results in China. Spine (Phila Pa 1976). Epub 2015 Sep 1. | ||
Kim TH, Lee SY, Kim YC, Park MS, Kim SW. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976). 2013;38(16):E992–E997. | ||
Zhang X, Zhang X, Chen C, et al. Randomized, controlled, multicenter, clinical trial comparing BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion in China. Spine (Phila Pa 1976). 2012;37(6):433–438. | ||
Sasso RC, Anderson PA, Riew KD, Heller JG. Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am. 2011;93(18):1684–1692. | ||
Chang KE, Pham MH, Hsieh PC. Adjacent segment disease requiring reoperation in cervical total disc arthroplasty: a literature review and update. J Clin Neurosci. 2017;37:20–24. | ||
Sirikci M, Karaca S, Enercan M, et al. Radiologic and clinical outcome of the operated and adjacent segments following prodisc-C cervical arthroplasty after a minimum 24-month follow-up: a single surgeon center experience. Neurosurg Q. 2016;26(3):234–239. | ||
Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010;10(11):994–998. | ||
Lee SH, Kim KT, Seo EM, Suk KS, Kwack YH, Son ES. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech. 2012;25(2):E41–E47. | ||
Jang JS, Lee SH, Min JH, Kim SK, Han KM, Maeng DH. Surgical treatment of failed back surgery syndrome due to sagittal imbalance. Spine (Phila Pa 1976). 2007;32(26):3081–3087. | ||
Leung C, Casey AT, Goffin J, et al. Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial. Neurosurgery. 2005;57(4):759–763; discussion 759–763. | ||
Puzas JE, Miller MD, Rosier RN. Pathologic bone formation. Clin Orthop Relat Res. 1989;(245):269–281. | ||
Tu TH, Wu JC, Huang WC, Wu CL, Ko CC, Cheng H. The effects of carpentry on heterotopic ossification and mobility in cervical arthroplasty: determination by computed tomography with a minimum 2-year follow-up: clinical article. J Neurosurg Spine. 2012;16(6):601–609. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.