Back to Journals » Clinical Ophthalmology » Volume 11
Idiopathic polypoidal choroidal vasculopathy in Thai patients with clinical and angiographic choroidal neovascularization
Authors Bhoomibunchoo C, Thoongsuwan S, Rojanaporn D , Watanachai N , Jirarattanasopa P , Wongcumchang N, Amphornphruet A, Vongkulsiri S , Arayangkoon E
Received 31 October 2016
Accepted for publication 9 January 2017
Published 9 February 2017 Volume 2017:11 Pages 317—322
DOI https://doi.org/10.2147/OPTH.S126226
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Chavakij Bhoomibunchoo,1 Yosanan Yospaiboon,1 Somanus Thoongsuwan,2 Duangnate Rojanaporn,3 Nawat Watanachai,4 Pichai Jirarattanasopa,5 Nattapon Wongcumchang,6 Atchara Amphornphruet,7 Sritatath Vongkulsiri,8 Eakkachai Arayangkoon9
1Department of Ophthalmology, Faculty of Medicine, Khon Kaen University, Khon Kaen, 2Department of Ophthalmology, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, 3Department of Ophthalmology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, 4Department of Ophthalmology, Faculty of Medicine, Chiang Mai University, Chiang Mai, 5Department of Ophthalmology, Faculty of Medicine, Prince of Songkla University, Songkhla, 6Department of Ophthalmology, Faculty of Medicine, Thammasat University, Pathum Thani, 7Department of Ophthalmology, Rajavithi Hospital, Bangkok, 8Department of Ophthalmology, Phramongkutklao Hospital, Bangkok, 9Department of Ophthalmology, Mettapracharak Hospital, Nakhon Pathom, Thailand
Objective: This study aimed to study the prevalence and characteristics of idiopathic polypoidal choroidal vasculopathy (IPCV) in Thai patients with clinical and angiographic choroidal neovascularization (CNV).
Patients and methods: A consecutive case study of 140 patients presenting with CNV was conducted in nine large referral eye centers throughout Thailand. The demographic data, fundus photographs, fundus fluorescein angiography and indocyanine green angiography of the patients were analyzed.
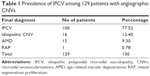
Results: Of 129 patients with clinical and angiographic CNV, IPCV was diagnosed in 100 patients (77.52%), idiopathic CNVs in 16 patients (12.40%) and age-related macular degeneration (AMD) in 12 patients (9.30%). Of the 107 eyes with IPCV, 90 eyes (84.11%) had both branching venous networks (BVNs) and polypoidal lesions. Most IPCV patients (93%) had unilateral involvement and were at a younger age than AMD patients. In all, 79 eyes (73.83%) had lesions found in the macular area, 14 eyes (13.08%) in the temporal to vascular arcades, ten eyes (9.35%) in the peripapillary area and four eyes (3.74%) in both macular and peripapillary areas. The clinical manifestations of IPCV at presentation were categorized into two patterns. There were 95 eyes (88.79%) of a hemorrhagic pattern and 12 eyes (11.21%) of an exudative pattern.
Conclusion: IPCV is the most common macular disease in Thai patients with CNV. Most IPCVs have both BVNs and polypoidal lesions located in the macular area and present with a hemorrhagic pattern.
Keywords: idiopathic polypoidal choroidal vasculopathy, prevalence, choroidal neovascularization, age-related macular degeneration
Introduction
In the past, patients with clinical presentation of choroidal neovascularization (CNV) were usually diagnosed as having age-related macular degeneration (AMD). With the advent of indocyanine green angiography (ICGA) and optical coherence tomography (OCT), idiopathic polypoidal choroidal vasculopathy (IPCV) has been reported increasingly worldwide.1 The abnormality is believed to originate in the inner choroid. The exact pathogenesis remains unclear; however, the pathologies involve dilated thin-walled aneurysmal vessels in the choroid.2 The characteristics of IPCV usually have two compositions: dilated branching venous networks (BVNs) and multiple terminal aneurysmal dilatation at the end of the venous networks.3 Clinically, the patients usually have recurrent subretinal hemorrhage, subretinal fluid, subretinal lipid and disciform macular scarring, which mimics AMD and other diseases characterized by the presence of CNV.4–6
Previous studies in Caucasians demonstrated that 4%–9.8% of patients presenting with CNV were finally diagnosed as having IPCV.7–10 Studies in Asians reported a much higher percentage.11–18 To the best of the authors’ knowledge, there was no such study in Thai patients. Therefore, this study was aimed to study the prevalence and characteristics of IPCV in Thai patients with clinical and angiographic CNVs.
Patients and methods
This multi-centered study was conducted from March 2015 to December 2015 in nine large referral eye centers throughout Thailand. Of these centers, six were in the central part (Siriraj Hospital, Ramathibodi Hospital, Rajavithi Hospital, Thammasat University Hospital, Phramongkutklao Hospital and Mettapracharak Hospital) and three were in the peripheral part of the country (Chiang Mai University Hospital in the Northern part, Khon Kaen University Hospital in the Northeastern part and Songklanagarind University Hospital in the Southern part). The study was approved by each institutional review board (Khon Kaen University Ethics Committee for Human Research; Siriraj Institutional Review Board, Faculty of Medicine Siriraj Hospital, Mahidol University; Ethical Clearance Committee on Human Rights Related to Research Involving Human Subjects, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Research Institute for Health Sciences, Chiang Mai University; Songklanagarind Research Ethics Committee; Human Ethics Committee of Thammasat University; Ethics Committee, Rajavithi Hospital, College of Medicine, Rangsit University; Institutional Review Board of the Royal Thai Army Medical Department; and Mettapracharak Hospital Research Ethics Committee). All patients signed written informed consent forms.
The patients were included into the study when they had clinical presentation of CNV such as subretinal or sub-pigment epithelial blood, subretinal fluid, subretinal lipid, subretinal pigment ring, irregular elevation of pigment epithelium, subretinal gray–white lesions, cystoid macular edema and a sea fan pattern of subretinal small vessels. The patients were excluded when they had previous ophthalmic laser treatment, including focal retinal laser, photodynamic therapy and transpupillary thermotherapy. Patients with angioid streaks, pathologic myopia, ocular histoplasmosis, rhegmatogenous retinal detachment, tractional retinal detachment, and uncontrolled glaucoma and patients who had opacification of the ocular media that precluded a clear fundus or angiographic examination were also excluded. Patients whose eyes had been operated on within 60 days prior to the study were also excluded.
All patients had a complete history and ocular examination with slit-lamp microscopy and fundus examination, fundus fluorescein angiography (FFA) with 5 mL of 10% sodium fluorescein and ICGA with 2 mL of 25 mg indocyanine green intravenously. Based on the EVEREST study,19 the patients were diagnosed as having IPCV by the presence of early subretinal focal ICGA hyperfluorescence (appearing within the first 6 minutes after the injection of indocyanine green) and, in addition, at least one of the following angiographic or clinical criteria: 1) polyp-like lesions; 2) hypofluorescent halos around lesions; 3) pulsation observed by video ICGA; 4) branching vascular networks of inner choroidal vessels; 5) submacular hemorrhage and 6) late-phase staining in the area of earlier hypofluorescent lesions.19
The primary outcome is the prevalence of patients finally diagnosed as having IPCV over patients with clinical and angiographic CNV. The secondary outcome is the characteristics of these IPCV patients. Statistical analysis was performed using SPSS for Windows version 16.0 (SPSS Inc., Chicago, IL, USA). The gender pattern in the IPCV patients was statistically compared to that in the AMD patients, and P-value was calculated by using Fisher’s exact test. In addition, the median and first and third quartile ranges of the ages in IPCV patients and AMD patients were statistically calculated and compared by Wilcoxon rank-sum test. The differences were considered significant when the P-value was <0.05.
Results
Of 140 patients in the study, 73 patients (52.14%) were males and 67 patients (47.86%) were females. In patients with clinical CNV, 100 patients (71.43%) were finally diagnosed as having IPCV; 16 patients (11.43%) as having idiopathic CNVs, including classic and occult forms; 12 patients (8.57%) as having AMDs; six patients (4.29%) as having chronic central serous retinopathy (CSR); two patients (1.43%) as having serous pigment epithelial detachment (PED); two patients (1.43%) as having macroaneurysm; one patient (0.71%) as having retinal angiomatous proliferation (RAP) and one patient (0.71%) as having retinal pigment epithelial (RPE) rip. Of 129 patients with clinical and angiographic CNVs, IPCVs accounted for 77.52%, whereas AMDs for 9.30% (Table 1).
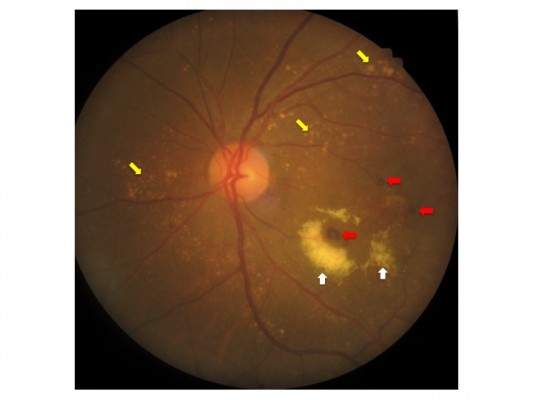
The characteristics of IPCV patients are demonstrated in Table 2. Of the 107 eyes with IPCV lesions, both eyes were equally affected and bilaterality was found in 7%. Most lesions were found in the macular area (Table 2). The clinical manifestations of IPCV at presentation were categorized into hemorrhagic and exudative patterns. Most fundus findings in this study were of a hemorrhagic pattern, which included hemorrhagic PED, subretinal hemorrhage, vitreous hemorrhage and serous retinal detachment or serous PED with adjacent subretinal hemorrhage (Figure 1). The remaining were of an exudative pattern, which included serous retinal detachment, serous PED, disciform scarring and subretinal fibrin. By ICGA findings, it was noted that most eyes had both BVNs and polypoidal lesions (Table 2 and Figure 2).
  | Table 2 The characteristics of patients with IPCV in the study |
The patients with IPCV had a median age of 59.5 years (first and third quartile ranges were 56 and 68), while the patients with AMD in this study had a median age of 74.5 years (first and third quartile ranges were 71.5 and 76.5). The difference in median age was statistically significant (P<0.001). The difference in gender prevalence, however, between IPCV and AMD groups was not statistically significant (P=0.375).
The characteristics of IPCV patients in this study were also compared to those in previous studies (Table 3). It was noted that most of the characteristics agree well with the previous Asian studies.
Discussion
PCV was previously thought to be a rare disease and to only affect black women.1,20 Although IPCV occurs more commonly in pigmented individuals, it is also found in white patients.7–10 Studies in Caucasians showed that IPCV occurred in 4%–9.8% of patients with CNVs7–10 compared to 22.2%–54.7% in Asian studies.11–18 The current study demonstrates the high prevalence of IPCV among patients presenting with clinical and angiographic CNVs. This finding agrees well with other previous Asian studies and confirmed that IPCV occurs more commonly in Asian patients presenting with CNVs.11–18 It is noted that the prevalence in this study is the highest in the literature. This may be attributed to the fact that this study was not only hospital based but also tertiary-care based. Ophthalmologists did not refer all CNV patients to the referral centers, especially those patients with mild or no symptoms. Only some difficult cases were referred. This may be one of the reasons that the prevalence in this study was higher than other studies.
Idiopathic CNV was the next common finding among 129 patients with angiographic CNV. Patients may develop idiopathic CNV and subsequent scarring in the absence of any other fundus abnormality or diseases known to be associated with CNV. These patients may represent a number of etiologies, including AMD without characteristic drusen or RPE abnormalities. AMD was the third most common finding with the prevalence of 9.3%. This seems to be contrary to Caucasian studies. Among patients with CNVs, Caucasian AMD occurred more common than IPCV,7–10 whereas this study showed IPCV much more common than AMD.
In the literature, IPCV was common in patients between the ages of 50 and 65 years.6,12,15,18,21 The present study also found IPCV in this age range. Furthermore, when comparing the ages of IPCV and AMD patients, it was found that IPCV patients were younger than AMD patients with a statistically significant difference. This finding agrees well with the study by Chang and Wu.18 They investigated the incidence of IPCV in 100 patients with presumed neovascular AMD and found that the mean age was younger in the PCV group than in the neovascular AMD group with a statistically significant difference.18
Previous studies demonstrated that IPCV in Caucasians had different clinical characteristics from those in Asians. Although initial studies showed that IPCV was found in African-American and Caucasian women more than men,1,20 some studies revealed no gender difference.7,8 In Asian populations, however, IPCV occurs more often in men than women.11,12,14,15,17,18,21–24 In this study, although it also occurred more in men than women, the difference was not statistically significant. The reason why Asian IPCV occurs commonly in men more than women may be attributed to an ethnic factor. It may be possible, however, to be a matter of chance. An epidemiologic study of a large series of IPCV patients including those in non-tertiary hospitals should be conducted to reduce the probability of chance and confirm the hypothesis of racial difference.
For the location of IPCV lesions, some Caucasian studies noted that the lesions were common in extramacular and peripapillary locations.7–9 On the contrary, Asian studies demonstrated that the lesions were more commonly located in the macular location.11–14,18–24 The current study also reported the more common macular location as reported in previous Asian studies.
Other characteristics of IPCV patients in this study were also compared to the previous studies. Although PCV is a bilateral disease, the majority of the patients had developed the lesion in one eye at presentation and subsequently in the other eye. This study demonstrated the unilateral involvement at presentation in 93% of patients. This finding agrees well with other previous studies.7,11,12,14,15,17,18,21–24
Fundus findings in PCV patients were of two patterns, exudative and hemorrhagic. In the exudative pattern, serous PED and retinal detachment were predominant at the macula. The hemorrhagic pattern was characterized by hemorrhagic PED and subretinal hemorrhage at the macula. Although some previous studies demonstrated that most of their patients showed an exudative pattern,15,21 most studies reported hemorrhagic patterns with polypoidal lesions. The current study also demonstrated a hemorrhagic pattern at presentation. ICGA revealed polypoidal lesions and branching vascular networks in most of the studies, including this study.6,8,10–12,18,22,24 The strength of this study is that it is a multi-centered study conducted in nine large referral eye centers throughout Thailand. Hence, the results represent a cross section of Thai IPCV patients. There are also some limitations. One of the limitations is that this study was conducted in tertiary-care hospitals so that the prevalence may be higher than expected. Another limitation is that since the study excluded the patients with ocular media opacity precluding a clear fundus or angiographic examination, there might be some IPCV patients with dense vitreous hemorrhage who were excluded. All these limitations might lead to an inaccurate prevalence. It gives, however, a whole picture of IPCV patients in Thailand that is similar to other Asian studies.
Conclusion
IPCV is the most common macular disease in Thai patients with clinical and angiographic CNVs. IPCV is more common in men, and often IPCV patients are younger than AMD patients. Most IPCVs have both BVNs and polypoidal lesions, located in the macular area and present with a hemorrhagic pattern.
Acknowledgments
The authors wish to thank Dr Yonrawee Piyacomn, Dr Tanapat Ratanapakorn (Department of Ophthalmology, Faculty of Medicine, Khon Kaen University) and Dr Adisai Varadisai (King Chulalongkorn Memorial Hospital, Bangkok) for contribution of patients’ data; Dr Kaewjai Thepsuthammarat (Clinical Epidemiology Unit, Faculty of Medicine, Khon Kaen University) for statistical analysis and Professor James A Will (University of Wisconsin, USA) for assistance with the English language presentation of the manuscript. This study has been presented in part at the 36th annual meeting of the Royal College of Ophthalmologists of Thailand, November 2015, Khon Kaen, Thailand.
Disclosure
The authors report no conflicts of interest in this work.
References
Imamura Y, Engelbert M, Iida T, Freund K, Yannuzzi L. Polypoidal choroidal vasculopathy: a review. Surv Ophthalmol. 2010;55(6):501–515. | ||
Lafaut BA, Aisenbrey S, Van den Broecke C, Bartz-Schmidt KU, Heimann K. Polypoidal choroidal vasculopathy pattern in age-related macular degeneration: a clinicopathologic correlation. Retina. 2000;20(6):650–654. | ||
Ciardella A, Donsoff I, Yannuzzi L. Polypoidal choroidal vasculopathy. Ophthalmol Clin North Am. 2002;15(4):537–554. | ||
Yannuzzi L, Freund K, Goldbaum M, et al. Polypoidal choroidal vasculopathy masquerading as central serous chorioretinopathy. Ophthalmol. 2000;107(4):767–777. | ||
Chuah C, Chee C. Idiopathic polypoidal choroidal vasculopathy as a cause of a disciform macular scar. Clin Exp Ophthalmol. 2003;31:163–165. | ||
Ahuja R, Stanga P, Vingerling J, Reck A, Bird A. Polypoidal choroidal vasculopathy in exudative and haemorrhagic pigment epithelial detachments. Br J Ophthalmol. 2000;84(5):479–484. | ||
Scassellati-Sforzolini B, Mariotti C, Bryan R, Yannuzzi LA, Giuliani M, Giovannini A. Polypoidal choroidal vasculopathy in Italy. Retina. 2001;21(2):121–125. | ||
Yannuzzi LA, Wong DW, Sforzolini BS, et al. Polypoidal choroidal vasculopathy and neovascularized age-related macular degeneration. Arch Ophthalmol. 1999;117(11):1503–1510. | ||
Ladas ID, Rouvas AA, Moschos MM, Synodinos EE, Karagiannis DA, Koutsandrea CN. Polypoidal choroidal vasculopathy and exudative age-related macular degeneration in Greek population. Eye (Lond). 2004;18(5):455–459. | ||
Lafaut BA, Leys AM, Snyers B, Rasquin F, De Laey JJ. Polypoidal choroidal vasculopathy in Caucasians. Graefes Arch Clin Exp Ophthalmol. 2000;238(9):752–759. | ||
Wen F, Chen C, Wu D, Li H. Polypoidal choroidal vasculopathy in elderly Chinese patients. Graefes Arch Clin Exp Ophthalmol. 2004;242(8):625–629. | ||
Kwok AK, Lai TY, Chan CW, Neoh EL, Lam DS. Polypoidal choroidal vasculopathy in Chinese patients. Br J Ophthalmol. 2002;86(8):892–897. | ||
Liu Y, Wen F, Huang S, et al. Subtype lesions of neovascular age-related macular degeneration in Chinese patients. Graefes Arch Clin Exp Ophthalmol. 2007;245(10):1441–1445. | ||
Song SJ, Youm DJ, Chang Y, Yu HG. Age-related macular degeneration in a screened South Korean population: prevalence, risk factors, and subtypes. Ophthalmic Epidemiol. 2009;16(5):304–310. | ||
Byeon SH, Lee SC, Oh HS, Kim SS, Koh HJ, Kwon OW. Incidence and clinical patterns of polypoidal choroidal vasculopathy in Korean patients. Jpn J Ophthalmol. 2008;52(1):57–62. | ||
Sho K, Takahashi K, Yamada H, et al. Polypoidal choroidal vasculopathy: incidence, demographic features, and clinical characteristics. Arch Ophthalmol. 2003;121(10):1392–1396. | ||
Maruko I, Iida T, Saito M, Nagayama D, Saito K. Clinical characteristics of exudative age-related macular degeneration in Japanese patients. Am J Ophthalmol. 2007;144(1):15–22. | ||
Chang YC, Wu WC. Polypoidal choroidal vasculopathy in Taiwanese patients. Ophthalmic Surg Lasers Imaging. 2009;40(6):576–581. | ||
Koh A, Lee WK, Chen LJ, et al. EVEREST study: efficacy and safety of verteporfin photodynamic therapy in combination with ranibizumab or alone versus ranibizumab monotherapy in patients with symptomatic macular polypoidal choroidal vasculopathy. Retina. 2012;32(8):1453–1464. | ||
Stern R, Zakov Z, Zegarra H, Gutman F. Multiple recurrent serosanguineous retinal pigment epithelial detachments in black women. Am J Ophthalmol. 1985;100(4):560–569. | ||
Anantharaman G, Ramkumar G, Gopalakrishnan M, Rajput A. Clinical features, management and visual outcome of polypoidal choroidal vasculopathy in Indian patients. Indian J Ophthalmol. 2010;58(5):399–405. | ||
Hou J, Tao Y, Li XX, Zhao MW. Clinical characteristics of polypoidal choroidal vasculopathy in Chinese patients. Graefes Arch Clin Exp Ophthalmol. 2011;249(7):975–979. | ||
Cackett P, Htoon H, Wong D, Yeo I. Haemorrhagic pigment epithelial detachment as a predictive feature of polypoidal choroidal vasculopathy in a Chinese population. Eye (Lond). 2010;24(5):789–792. | ||
Uyama M, Wada M, Nagai Y, et al. Polypoidal choroidal vasculopathy: natural history. Am J Ophthalmol. 2002;133(5):639–648. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.