Back to Journals » Patient Preference and Adherence » Volume 12
High treatment adherence, satisfaction, motivation, and health-related quality of life with fingolimod in patients with relapsing-remitting multiple sclerosis – results from a 24-month, multicenter, open-label Danish study
Authors Schreiber K , Kant M, Pfleger C, Jensen HB, Oesterberg O , Hald AR, Nielsen FK , Rubak S
Received 22 February 2018
Accepted for publication 26 April 2018
Published 29 June 2018 Volume 2018:12 Pages 1139—1150
DOI https://doi.org/10.2147/PPA.S166278
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Karen Schreiber,1 Matthias Kant,2 Claudia Pfleger,3 Henrik Boye Jensen,4 Ole Oesterberg,5 Anne Rieper Hald,5 Frederik K Nielsen,5 Sune Rubak6
1Department of Neurology, Rigshospitalet, Copenhagen University Hospital, Copenhagen, Denmark; 2Department of Neurology, Hospital of Southern Jutland, Soenderborg, Denmark; 3Department of Neurology, Aalborg University Hospital, Denmark; 4Department of Neurology, Kolding Hospital, Kolding, Denmark; 5Novartis Pharmaceutical, Copenhagen, Denmark; 6Department of Child and Adolescent Health, Aarhus University Hospital Skejby, Aarhus Denmark
Purpose: Treatment adherence is a prerequisite for treatment success and therefore an important consideration to assure that therapeutic goals are achieved both from a patient point of view and for optimal health care resource utilization. Published data on treatment adherence with fingolimod (Gilenya®) are limited. Therefore, this study investigated treatment adherence in patients with relapsing-remitting multiple sclerosis (RRMS) treated with fingolimod in Denmark.
Patients and methods: This was a 24-month, multicenter, open-label study, investigating treatment adherence, satisfaction, motivation, and health-related quality of life (QoL) in RRMS patients treated with fingolimod. In addition, the effect of a motivational interview support program on these measures was evaluated. Treatment adherence was assessed by pill count. Treatment satisfaction, motivation, and QoL were assessed by patient-reported outcomes (PROs).
Results: A total of 195 patients were enrolled in the study. A very high treatment adherence was observed during the entire study with no statistically significant difference between study visits before (99%) and after (97%) the motivational interview. In accordance, a high level of treatment satisfaction was found in the Treatment Satisfaction Questionnaire for Medication 9, which was scored high throughout the study with the highest scores seen for the convenience domain (ranging from 94.51 to 95.78). Furthermore, additional PROs demonstrated a high health-related QoL, a self-determined form of motivation for taking medication, and a patient perception of an autonomy supportive approach provided by the health care provider, at all study visits.
Conclusion: High levels of treatment adherence, satisfaction, motivation, and QoL were observed in Danish RRMS patients treated with fingolimod. As these positive measures were observed at all study visits and throughout the study, no effect of the motivational interview support program was found.
Keywords: Gilenya®, multiple sclerosis, treatment adherence, motivational interview, quality of life, Treatment Satisfaction Questionnaire for Medication
Introduction
Multiple sclerosis (MS) is a chronic, autoimmune demyelinating disease of the central nervous system (CNS) affecting more than 2.3 million people worldwide.1,2 The disease targets the myelin sheaths around nerves, leading to inflammation, myelin loss, and axonal destruction leading to disability. The most common form of MS, affecting around 85% of MS patients, is relapsing-remitting MS (RRMS), which is characterized by episodes of relapse followed by periods of remission. RRMS often develops into secondary progressive MS, where the symptoms gradually worsen and accumulate without a relapsing nature.3
Symptoms of MS vary in type and severity between patients and even within the same patient. Common symptoms include fatigue, visual disturbances, altered sensation, depression, numbness, weakness, bladder and bowel dysfunction, sleep disorders, cognitive impairment, and difficulties with mobility.1 Importantly, the disabling nature of the disease significantly impairs the quality of life (QoL) of the patients by interfering with their daily activities.4
Although MS is currently incurable, long-term treatment with disease-modifying therapies (DMTs) has been shown to reduce relapse rates and thus the risk of disability progression in RRMS. A broad panel of DMTs with different modes and frequencies of administration is available including different injectable, oral, and intravenous therapies.5
Poor adherence to long-term therapy for chronic illnesses, including MS, is a common problem.6,7 According to the World Health Organization (WHO), adherence among patients suffering from chronic diseases is as low as 50% in developed countries and probably even lower in developing countries.6 Specifically, for MS, rates of adherence to DMTs have been reported to range from as low as 28% up to 88%.8 Numerous factors contribute to this non-adherence in MS, for example, cognitive impairment and depression, fear of medicine administration and inconvenience of use, side effects, and insufficient caregiver support.7,9
For chronic diseases such as MS, administration of DMT as prescribed is a prerequisite for treatment success. In this regard, several studies have shown that adherent patients tend to have a lower risk of relapses, lower risk of hospital admission, fewer emergency visits, and fewer visits to their physician compared to nonadherent patients.10,11 Thus, adherence to a specific medication regimen is an important consideration to assure that therapeutic goals are achieved both from a patient point of view and considering health economy in terms of optimal health care resource utilization.
Fingolimod (Gilenya®; Novartis International AG, Basel, Switzerland) was the first oral, once daily DMT to gain regulatory approval for the treatment of RRMS. Fingolimod is a sphingosine-1-phosphate receptor modulator.12 The active metabolite fingolimod phosphate blocks the migration of lymphocytes from lymph nodes, thereby reducing the number of lymphocytes in peripheral blood, and hence reduces lymphocyte migration into the CNS. Fingolimod has demonstrated clinical efficacy in reducing relapses, delaying disability progression, and improving MRI and brain volume loss outcomes in phase 3 clinical trials.13
Given that adherence is key to the effectiveness of DMTs, a thorough understanding of adherence and medication-taking behavior to individual DMTs is paramount for optimal patient care and health care utilization. Published data on treatment adherence in RRMS patients treated with fingolimod are limited. This also applies to the level of treatment satisfaction, motivation, and QoL in these patients, all of which are important determinants for adherence to treatment. The present 24-month, multicenter, open-label study therefore investigated the adherence, treatment satisfaction, motivation, and health-related QoL in RRMS patients treated with fingolimod. In addition, the effect of a motivational interview support program including motivational interview training of the participating investigators on these measures was evaluated as was the safety of the treatment.
Patients and methods
Study design
This was a 24-month, multicenter, open-label study to investigate the treatment adherence, satisfaction, motivation, and QoL in RRMS patients treated with fingolimod. In addition, the effect of a motivational interview support program on these measures was evaluated. Patients were recruited from eight different MS clinics in Denmark. The patient database at each clinic served as the source of recruitment, thus all patients recruited had at least 6 months fingolimod treatment prior to enrollment in the study.
The study consisted of two phases: a 12-month observational run-in phase and a 12-month motivational interview phase where the effect of a motivational interview support program was evaluated (Figure 1). At the screening/baseline visit (visit 1), patients were evaluated for eligibility in the study, and if eligible, baseline assessments of treatment adherence, satisfaction, motivation, and health-related QoL were performed. After the screening/baseline visit, patients visited the clinic every 6 months (±1 month visit window) for post-baseline assessments of these parameters for a total study duration of 2 years.
The study was done in full accordance with Good Clinical Practice and the Declaration of Helsinki as adopted by the World Medical Association as well as Danish laws and regulations. Prior to conduct, the study was approved by both the National Committee on Health Research Ethics and the Danish data protection agency.
Motivational interview training
Motivational interviews were performed at each visit to the clinic in the motivational interview phase (ie, from visit 3 and onwards, Figure 1). Before the initiation of the motivational interview phase, the participating study personnel were trained in motivational interviewing (between visits 2 and 3 for all sites).
All health care professionals underwent a 2-day course in motivational interviewing techniques where they were trained in motivational interviewing by trainers who were certified members of the Motivational Interviewing Network. The effect of training was investigated by using Motivational Interviewing Treatment Integrity (MITI) coding 3.1.14 Additional booster trainings (2-hour sessions) were conducted locally at each clinic, 3–9 months after the initial training.
Motivational interviewing represents a specific method employed by the doctor to counsel their patients with the overall purpose of changing their behavior and increase the patients’ own motivation for a particular intervention, in this case intake of medication.15 The overall concept of motivational interviewing is for the doctors to create a supportive patient–doctor relationship rather than a compelling one. The technique may help the doctor with patients who are averse to behavioral changes, and it has been implemented successfully in several therapies.16
Study population
All patients gave written informed consent before entering the study. Patients were eligible for inclusion if they were aged 18–55 years, were diagnosed with RRMS according to the 2005 revised McDonald criteria,17,18 and had an expanded disability status scale (EDSS) score between 0 and 6.5. To avoid misinterpretation of adherence due to, for example, low tolerance leading to change of treatment or high adherence during the first treatment period, patients were required to having received fingolimod for a minimum of 6 months prior to inclusion. Patients who had received systemic corticosteroids or immunoglobulins within 1 month prior to screening, immunosuppressive medications or monoclonal antibodies (including natalizumab; Biogen, Cambridge, MA, USA) within 3 months prior to screening, or mitoxantrone within 6 months prior to screening were not eligible for the study.
Study assessments
Effect of motivational interview training of health care professionals
To assess the effect of motivational training of the health care professionals, MITI 3.1 scoring of the interviewers was performed before and after the training. In this regard, two independent educated trainers evaluated the implementation of motivational interviews at the study sites by scoring video records (15–20 min duration) of patient consultations taken before and after the motivational interview training.
Treatment adherence
Treatment adherence was assessed after 6, 12, 18, and 24 months in the study (Figure 1) based on pill count. Patients were asked to bring all their study medication to the clinic at the screening/baseline visit (visit 1) and at all post-baseline visits to the clinic. Adherence was then calculated as number of dispensed pills minus number of pills brought to the visit divided by the number of days between respective visits.
Treatment satisfaction
Treatment satisfaction was assessed after 6, 12, 18, and 24 months in the study (Figure 1) by using the abbreviated Treatment Satisfaction Questionnaire for Medication 9 (TSQM-9) score.19 The TSQM-9 assesses the overall level of satisfaction of patients with their treatment. It consists of nine questions focusing on the individual domains of effectiveness, convenience, and global satisfaction. Domain scores range from 0 to 100 with higher TSQM scores indicating greater treatment satisfaction within a particular domain.
Patient satisfaction with their medication has been shown to impact treatment-related behavior, including their likelihood of continuing to use their medication and to adhere to their treatment.20–22
Motivation
Controlled forms of motivation and amotivation have previously been linked to non-adherence to treatment.23,24 Motivation was assessed after 6, 12, 18, and 24 months in the study (Figure 1) by using the Treatment Self-Regulation Questionnaire25 (TSRQ) and the Health-Care Climate Questionnaire (HCCQ).26
Patients’ self-motivation toward taking their medication was assessed with the TSRQ assessing the degree to which behaviors tend to be self-determined. The TSRQ used in the present study consisted of 15 questions with a range of 1–7 and has been endorsed by the Behavior Change Consortium (BCC) investigators. The questionnaire has been validated across three different health behaviors (tobacco, diet, and exercise). There were three subscales to the scale: autonomous regulatory style (six questions), controlled regulatory style (six questions), and amotivation (three questions) with the autonomous regulatory style representing the most self-determined form of motivation. Each subscale score ranged between 1 and 7.
Physicians’ support to motivate the patient was assessed by the HCCQ. HCCQ assesses the degree to which patients experienced their health care providers to be autonomy supportive relative to controlling with respect to particular issues, behaviors, or treatments. HCCQ consists of five questions with a range from 0 to 6. The total HCCQ score varies from 0 to 30 with higher values indicating greater patient perception of an autonomy supporting versus controlling approach from the health care providers.
Health-related QoL
It was assumed that a high health-related QoL is linked to high treatment adherence as it has been used to measure drug efficacy.27,28 Health-related QoL was assessed after 6, 12, 18, and 24 months in the study (Figure 1) by using the 12-item short form questionnaire (SF-12) version 1.29 The SF-12 is a commonly used health-related QoL questionnaire, including 12 individual questions addressing the following eight domains: physical functioning, physical role, bodily pain, general health, vitality, social functioning, emotional role, and mental health scale. The questions were combined, scored, and weighted allowing for the generation of physical (physical functioning, role physical, bodily pain, and general health) and mental health (vitality, social functioning, role emotional, and mental health) summary scores ranging between 0 and 100, with 0 indicating the lowest level of health and 100 indicating the highest level.
The physical and mental component summary scores were compared with US norm-based scores, with scores >50 indicating better health.30
Safety
Safety was assessed descriptively and was based on the incidence and nature of adverse events (AEs), serious AEs (SAEs), and laboratory abnormalities (lymphocytes, alanine aminotransferase, and aspartate aminotransferase).
Statistical methods
Study size calculation was based on previous studies showing an expected improvement in adherence after motivational interviews of 5% units with a standard deviation of 25%.31,32 A total sample size of 230 patients was anticipated to have 80% statistical power to detect this effect size with a 5% level of significance and accounting for an expected dropout rate of 15%.
The safety analysis set (SAS) consisted of all patients who received at least one dose of fingolimod after inclusion in the study and who had at least one safety or efficacy measurement. The full analysis set (FAS) consisted of patients who were included in the safety set, who were diagnosed with RRMS, and who had at least one efficacy measurement at month 6. The per protocol set (PPS) consisted of patients who were included in the FAS and were deemed to have no major protocol violations that could interfere with the objectives of this study. Lack of adherence was not considered a major protocol deviation.
The primary efficacy endpoint was the mean treatment adherence (based on pill count) in the observational run-in phase versus the motivational interview phase. The primary efficacy analysis was based on the PPS. The difference in adherence between the two phases of the study was analyzed by two-sided t-tests performed on the 5% level of significance.
The upper limit of treatment adherence was set to 1 (100%); thus, adherence values above 1 were set to 1 in the statistical analyses. The secondary efficacy endpoints were mean TSQM-9, TSRQ, HCCQ, and SF-12 scores. The secondary efficacy analyses were based on the FAS. The secondary endpoints are presented with summary statistics for observed values.
Missing data were not imputed. Outliers were included in summary tables and were not handled separately. Available data from prematurely withdrawn patients were included in the analysis as far as possible.
Results
Patients
Between October 22, 2013, and April 30, 2014, a total of 195 patients were recruited for the study. This sample size is somewhat lower than the number of anticipated patients based on the power calculations described above. However, this sample size would assure the detection of an adherence improvement of 6% with a statistical power of 80%–90% with a standard deviation of 25%.
Of the total number of patients recruited into the study, 144 (73.8%) completed the study and 51 (26.2%) discontinued the study (Figure 2). The two main reasons for discontinuation from the study were patients who discontinued upon own request (17 patients, 8.7%) and patients for whom treatment was stopped by the treating physician (16 patients, 8.2% of which 7 [3.6%] were due to intolerance to treatment and 9 [4.6%] due to an AE).
  | Figure 2 Patient flow through the study. |
The study population comprised 130 (66.7%) females and 65 (33.3%) males (Table 1). The mean age at the screening visit was 41 years. Majority of patients were Caucasian (99.5%). The mean duration of MS from diagnosis to informed consent was 7.46 years and the mean EDSS score at the screening visit was 2.99.
  | Table 1 Patient demographics and baseline characteristics |
All the 195 enrolled patients were included in the SAS and thereby included in the analysis of safety and tolerability. For the observational run-in phase, a total of 10 subjects were excluded from the FAS population due to no efficacy measurements at month 6, resulting in an FAS of 185 patients. Of these patients, 59 had protocol deviations deemed to interfere with the study objectives leaving 126 subjects for the PPS. For the motivational phase, the FAS consisted of 159 patients and the PPS 105 patients.
Effect of motivational interview training of health care professionals – MITI scoring
Results from the MITI scoring showed a high degree of MITI with high levels of motivational interviewing spirit, empathy, and behavior with no pronounced difference between before and after the motivational interview training of the health care professionals (Table 2).
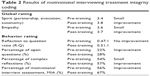  | Table 2 Results of motivational interviewing treatment integrity coding |
Treatment adherence
The mean and median treatment adherence are summarized in Table 3 for both the phases of the study. In general, a very high treatment adherence was observed during the entire study with no statistically significant difference between the observational run-in phase (99%) and the motivational interview phase (97%) (difference in adherence between phases was −0.0196 [−0.0453 to 0.0061]95% CI, p=0.1329).
  | Table 3 Treatment adherence |
Treatment satisfaction
High TSQM-9 scores were observed already at baseline, and they remained high for the entire duration of the study across all TSQM domains with no noteworthy difference between the two phases of the study (Figure 3). The highest satisfaction scores were seen for the convenience domain (ranging from 94.51 to 95.78).
Treatment motivation
The degree to which patients tended to take their medication in an autonomous (self-determined), controlled regulatory or amotivation style is depicted in Figure 4. The data showed that the patients tended to have a more self-determined form of motivation for taking their treatment compared to a controlled or amotivation form throughout the study.
The mean total HCCQ score was generally high during the study with no pronounced difference between the two phases of the study ranging between 26.33 at baseline and 27.69 at month 24 (visit 5) (Figure 5). Thus, the patients generally had a perception of their health care providers providing an autonomy support.
Health-related QoL
The mean SF-12 physical component summary score remained fairly constant throughout the study varying around a value of 45 (range: 44.49–45.91) (Figure 6). Likewise, the mean SF-12 mental component summary score also remained within the same level throughout the study varying around a value of ~50 (range: 49.79–51.26).
Both the physical and mental component summary scores were a little lower, yet comparable, than the average for the general population in the United States.
Safety
Overall, treatment with fingolimod was well tolerated, and the observed AEs were consistent with what has previously been reported with fingolimod.
A total of 116 of 195 patients (59.5%) reported 228 AEs during the study and 46 of the patients (23.6%) reported AEs considered related to the treatment. Of all the patients, 11 patients (5.6%) discontinued treatment due to 12 AEs. The most frequently reported AEs were within the system organ class “infections and infestations” with 64 of the patients (32.8%) reporting such events, and with pneumonia, cystitis, and influenza representing the most frequently reported preferred terms. A total of 14 patients (7.2%) reported 19 SAEs of which four were considered as related to the treatment (breast cancer, intentional overdose, malignant melanoma, and neoplasm). No deaths were reported during the study, and there were no clinically significant findings from safety laboratory assessments.
Discussion
Poor adherence to long-term therapy is a well-known problem in MS.7 Since adherence is imperative for treatment outcome, it is important to consider and evaluate adherence as well as factors related to adherence to a particular medication to assure that therapeutic goals are achieved, to minimize negative impacts of disease activity on RRMS patients and to reduce unnecessary costs on society to treat disease exacerbations.
Published data on treatment adherence with fingolimod are limited. Therefore, the present study investigated treatment adherence as well as parameters closely related to adherence, that is, treatment satisfaction, motivation, and health-related QoL, in RRMS patients treated with fingolimod in Denmark. In addition, since motivational interviews have previously shown to increase patients’ adherence to treatment,15 the effect of a motivational interview support program on these measures was also evaluated.
The results demonstrated a very high level of adherence to fingolimod treatment during the entire study with no statistically significant difference between the observational run-in phase (99%) and the motivational interview phase (97%). These adherence levels are somewhat higher than levels published for other types of DMTs in MS which have been reported to range from as low as 28% up to 88%.8 Generally, the adherence to fingolimod treatment has been higher than other oral DMTs for MS.33,34 In addition, the adherence levels found here are also higher than the levels found for the minority populations of Hispanic and African American MS patients treated with fingolimod.35 In this regard, it should be emphasized that the study includes a limited number of patients and concerns only MS patients treated in Danish MS clinics, and there may be significant differences to other MS clinics with fewer resources to treat these patients.
The results presented here should be considered within the context of an observational, open-label, non-randomized study design, in which the patients were drawn from 8 of 10 possible Danish MS clinics. Participants agreeing to participate may tend to score higher on patient-reported outcomes (PROs) and be more adherent compared to a more general MS population. The discontinuation rate was 26.2% during the 24 months which limit longitudinal interpretations of the study; however, this discontinuation rate should be expected based on experiences from the Phase III study program where 19%36 to 32%37 was seen (both studies were 24 months studies).
The primary endpoint was adherence as measured by pill count. Thus, patient’s medication was counted at every visit to the clinic. In turn, there is an inherent risk of incomplete return of unused fingolimod as well as fingolimod capsules that were lost and thus never taken. Some patients may have difficulties explaining how and why they lost these rather expensive capsules and have a desire to appear adherent in the eyes of their doctor. Thus, potential social desirability bias of the patients may have led to an overestimation of adherence.
In accordance with the high adherence levels, a high treatment satisfaction with fingolimod, reflected by high TSQM-9 scores, was observed throughout the study with the highest TSQM-9 scores seen for the convenience domain (ranging from 94.51 to 95.78). Furthermore, high mean SF-12 physical and mental component summary scores, comparable to those for the general population in the United States,30 were observed throughout the study indicating a high self-reported health-related QoL of the fingolimod-treated patients. In addition, results from the TSRQ and HCCQ indicated that patients were predominantly self-determined (as compared to being controlled) in their form of motivation for taking their medication and that they mainly felt that their health care provider used an autonomy supportive approach when meeting them. In this regard, it has previously been observed that patients treated with fingolimod have significant improvements in several self-reported outcomes compared to patients who continue injectable DMTs, including QoL and TSQM.38 Thus, the high baseline adherence levels observed in this study could be partly explained by a high satisfaction with fingolimod as well as a high treatment motivation and QoL of the included patients. As satisfaction, motivation, and QoL remained high throughout the study, this in part explains high adherence.
It should be mentioned that one of the inclusion criteria for this study was that patients were required to having received fingolimod for a minimum of 6 months prior to inclusion. This was introduced to avoid misinterpretation of adherence due to, for example, low tolerance leading to change of treatment or high adherence during the first treatment period. However, this inclusion criteria may also have introduced some selection bias, since only stable, well-treated patients were selected for the study, which could potentially have led to an overestimation of the assessed PROs.
An additional purpose of the study was to investigate the effect of a motivational interview support program on treatment adherence. Motivational interviews have previously been shown to have a positive effect on treatment adherence in MS,39 and it was thus highly relevant to investigate whether this could promote adherence in this patient population as well. However, the results showed no pronounced effect of a motivational interview on any of the parameters investigated, which is probably the result of these measures being high already at baseline leaving no room for improvements. Accordingly, results from the MITI scoring showed that the health care professionals were highly skilled in motivational interviewing already before the motivational interview training, thus probably partly explaining the lack of effect on adherence.
These data could suggest that Danish MS patients have a high degree of support in the health care system providing help to cope with their chronic disease which partly could explain their high adherence as observed in the present study.
Regarding safety, treatment with fingolimod was found to be well tolerated and no new and unexpected safety signs were reported.
Conclusion
This 24-month open-label study demonstrated high levels of treatment adherence as well as treatment satisfaction, motivation, and health-related QoL in a Danish cohort of RRMS patients treated with fingolimod. Due to the high level of treatment adherence already from baseline, no effects of a motivational interview support program could be demonstrated.
Acknowledgments
Medical writing services were provided by Sidse Ørnbjerg Würtz, PhD, and owner of Medical Writing by Sidse Ørnbjerg Würtz, Biskop Svanes Vej 47, 3460 Birkeroed, Denmark. This study was funded by Novartis Pharma AG, Basel, Switzerland.
Author contributions
All authors contributed to the design and execution of the study and participated in the analysis and interpretation of the data. In addition, all authors provided written input to the manuscript and participated in critical review, revision, and final approval of the manuscript. All the authors agree to be accountable for all aspects of the work.
Disclosure
Karen Schreiber has served on the scientific advisory board for Biogen Idec and has received honoraria for lecturing and support for congress participation from Biogen Idec, Genzyme, Teva, Merck, and Novartis. Matthias Kant has served on the scientific advisory board for Biogen Idec and Novartis and has received honoraria for lecturing and support for congress participation from Biogen Idec, Genzyme, Teva, and Novartis. Claudia Pfleger has served on the scientific advisory board for Biogen Idec, Novartis, Genzyme, and Teva and has received support for congress participation from Biogen Idec, Teva, and Novartis. Henrik Boye Jensen has served on the scientific advisory board for Biogen Idec, Novartis, and Genzyme and has received honoraria for lecturing and support for congress participation from Biogen Idec, Teva, and Novartis. Sune Rubak has served on the scientific advisory board for Novartis and has received honoraria for lecturing from Novartis. Ole Oesterberg, Anne Rieper Hald, and Frederik Nielsen are employees of Novartis. The authors report no other conflicts of interest in this work.
References
National Multiple Sclerosis Society. Multiple Sclerosis FAQs. Available from: http://www.nationalmssociety.org/What-is-MS/MS-FAQ-s. Accessed March 18, 2016. | ||
Lemus HN, Warrington AE, Rodriguez M. Multiple sclerosis: mechanisms of disease and strategies for myelin and axonal repair. Neurol Clin. 2018;36:1–11. | ||
Wingerchuk DM, Carter JL. Multiple sclerosis: current and emerging disease-modifying therapies and treatment strategies. Mayo Clin Proc. 2014;89:225–240. | ||
Kargiotis O, Paschali A, Messinis L, et al. Quality of life in multiple sclerosis: effects of current treatment options. Int Rev Psych. 2010;22:67–82. | ||
Wingerchuk DM, Weinshenker BG. Disease modifying therapies for relapsing multiple sclerosis. BMJ. 2016;354:i3518. | ||
Sabaté E, editor. Adherence to Long-Term Therapies: Evidence for Action. Geneva: World Health Organization; 2003. Available from: http://www.who.int/chp/knowledge/publications/adherence_report/en/index.html. Accessed December 7, 2017. | ||
Patti F. Optimizing the benefit of multiple sclerosis therapy: the importance of treatment adherence. Patient Prefer Adherence. 2010;4:1–9. | ||
Munsell M, Frean M, Menzin J, Phillips AL. An evaluation of adherence in patients with multiple sclerosis newly initiating treatment with a self-injectable or an oral disease-modifying drug. Patient Prefer Adherence. 2017;11:55–62. | ||
Higuera L, Carlin CS, Anderson S. Adherence to disease-modifying therapies for multiple sclerosis. J Manag Care Spec Pharm. 2016;22:1394–1401. | ||
Steinberg SC, Faris RJ, Chang CF, et al. Impact of adherence to interferons in the treatment of multiple sclerosis – a non-experimental, retrospective, cohort study. Clin Drug Investig. 2010;30:89–100. | ||
Tan H, Cai Q, Agarwal S, Stephenson JJ, Kamat S. Impact of adherence to disease-modifying therapies on clinical and economic outcomes among patients with multiple sclerosis. Adv Ther. 2011;28:51–61. | ||
European Medicines Agency. Summary of Product Characteristic for Fingolimod. Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/002202/human_med_001433.jsp&mid=WC0b01ac058001d125. Accessed February 1, 2018. | ||
Ziemssen T, Medin J, Couto CAM, Mitchell CR. Multiple sclerosis in the real world: a systematic review of fingolimod as a case study. Autoimmun Rev. 2017;16:355–376. | ||
Moyers TB, Martin T, Manuel JK, et al. Assessing competence in the use of motivational interviewing. J Subst Abuse Treat. 2005;28:19–26. | ||
Rollnick S, Miller WR. What is motivational interviewing? Behav Cogn Psychother. 1995;23:325–334. | ||
Rubak S, Sandbæk A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55:305–312. | ||
Polman CH, Reingold SC, Edan G, et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol. 2005;58:840–846. | ||
Lublin FD, Reingold SC. Defining the clinical course of multiple sclerosis: results of an international survey. Neurology. 1996;46:907–911. | ||
Bharmal M, Payne K, Atkinson MJ, et al. Validation of an abbreviated Treatment Satisfaction Questionnaire for Medication (TSQM-9) among patients on antihypertensive medications. Health Qual Life Outcomes. 2009;27:36. | ||
Zhang Z, Gerstein DR, Friedmann PD. Patient satisfaction and sustained outcomes of drug abuse treatment. J Health Psychol. 2008;13:388–400. | ||
Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1:189–199. | ||
DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40:794–811. | ||
Williams GC, Deci EL, Ryan RM. Improving patients’ health through supporting the autonomy of patients and providers. In: Delci EL, Ryan M, editors. Handbook of Self-Determination Research. Rochester, NY: University of Rochester Press; 2002:233–254. | ||
Williams GC, Deci EL, Ryan RM. Building health-care partnerships by supporting autonomy: promoting maintained behavior change and positive health outcomes. In: Suchman AL, Hinton-Walker P, Botelho R, editors. Partnerships in Healthcare: Transforming Relational Process. Rochester, NY: University of Rochester Press; 1998:67–87. | ||
Levesque CS, Williams GC, Elliot D, et al. Validating the theoretical structure of the Treatment Self-Regulation Questionnaire (TSRQ) across three different health behaviors. Health Educ Res. 2007;22:691–702. | ||
Gremigni P, Sommaruga M, Peltenburg M. Validation of the Health Care Communication Questionnaire (HCCQ) to measure outpatients’ experience of communication with hospital staff. Pat Educ Counsl. 2008;71:57–64. | ||
Bowling A. Measuring Disease: A Review of Disease Specific Quality of Life Instruments. Buckingham, Philadelphia: Philadelphia Open University Press. 1995:1–19. | ||
Johannesson M. Economic evaluation of drugs and its potential uses in policy making. Pharmacoeconomics. 1995;8:190–198. | ||
Ware JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. | ||
Janzen W, Turpin KVL, Warren SA, Marrie RA, Warren KG. Change in the Health-Related Quality of Life of multiple sclerosis patients over 5 years. Int J MS Care. 2013;15:46–53. | ||
Golin CE, Earp J, Tien HC, Stewart P, Porter C, Howie L. A 2-arm, randomized, controlled trial of a motivational interviewing-based intervention to improve adherence to antiretroviral therapy (ART) among patients failing or initiating ART. J Acquir Immune Defic Syndr. 2006;42:42–51. | ||
Ogedegbe G, Chaplin W, Schoenthaler A, et al. A practice-based trial of motivational interviewing and adherence in hypertensive African Americans. Am J Hypertens. 2008;21:1137–1143. | ||
Johnson KM, Zhou H, Lin F, Ko JJ, Herrera V. Real-world adherence and persistence to oral disease-modifying therapies in multiple sclerosis patients over 1 year. J Manag Care Spec Pharm. 2017;23:844–852. | ||
Bergvall N, Petrilla AA, Karkare SU, et al. Persistence with and adherence to fingolimod compared with other disease-modifying therapies for the treatment of multiple sclerosis: a retrospective US claims database analysis. J Med Econ. 2014;17:696–707. | ||
Williams MJ, Johnson K, Trenz HM, et al. Adherence, persistence, and discontinuation among Hispanic and African American patients with multiple sclerosis treated with fingolimod or glatiramer acetate. Curr Med Res Opin. 2018;34(1):107–115. | ||
Kappos L, Radue EW, O’Connor P, et al. A placebo-controlled trial of oral fingolimod in relapsing multiple sclerosis. N Engl J Med. 2010;362:387–401. | ||
Calabresi PA, Radue EW, Goodin D, et al. Safety and efficacy of fingolimod in patients with relapsing remitting multiple sclerosis (FREEDOMS II): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Neurol. 2014;13:545–556. | ||
Fox E, Edwards K, Burch G, et al. Outcomes of switching directly to oral fingolimod from injectable therapies: Results of the randomized, open-label, multicentre, Evaluate Patient OutComes (EPOC) study in relapsing multiple sclerosis. Mult Scler Relat Dis. 2014;3:607–619. | ||
Caon C, Saunders C, Smrtka J, Baxter N, Shoemaker J. Injectable disease-modifying therapy for relapsing-remitting multiple sclerosis: a review of adherence data. J Neuro Nurse. 2010;S42:5–9. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.