Back to Journals » ClinicoEconomics and Outcomes Research » Volume 16
Racial and Ethnic Differences in Initiation and Discontinuation of Antiarrhythmic Medications in Management of Atrial Fibrillation
Authors Kipp R, Herzog LO , Khanna R , Zhang D
Received 1 February 2024
Accepted for publication 19 March 2024
Published 27 March 2024 Volume 2024:16 Pages 197—208
DOI https://doi.org/10.2147/CEOR.S457992
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Samer Hamidi
Ryan Kipp,1 Lee-or Herzog,2 Rahul Khanna,3 Dongyu Zhang3
1Division of Cardiovascular Medicine, Department of Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI, USA; 2Franchise Health Economics and Market Access, Johnson and Johnson, Irvine, CA, USA; 3MedTech Epidemiology and Data Sciences, Johnson and Johnson, New Brunswick, NJ, USA
Correspondence: Ryan Kipp, Division of Cardiovascular Medicine, Department of Medicine, University of Wisconsin School of Medicine and Public Health, 600 Highland Ave, Madison, WI, 53792, USA, Tel +608-265-4188, Email [email protected]
Background: Atrial fibrillation (AF) is associated with considerable morbidity and mortality. Timely management and treatment are critical in alleviating AF disease burden. There is significant heterogeneity in patterns of AF care. It is unclear whether there are racial and ethnic differences in treatment of AF following antiarrhythmic drug (AAD) prescription.
Methods: Using the Optum Clinformatics Data Mart-Socioeconomic Status database from January, 2009, through March, 2022, multivariable logistic regression techniques were used to examine the impact of race and ethnicity on rate of AAD initiation, as well as receipt of catheter ablation within two years of initiation. We compared AAD discontinuation rate by race and ethnicity groups using Cox regression models. Log-rank analyses were used to examine the rate of AF-related hospitalization.
Results: Among 143,281 patients identified with newly diagnosed AF, 30,019 patients (21%) were initiated on an AAD within 90 days. Patients identified as Non-Hispanic Black (NHB) were significantly less likely to receive an AAD compared to Non-Hispanic White patients (NHW) (Odds Ratio [OR] 0.90, 95% confidence interval [CI] 0.85– 0.94). Compared to NHW, Hispanic (Hazard Ratio [HR] 1.08, 95% CI 1.02– 1.14) and Asian patients (HR 1.17, 95% CI 1.06– 1.29) have a higher rate of AAD discontinuation. Following AAD initiation, NHB patients were significantly more likely to have an AF-related hospitalization (p < 0.01). However, NHB patients were significantly less likely to receive ablation compared to NHW (HR 0.83, 95% CI 0.70– 0.97), and less likely to change AAD (p < 0.01).
Conclusion: Patients identified as NHB are 10% less likely to receive an AAD for treatment of newly diagnosed AF. Compared to NHW, Hispanic and Asian patients were more likely to discontinue AAD treatment. Once initiated on an AAD, NHB patients were significantly more likely to have an AF -related hospitalization, but were 17% less likely to receive ablation compared to NHW patients. The etiology of, and interventions to reduce, these disparities require further investigation.
Keywords: atrial fibrillation, cardiovascular disease, health disparity, epidemiology, real-world data
Introduction
Rhythm control for management of atrial fibrillation (AF), particularly with ablation, is increasingly recognized as a tool to reduce the risk of heart failure, hospitalization, stroke, and death.1,2 Due to these benefits, there has been a steady annual increase in the number of AF ablations performed.3,4 While management of AF with catheter ablation (CA) avoids the long-term risk of antiarrhythmic drugs (AADs) and facilitates improved rhythm control, AADs remain a mainstay of contemporary AF management.
Prior investigations have suggested that patients living in the United States (US) who identified as Black and those with lower incomes were significantly less likely to receive rhythm control medication for management of atrial fibrillation.4 It is unclear how race and ethnicity impact treatment decisions following AAD initiation for rhythm management of AF. The objective of this study was to investigate the impact of race and ethnicity on the outcomes and management decisions for newly diagnosed AF in the United States. Prior studies suggest that disparities in prevention and treatment of AF are substantial across different racial and ethnic groups, with racial and ethnic minorities having less access to healthcare resources.5 Therefore, we hypothesized that, compared to patients identified as non-Hispanic White, patients identified as non-Hispanic Black initiated on an AAD would be less likely to change AAD or receive an ablation, despite a higher rate of AF-related hospitalizations.
Methods
Data Source and Study Population
This study is a retrospective analysis of the Optum Clinformatics Data Mart-Socioeconomic Status (SES) Database from January, 2009, to March, 2022. This database includes deidentified administrative claims of individuals with commercial insurance or Medicare Advantage health plans. The Optum database includes inpatient, outpatient, and pharmacy claims from ~18 million patients with annual healthcare coverage.6 The Optum Clinformatics Data Mart-SES Database provides socio-economic information (eg, education and income) and location information for individuals with both medical and pharmacy coverage at the US Census Division level.7 This analysis of the Optum Clinformatics database was conducted under an exemption from Institutional Review Board oversight for US-based studies using de-identified healthcare records, as dictated by Title 45 Code of Federal Regulations (45 CFR 46.101(b)(4)) (https://www.govinfo.gov/content/pkg/CFR-2011-title45-vol1/pdf/CFR-2011-title45-vol1.pdf). As Optum data does not contain direct identifiers of individuals, employers, households, or providers, Institutional Review Board approval was waived.
Individuals who met the following criteria were included for the assessment of AAD initiation: (1) had ≥2 medical services visits with AF as the primary diagnosis between January 1, 2010, and December 31, 2019 (with the first such visit considered as the index visit); (2) the age at index was between 21 and 80 years; (3) had continuous enrollment for at least 12 months before the index visit; (4) had no AF diagnosis and no AAD prescription (amiodarone, dofetilide, dronedarone, flecainide, propafenone, sotalol, and disopyramide) in the 12 months before the index visit; and (5) had continuous enrollment for at least 24 months following the index visit. AF was identified by the International Classification of Diseases, Ninth Revision (ICD-9) code 427.31; or the ICD-10 codes I48.0, I48.1, I48.2, I48.91.
For assessing AAD discontinuation, the following additional criteria were applied: (1) initiated AAD within 90 days after the index AF visit and (2) had continuous enrollment for at least 24 months after AAD initiation. After applying study criteria, a total of 143,281 and 29,620 patients were included for AAD initiation and discontinuation analysis, respectively. Supplemental Figure 1 depicts the study inclusion and exclusion criteria.
Study Outcomes
The primary outcome of interest was AAD initiation within 90 days of AF diagnosis, which was assessed on the basis of an AAD prescription filled within 90 days of index AF visit. Discontinuation was classified based on a gap of greater than 90 days between AAD refills at any point within the two‐year period after AAD initiation.
Secondary outcomes included rate of AF and cardiovascular-related hospitalization, rate of switching AAD, and receipt of CA within two years of AAD initiation. AF-related hospitalization was identified as a hospitalization where the primary diagnosis was AF. Cardiovascular-related hospitalization was identified as a hospitalization where the primary diagnosis was coronary artery disease, heart failure, cardiomyopathy, cardiac arrhythmia, or cerebral hemorrhage or stroke (ICD codes are present in Supplemental Table 1). Switching AAD was identified by a prescription for a different AAD than originally prescribed. Receipt of CA was identified by the use of Current Procedural Terminology (CPT) code 93,656 and/or International Classification of Diseases, Tenth Revision, Procedural Coding System (ICD-10-PCS) codes (02553ZZ, 02563ZZ, 02573ZZ, 02583ZZ, 025K3ZZ, 025L3ZZ, 025M3ZZ, 025S3ZZ, 025T3ZZ), or ICD-9-PCS codes (37.34).
Study Variables
Race and ethnicity were the main independent variables of interest and categorized as non-Hispanic White (NHW), non-Hispanic Black (NHB), Hispanic, Asian, and Other within the Optum dataset. We combined responses of unknown race and ethnicity and missing responses into “Other” category. Patients’ socio-demographics included age at index AF visit, sex, geographic region, education, and household income. Geographic regions were categorized based on the US Census Bureau regions: Midwest, Northeast, South, and West.8 Education was classified into high school or lower, without a bachelor degree, and bachelor or higher, and annual household income was classified into <$50k, $50k-$99.9k, ≥$100k. Insurance type (Medicare, commercial insurance, both), insurance plan (Health Maintenance Organization [HMO] or Exclusive Provider Organization [EPO], Preferred Provider Organization [PPO], Point of Service [POS] or indemnity, other), and setting of AF diagnosis (inpatient and outpatient) were also included as study covariates. Subtypes of AF were ascertained via the ICD-10 codes (paroxysmal: I48.0, persistent: I48.1x) for incident AF patients diagnosed after October 2015.
Statistical Analysis
Descriptive characteristics were reported for patients with newly diagnosed AF (N = 143,281). Chi-square tests were used to assess if AAD initiation rates varied by race and ethnicity. A multivariable logistic regression model, which treated AAD initiation as the outcome, was used to estimate adjusted odds ratio (OR) and 95% confidence interval (CI) for AAD initiation by race and ethnicity. In addition to race and ethnicity (considered as the main independent variable of interest), the regression model adjusted for age, sex, education, income, region, CHA2DS2-VASc Score, Elixhauser Comorbidity Index, and CA receipt. The selection of covariates was based on previously published literature and a priori knowledge regarding their relationships with the exposure (race and ethnicity) and outcome of interest.4,9–13
We descriptively summarized the numbers and percentages of AAD discontinuation within two years of the first AAD prescription. Chi-square tests were used to assess if discontinuation rates varied by race and ethnicity and Kaplan–Meier curves were used to visualize the rate of continuation (1-discontinuation rate) by race and ethnicity during the two-year follow-up. Log rank test was used to compare discontinuation rate across race and ethnicity groups. A multivariable Cox proportional hazards regression model, which treated AAD discontinuation as the dependent variable, was used to examine the association between AAD discontinuation and race and ethnicity (adjusted hazard ratio (HR) and 95% CI reported). In the analysis, patients entered the risk set once they initiated AAD and the follow-up ended at the end of two-year period or AAD discontinuation, whichever occurred first. The model was adjusted for age, sex, education, income, region, CHA2DS2-VASc Score, Elixhauser Comorbidity Index, and CA receipt; the rationale of covariates selection was the same as the aforementioned logistic regression model. The proportional hazards assumption14 was assessed on the basis of scaled Schoenfeld residuals, and there was no violation of this assumption. To explore if the association between race and ethnicity and AAD initiation and discontinuation varied by gender, age, or socioeconomic status, subgroup analyses by sex, age, and annual household income (≤59k vs ≥60k), respectively, were conducted. The choice of the income cutoff was based on the US median household income between 2010–201915–17 and equivalence of sample size in two subgroups.
Kaplan–Meier curves and log rank tests were used to compare the rate of AF and cardiovascular hospitalization within two years of AAD initiation across race and ethnicity groups. The rate of AAD change was compared using chi-squared tests. The receipt of CA within two years of AAD initiation was also compared using chi-squared and multivariable cox proportional hazards regression (adjusted for all previously listed covariates).
To explore the stability of association for race and ethnicity, two sets of sensitivity analyses were conducted for multivariable models estimating effect measure for AAD initiation, AAD discontinuation, and CA receipt after initiation. In the first set of sensitivity analysis, we adjusted for AF subtype in the model. In the second set of sensitivity analysis, we adjusted for individual health conditions that could impact the outcome (obesity, congestive heart failure, cardiac arrhythmias, valvular disease, peripheral vascular disorders, pulmonary circulation disorders, chronic pulmonary disease, diabetes, hypertension, renal failure, and sleep apnea).
In addition, to assess if the racial and ethnic disparity of treatment decision (AAD initiation, AAD discontinuation, and CA receipt) was impacted by SES, we built 3 multivariable models for each of the aforementioned outcomes in which education or income were removed (model 1: only education was removed; model 2: only income was removed; model 3: both education and income were removed). Percentage change of the effect size of race and ethnicity was obtained by comparing OR and HR of these trimmed models to those estimated by the primary multivariable logistic and Cox regressions, respectively. Specifically, the percentage change was calculated by using the following formula (effect measure[trimmed model] – effect measure[primary model])/effect measure[primary model] × 100%.18,19
Two-sided values of p <0.05 were considered to be statistically significant. Statistical analyses were conducted with R software (version 4.1.2; R Foundation for Statistical Computing, Vienna, Austria) and STATA (version 17; StataCorp, College Station, TX, USA).
Results
From 2010 to 2019, 143,281 patients had newly diagnosed AF and were included in the AAD initiation analysis. Table 1 describes key characteristics of patients with newly diagnosed atrial fibrillation, stratified by race and ethnicity. The mean age was 69 years and 54.9% were male. Compared to NHW, patients identified as NHB had a higher proportion of females (NHW 44.2% compared to NHB 52.1%); NHB were less likely to have a bachelor’s degree or higher (NHW 17.4% compared to NHB 5.7%) and more likely to be in the income category of less than $50,000 (NHW 33.3% compared to NHB 57.9%). In general, patients identified as NHB had a greater burden of comorbidities than NHW.
 |
Table 1 Characteristics of Patients with Newly Diagnosed AF |
Of the 143,281 patients identified with new onset AF, 30,019 patients (21%) initiated an AAD within 90 days of AF diagnosis (Table 2). The most commonly prescribed AAD was amiodarone (10.6%), followed by flecainide (3.5%), sotalol (3.1%), dronedarone (2.1%), propafenone (1.3%), and dofetilide (0.4%). Overall, 21.0% of patients identified as NHW initiated AAD within 90 days after AF diagnosis, and the initiation rate was 20.6%, 22.0%, 20.0%, and 18.8% for patients identified as NHB, Hispanic, Asian, and Other, respectively (univariate comparison of AAD initiation across race and ethnicity p <0.01). In the fully adjusted model, NHB were 10% less likely to receive an AAD compared to NHW (aOR = 0.90, 95% CI = 0.85–0.94), while there were no significant differences between NHW and Hispanic, Asian, or patients identified as Other (Figure 1). In the subgroup analyses investigating AAD initiation by age, gender, and income, the impact of race and ethnicity had a similar impact on the rate of AAD receipt as in the primary analysis (Supplemental Table 2). When looking at individual AAD, patients identified as NHB and Hispanic were more likely to initiate amiodarone compared to patients identified as NHW, Asian, and Other (Table 2). Similar to the primary analysis, ORs of the sensitivity analyses suggested that NHB, compared to NHW, were less likely to initiate AAD (Supplemental Table 3).
 |
Table 2 Rate of Antiarrhythmic Drug Initiation Stratified by Race and Ethnicity |
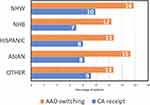
Of the 29,620 patients initiating AAD within 90 days of AF diagnosis, 20.2% of patients had an AF- related hospitalization and 28.6% had a cardiovascular-related hospitalization within two years of AAD initiation. Patients identified as NHB had a significantly higher rates of AF-related and cardiovascular disease-related hospitalization, while patients identified as Asian had lower rates of AF and cardiovascular disease-related hospitalization (Log-rank p <0.01 for comparisons of AF and cardiovascular disease-related hospitalizations across all ethnic and racial groups) (Figure 2). During this time, 15.2% of patients transitioned to a new AAD, and 9.5% of patients underwent CA. Despite the highest rate of AF-related hospitalization, NHB were least likely to transition to a new AAD or receive CA (Figure 3). After adjustment, patients identified as NHB were 17% less likely to receive ablation compared to patients identified as NHW (HR 0.83, 95% CI 0.70–0.97). In sensitivity analysis for CA receipt, HR of NHB did not change substantially compared to primary analysis, although statistical significance was not observed. There was no significant difference in the rate of ablation between patients identified as NHW and Hispanic, Asian, or patients identified as Other (Supplemental Table 4).
Of the 29,620 patients initiating AAD within 90 days after AF diagnosis and included in the discontinuation analysis, 64.8% discontinued AAD within two years (Supplemental Table 5). Patients initiating amiodarone had the highest discontinuation rate (78.4%), followed by dronedarone (75.3%), propafenone (69.2%), flecainide (59.8%), sotalol (51.8%), and dofetilide (45.9%). Patients identified as Asian had the highest discontinuation rate (71.7%), followed by Hispanic (69.1%), patients identified as Other (67.2%), NHW (64.4%), and NHB (61.5%) (p < 0.01). Similar to the overall analysis, patients identified as NHB were least likely to discontinue amiodarone. The Kaplan–Meier curve (Supplemental Figure 2) showed that discontinuation rates significantly differed across race and ethnicity groups (log-rank p <0.01). In the fully adjusted model, patients identified as Hispanic and Asian were significantly more likely to discontinue AAD compared to NHW, while NHB had a similar rate of discontinuation as NHW (Figure 4). In the subgroup analysis investigating the rate of AAD discontinuation stratified by age, gender, and income, race and ethnicity had similar impacts on the rate of AAD discontinuation as in the primary analysis (Supplemental Table 6). In sensitivity analysis for AAD discontinuation, Hispanic patients, compared to NHW patients, were more likely to have AAD discontinuation within 2 years since AAD initiation (Supplemental Table 7).
 |
Figure 4 Adjusted hazard ratios for AAD discontinuation within two years of AAD initiation in patients with newly diagnosed AF. Compared to patients identified as NHW, patients identified as Hispanic and Asian were significantly more likely to discontinue AAD within two years of AAD initiation. There was no difference in the rate of AAD discontinuation between patients identified as NHW and NHB, or between patients identified as NHW and Other. The model adjusted for the same covariates in Figure 1. Abbreviations: AAD, antiarrhythmic drug; NHB, Non-Hispanic Black; NHW, Non-Hispanic White. |
By comparing ORs from the trimmed models to those obtained from the primary model, we found that the proportion of association between race and ethnicity and AAD initiation that could be explained by education or income was minimal (Supplemental Table 8a). Similarly, we did not find evidence to support that the association between race and ethnicity and AAD discontinuation could be explained by education or income (Supplemental Table 8b). However, when comparing HRs from the trimmed models to those estimated by the primary Cox regression model for CA receipt, we found that income explained about 12% of the differential likelihood of CA receipt between NHW and NHB patients; this percentage increased to almost 16% if education was incorporated (Supplemental Table 8c).
Discussion
To our knowledge, this is the first investigation of AF treatment patterns following initiation of antiarrhythmic medications. We found that patients identified as NHB were significantly less likely to initiate AAD following an initial diagnosis of AF. However, once initiated on an AAD, patients identified as NHB were most likely to be hospitalized for AF, and were least likely to transition to a different AAD, receive CA, or discontinue the AAD. The lower rate of CA receipt among NHB patients can be partially explained by lower income and educational background.
Disparity in initial rhythm control of AF has been previously identified. A study based on Medicare data analyzed 517,941 newly diagnosed AF patients between 2010 and 2011; their results suggested a lower rate of CA in Hispanic AF patients compared to White peers (HR[Hispanic vs White]=0.70, 95% CI 0.63–0.79).20 However, the characteristics of their database make the conclusion less generalizable to AF patients of current era or younger age. Another study analyzed 109,221 patients from the Optum database who were diagnosed with incident paroxysmal AF between 2015 and 2019.4 After multivariable adjustment, they found that Black patients were less likely to use rhythm control strategy than White patients. Our study expanded their findings by exploring patients of different age groups, including all types of AF, and depicting AF-related health services use from a longitudinal perspective, making a stronger generalizability of the conclusion to AF patients.
In the present study, we also found a very high rate of AAD discontinuation within two years of initiation, with 64% of patients initiated on an AAD stopping the medication. While amiodarone was the most frequently prescribed AAD accounting for more than 50% of the prescriptions for AAD, it was also the most frequently discontinued. Due to the retrospective nature of this study, we cannot determine the reason for AAD continuation or discontinuation, but possible causes include successful use of ablation to decrease the burden of atrial fibrillation (though the rate of AAD discontinuation is significantly greater than the rate of CA), intolerance of or side effects from AAD, or changes in AF treatment strategy.
After initiated on an AAD and rhythm control, we identified continued differences in treatment associated with race and ethnicity. Despite the highest rates of AF-related hospitalization, patients identified as NHB had lowest rates of CA, or AAD change.
The cause of the differential treatment patterns identified in this study is unclear. One possible cause is a lower rate of referral to Cardiology or Electrophysiology for consideration of CA (particularly after AF-related hospitalization following AAD initiation) due to differential access to subspecialty care or provider education regarding the benefits of CA.4,21,22 However, in a single integrated heart care system, NHB and NHW patients with newly diagnosed AF had similar rates of referral to General Cardiology and Electrophysiology Clinics. Differences in who ultimately received AF ablation were observed only in referral from Electrophysiology Clinic for ablation.23
Another possible cause of the treatment patterns observed in the present study is failure of the medical system to earn patient trust and differences in response to shared decision-making regarding whether to proceed with AAD or catheter ablation. After counselling regarding the benefits of primary prevention Implantable Cardioverter Defibrillators (ICDs), patients identified as Black and Hispanic were less likely to proceed with ICD implantation.24 A similar response to counselling could impact AF management trends. Systematic and structural racism could similarly contribute to these disparities in AF management.
This disparity in treatment patterns is particularly important to identify, understand, and address due to an association of AAD use with adverse cardiovascular outcomes in patients from ethnic and racial minorities. In a subgroup analysis of the CABANA trial, patients identified as nonminority in North America had similar rates of the composite endpoint of death, disabling stroke, serious bleeding, or cardiac arrest regardless of whether they were randomized to rhythm control with ablation or AAD. However, patients identified as a racial or ethnic minority had a significantly higher rate of the composite endpoint when treated with an AAD compared with ablation.25 Benefits of CA in racial and ethnic minorities are also observed in prior research based on real-world data. For example, a prior study leveraging claims data found that Black and Hispanic AF patients receiving CA, compared to patients receiving AAD for treatment, had an approximately 50% lower risk of heart failure.26 Due to the covariates available in the Optum SES dataset, we could not investigate whether there were differences in death associated with race and ethnicity and AAD use. However, patients identified as NHB were least likely to change their AAD or undergo CA within two years of initial AF diagnosis, despite having the highest rate of AF-related hospitalization. While further studies are needed to confirm the results of the CABANA sub-study, our results indicate that NHB patients have greater AAD exposure (particularly to amiodarone) and lower rates of CA despite higher rates of treatment failure increasing the risk of adverse events associated with prolonged AAD use.
Large studies looking systematically at the US health care system referral patterns and patterns for rhythm management (including for AAD use and ablation), as well as further investigation into the etiology of differences in AAD use, are required to better identify points of intervention to reduce the disparity and improve outcomes in patients with AF. Given the anticipated growth of new AF diagnoses over the next several decades,27 unrecognized and unaddressed disparities in AF treatment will result in significantly more morbidity and mortality in historically disadvantaged populations. Globally, each country has its own racial and ethnic structure and health system, thus the generalizability of our conclusion to other countries should be further assessed in the future. However, our study suggests that health policy makers of different countries should be aware that treatment patterns of AF patients may be differential across racial and ethnic groups and consider this potential disparity when allocating healthcare resource.
Study Limitations
The present study investigates outcomes following use of AAD in patients with commercial insurance over 13 years facilitating inclusion of a large number of patients with newly diagnosed AF. Despite the strength of this large dataset allowing robust adjustments, there are some limitations. While use of an administrative dataset over such a long time allowed for a large patient population to be studied, due to use of ICD-9 and ICD-10 codes the dataset could not provide more granular information on type of atrial fibrillation present at diagnosis. Similarly, unmeasurable confounders such as COPD severity, New York Heart Association functional class, left ventricular ejection fraction, or fragility could not be assessed and may impact the results. Adjustments of socioeconomic status including education level and household income was performed in this analysis, but more granular assessments of socioeconomic status through incorporation of community factors was not possible.
Treatment of AF is often guided by AF-related symptoms.28,29 Previous studies have identified that patients identifying as Black are more likely to report more severe AF-related symptoms compared to patients identifying as White.30 While we were unable to account for symptoms in the present analysis, we would expect more attempts at rhythm control in patients identified as NHB due to symptom severity, which is the opposite of what we identified in the present analysis.
Additionally, the decision on whether to proceed or continue with rhythm control via AAD or catheter ablation is determined with shared decision-making. The result of this discussion is influenced not only by the clinical judgement to offer various treatments but also how the information is presented and received. Previous studies have identified racial and socioeconomic differences in how recommendations for cardiovascular procedures such as ICD implantation are delivered and received,24,31 which may similarly influence the disparities seen in the present study. This difference in delivery or receipt of counselling could not be accounted for with the dataset utilized. The study also only included patients initiated on an AAD within 90 days of their initial AF diagnosis, so any patients initiated on an AAD beyond 90 days of AF diagnosis were not included in the present analysis. The Optum dataset only includes patients with commercial insurance. These results may not apply to patients with only Medicare or Medicaid, or those without insurance. The present analysis on race and ethnicity is limited to the broad categorizations of NHW, NHB, Asian and Hispanic as identified in the Optum dataset. Due to limitations in the data, a more granular analysis on the impact of patient race or ethnicity on treatment decisions was not possible.
Conclusions
Patients identified as NHB were least likely to initiate an antiarrhythmic drug within 90 days of initial AF diagnosis. Once initiated on an AAD, patients identified as NHB were most likely to have an AF-related hospitalization but least likely to receive CA or transition to a different AAD. Additional studies are required to further investigate the etiology of the disparity in AAD and CA use and outcomes in order to design interventions to provide more equitable care for patients with atrial fibrillation.
Acknowledgment
The abstract of this paper was presented at the 2023 annual meeting of Heart Rhythm Society as a conference talk with interim findings. The abstract associated with this study was published in Abstract in Heart Rhythm: https://doi.org/10.1016/j.hrthm.2023.03.426
Funding
This study was funded by Johnson & Johnson.
Disclosure
Leeor Herzog, Rahul Khanna, and Dongyu Zhang are employees of Johnson and Johnson. Ryan Kipp reports non-financial support from BioSense Webster, outside the submitted work.
References
1. Marrouche NF, Brachmann J, Andresen D, et al. Catheter ablation for atrial fibrillation with heart failure. N Engl J Med. 2018;378(5):417–427. doi:10.1056/NEJMoa1707855
2. Kirchhof P, Camm AJ, Goette A, et al. Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med. 2020;383(14):1305–1316. doi:10.1056/NEJMoa2019422
3. Kushnir A, Barbhaiya CR, Aizer A, et al. Temporal trends in atrial fibrillation ablation procedures at an academic medical center: 2011–2021. J Cardiovasc Electrophysiol. 2023;34:800–807. doi:10.1111/jce.15839
4. Eberly LA, Garg L, Yang L, et al. Racial/ethnic and socioeconomic disparities in management of incident paroxysmal atrial fibrillation. JAMA Network Open. 2021;4(2):e210247. doi:10.1001/jamanetworkopen.2021.0247
5. Amponsah MK, Benjamin EJ, Magnani JW. Atrial fibrillation and race - A contemporary review. Curr Cardiovasc Risk Rep. 2013;7(5):336–345. doi:10.1007/s12170-013-0327-8
6. Freeman L, Kee A, Tian M, et al. Retrospective claims analysis of treatment patterns, relapse, utilization, and cost among patients with multiple sclerosis initiating second-line disease-modifying therapy. Drugs Real World Outcomes. 2021;8(4):497–508. doi:10.1007/s40801-021-00251-w
7. Field ME, Goldstein L, Corriveau K, et al. Same-day discharge after catheter ablation in patients with atrial fibrillation in a large nationwide administrative claims database. J Cardiovasc Electrophysiol. 2021;32(9):2432–2440. doi:10.1111/jce.15193
8. O’Byrne ML, DeCost G, Katcoff H, et al. Resource utilization in the first 2 years following operative correction for tetralogy of Fallot: study using data from the optum’s de-identified clinformatics data mart insurance claims database. J Am Heart Assoc. 2020;9(15):e016581. doi:10.1161/JAHA.120.016581
9. D’Angelo RN, Rahman M, Khanna R, et al. Limited duration of antiarrhythmic drug use for newly diagnosed atrial fibrillation in a nationwide population under age 65. J Cardiovasc Electrophysiol. 2021;32(6):1529–1537. doi:10.1111/jce.15012
10. LaPointe NM A, Dai D, Thomas L, et al. Antiarrhythmic drug use in patients <65 years with atrial fibrillation and without structural heart disease. Am J Cardiol. 2015;115(3):316–322. doi:10.1016/j.amjcard.2014.11.005
11. Biancari F, Teppo K, Jaakkola J, et al. Income and outcomes of patients with incident atrial fibrillation. J Epidemiol Community Health. 2022;76(8):736–742. doi:10.1136/jech-2022-219190
12. Essien UR, Kornej J, Johnson AE, et al. Social determinants of atrial fibrillation. Nat Rev Cardiol. 2021;18(11):763–773. doi:10.1038/s41569-021-00561-0
13. LaRosa AR, Claxton J, O’Neal WT, et al. Association of household income and adverse outcomes in patients with atrial fibrillation. Heart. 2020;106(21):1679–1685. doi:10.1136/heartjnl-2019-316065
14. Xue X, Xie X, Gunter M, et al. Testing the proportional hazards assumption in case-cohort analysis. BMC Med Res Methodol. 2013;13:88. doi:10.1186/1471-2288-13-88
15. U.S. Census Bureau. QuickFacts. Available from: https://www.census.gov/quickfacts/fact/table/US/PST045222.
16. National Center for Education Statistics. Median household income, by state. Available from: https://nces.ed.gov/programs/digest/d11/tables/dt11_025.asp.
17. U.S. Census Bureau. Income and poverty in the United States: 2015. Available from: https://www.census.gov/library/publications/2016/demo/p60-256.html.
18. Yuan Y, Taneja M, Connor AE. The effects of social and behavioral determinants of health on the relationship between race and health status in U.S. Breast Cancer survivors. J Womens Health. 2019;28(12):1632–1639. doi:10.1089/jwh.2018.7360
19. Karlson KB, Popham F, Holm A. Marginal and conditional confounding using logits. Sociol Methods Res. 2023;52(4):1765–1784. doi:10.1177/0049124121995548
20. Bhave PD, Lu X, Girotra S, et al. Race- and sex-related differences in care for patients newly diagnosed with atrial fibrillation. Heart Rhythm. 2015;12(7):1406–1412. doi:10.1016/j.hrthm.2015.03.031
21. Cook NL, Ayanian JZ, Orav EJ, et al. Differences in specialist consultations for cardiovascular disease by race, ethnicity, gender, insurance status, and site of primary care. Circulation. 2009;119(18):2463–2470. doi:10.1161/CIRCULATIONAHA.108.825133
22. Eberly LA, Richterman A, Beckett AG, et al. Identification of racial inequities in access to specialized inpatient heart failure care at an academic medical center. Circ Heart Fail. 2019;12(11):e006214. doi:10.1161/CIRCHEARTFAILURE.119.006214
23. Duke JM, Muhammad LN, Song J, et al. Racial disparity in referral for catheter ablation for atrial fibrillation at a single integrated health system. J Am Heart Assoc. 2022;11(18):e025831. doi:10.1161/JAHA.122.025831
24. Hess PL, Hernandez AF, Bhatt DL, et al. Sex and race/ethnicity differences in implantable cardioverter-defibrillator counseling and use among patients hospitalized with heart failure: findings from the get with the guidelines-heart failure program. Circulation. 2016;134(7):517–526. doi:10.1161/CIRCULATIONAHA.115.021048
25. Thomas KL, Al-Khalidi HR, Silverstein AP, et al. Ablation versus drug therapy for atrial fibrillation in racial and ethnic minorities. J Am Coll Cardiol. 2021;78(2):126–138. doi:10.1016/j.jacc.2021.04.092
26. Gruber M, Iglesias M, Khanna R, et al. Heart failure risk in patients with atrial fibrillation treated with catheter ablation vs antiarrhythmic drugs. Heart Rhythm O2. 2023;4(11):681–691. doi:10.1016/j.hroo.2023.09.009
27. Lippi G, Sanchis-Gomar F, Cervellin G. Global epidemiology of atrial fibrillation: an increasing epidemic and public health challenge. Int J Stroke. 2021;16(2):217–221. doi:10.1177/1747493019897870
28. Hindricks G, Potpara T, Dagres N, et al. ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European society of cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498. doi:10.1093/eurheartj/ehaa612
29. January CT, Wann LS, Alpert JS, et al. AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):e199–267. doi:10.1161/CIR.0000000000000041
30. Golwala H, Jackson LR 2nd, Simon DN, et al. Racial/ethnic differences in atrial fibrillation symptoms, treatment patterns, and outcomes: insights from outcomes registry for better informed treatment for atrial fibrillation registry. Am Heart J. 2016;174:29–36. doi:10.1016/j.ahj.2015.10.028
31. Whittle J, Conigliaro J, Good CB, et al. Do patient preferences contribute to racial differences in cardiovascular procedure use? J Gen Intern Med. 1997;12(5):267–273. doi:10.1007/s11606-006-5062-0
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.