Back to Journals » Patient Preference and Adherence » Volume 18
Quality Control Circle Practices to Improve Mask-Wearing Compliance by Patients Diagnosed with Tuberculosis During External Examinations
Authors Liu W, Guo J, Jiang Q, Zhou G, Dong Y, Xu B, Liu Z, Zhang Z, Liu J
Received 19 October 2023
Accepted for publication 9 January 2024
Published 21 January 2024 Volume 2024:18 Pages 227—237
DOI https://doi.org/10.2147/PPA.S445632
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Wangmei Liu,* Jing Guo,* Qiaomin Jiang, Guangnao Zhou, Yanyu Dong, Biqing Xu, Zhongda Liu, Zunjing Zhang, Jianjun Liu
Department of Tuberculosis, Lishui Hospital of Traditional Chinese Medicine, Lishui, Zhejiang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jianjun Liu; Zunjing Zhang, Department of Tuberculosis, Lishui Hospital of Traditional Chinese Medicine, No. 800 Zhongshan Street, Liandu District, Lishui, 323000, People’s Republic of China, Tel +86 13757835027 ; +86 13884387661, Email [email protected]; [email protected]
Objective: The purpose of this study is to examine the effect of quality control circle (QCC) activities on increasing the mask-wearing compliance of hospitalized patients diagnosed with tuberculosis (TB) during external examinations.
Methods: To assess the mask-wearing compliance of patients diagnosed with TB admitted to a ward in our hospital in 2019, who visited other departments, we conducted activities in accordance with the ten steps of the QCC. We outlined the causes of non-compliance and developed and implemented improvement plans. We compared the results obtained before and after the implementation of the QCC to assess the enhancement in patient compliance concerning wearing masks during external examinations, particularly among individuals diagnosed with pulmonary tuberculosis.
Results: The compliance rate for mask-wearing during external examinations rose from an initial 32.61% (45/138) prior to the intervention to 83.71% (149/178) following the intervention. The difference between the two groups was statistically significant (χ2 = 85.635, P < 0.001). The following countermeasures and implementation measures were formulated: (1) Increasing public health education and awareness; (2) Strengthening the training of nursing staff to enhance their knowledge; (3) Providing free surgical masks; (4) Establishing an effective monitoring system with the department of auxiliary examinations.
Conclusion: QCC interventions were significantly effective in enhancing adherence to mask-wearing protocols during external examinations of hospitalized patients with tuberculosis. Such improvements contribute substantially to the mitigation of tuberculosis transmission within clinical and healthcare environments.
Keywords: compliance, quality control circle, surgical mask, tuberculosis
Introduction
In the Global Tuberculosis Report 2023 released by the World Health Organization, on November 7, 2023, it was disclosed that globally, a total of 10.6 million new tuberculosis (TB) cases emerged in 2022.1 The incidence rate stood at 133 cases per 100,000 patients. It is noteworthy that two-thirds of these cases emanated predominantly from specific countries: India (27%), Indonesia (10%), China (7.1%), the Philippines (7.0%), Pakistan (5.7%), Nigeria (4.5%), Bangladesh (3.6%), and Congo (3.0%). TB, a persistent respiratory contagion, is caused by the bacterium Mycobacterium tuberculosis. This ailment has been a recurrent menace to human health for a millennium. As per the WHO’s global mortality data from 2019, TB ranks as the 13th principal global cause of mortality.2 Predating the 2019 outbreak of the COVID-19 pandemic, TB was recognized as the foremost cause of mortality attributed to a singular infectious agent, exceeding deaths associated with HIV/AIDS.3 The disease has exerted a profound adverse impact on the collective health status of global populations.
Despite the progression and breakthroughs in modern medicine, the persistent prevalence of TB underscores the intricate nature of this ailment. One of the Sustainable Development Goals (SDGs) of the United Nation targets the eradication of TB by the year 2030. In alignment with this, the end TB strategy of the WHO has delineated ambitious benchmarks. It aspires to slash the incidence rate by 80% by 2030, taking the data from 2015 as a reference point. Furthermore, the strategy endeavors to curtail the sheer incidence rate to a figure below 20 cases per 100,000 patients. While China has exhibited commendable strides in its pursuit to eradicate TB, its status remains cataloged as a nation with “medium” TB incidence. With a prevailing incidence rate of “60 per 100,000”, there is an imperative need to reduce it down to “20 per 100,000”. The magnitude of this challenge cannot be understated.
The primary cause of TB infection is aerosolized bacteria from patients diagnosed with TB. Air and droplets are the principal transmission methods. When patients cough, sneeze, or speak loudly, they expel TB droplets of 1–5 μm in diameter. Healthy individuals can inhale these droplets directly into their alveoli, where they are phagocytosed by macrophages and cause infection. By effectively obstructing the airborne transmission pathways of M. tuberculosis,4 the likelihood of TB transmission is drastically reduced. This may have a protective effect on the local population and reduce hospital infection rates. Relevant research findings indicate that the lack of self-awareness among patients with TB contributes to the formation of unhealthy daily practices.4 This hinders the management of patients illness and leads to the extensive spreading of M. tuberculosis.4 Under the assumption that the state of patients diagnosed with TB permits it, surgical masks should be worn at all times to achieve isolation. Currently, mask-wearing protocols for patients with TB in domestic hospitals are not standardized. The proportion of hospitalized patients with TB who wear surgical masks is low, and compliance is moderate.5 Thus, augmenting the adherence of patients with TB to mask-wearing becomes paramount.
The Quality Control Circle (QCC) can be characterized as a collaborative assembly of individuals operating within the same professional environment and tasked with analogous roles. Often referred to as the quality management team, the constituents of QCC engage in collective endeavors, harnessing the division of labor, ideation, and problem-solving methodologies to bolster the caliber and productivity of their professional tasks.6 The modus operandi of QCC entails a systematic sequence of intertwined processes all aimed at perpetuating advancements in quality. This methodology has garnered substantial endorsement in the field of hospital management. In this context, the TB department of our hospital embarked on the initiation of QCC activities in August 2019. The focal point of this present study is to gauge the efficacy of such initiatives in magnifying adherence to mask-wearing protocols during external examinations of hospitalized patients afflicted with pulmonary TB.
Data and Methods
General Data
This study included 138 patients with TB admitted to the TB Department at Lishui Hospital of Traditional Chinese Medicine who underwent external examination in September 2019 as the pre-implementation cohort for the QCC initiatives. In contrast, a subsequent group of 178 patients with TB who were admitted and underwent external examination in October 2019 were identified as the post-implementation cohort of the QCC. The data collection endeavored to capture the frequency of mask-wearing by these patients at multiple stages: as they departed from their respective wards, during their examination sessions in auxiliary departments (EKG room, B ultrasound room, and radiology), and as they made their return to their wards subsequent to the examinations. Moreover, we collected Supplementary Data concerning the proper wearing of these masks by the patients to serve as reference data.
Research Method
Understanding the Current Situation
A survey for “Tuberculosis Patients’ Mask-Wearing During External Examinations” was designed, including patient name, hospitalization number, date, external examination items, and sections on “whether wearing a mask” and “whether wearing a mask correctly”. These sections were completed by nursing staff in the ward before the external examination, assisted by medical staff during the examination, and filled out by nursing staff in the ward after the external examination. Trained and qualified investigators conducted surveys on tuberculosis patients undergoing external examinations, and the completed forms were collected after being filled out. The collected data include information on whether patients wore masks during examinations. The survey consisted essentially of three parts of data included: (1) determining if the patients wore masks; (2) if they did, assessing if they wore them correctly and asking those who wore masks poorly for their reasons; and (3) if they did not wear masks, requesting their reasons.
Goal Setting
This study scored four candidate themes across four dimensions: policy, importance, urgency, and circle capability, with a score of 1–5 for each dimension. The scores for all alternative themes were then summed, and the one with the highest score was selected as the activity theme. Among the four candidate themes, “Enhancing Compliance of Tuberculosis Patients with Wearing Masks during External Examinations” scored the highest, and thus, it was chosen as the activity theme. The evaluation scores for this theme were as follows: policy, 5.0 points; importance, 5.0 points; urgency, 4.81 points; circle capability, 4.10 points, with a total score of 19.08 points. The circle capacity on the theme scoring sheet was assessed to be 82% based on the scores of the circle members. Prior to the implementation of the QCC, it was determined that 32.61% of patients with TB wore masks when undergoing external examinations. This rate was considered as the current status value. According to the “Pareto chart 80/20” rule, the improvement focus was 83.87%. To determine the target value for improvement, we referred to the formula: target value = current status value + (1 - current status value) × improvement focus × circle capacity = 32.61% + (1–32.61%) × 83.87% × 82.00% = 78.96%. Therefore, the goal was to increase the mask-wearing compliance rate of patients with TB during external examinations from 32.61% to 78.96% by December 2019, which represents a 142.13% increase.
Analysis of the Essential Factors
Members of the circle used the brainstorming method to conduct a typical essential element analysis, concentrating on four primary variables: people, methods, things, and other factors (such as economic, cultural differences, and geographical environment).
Countermeasure Formulation and Implementation
- All circle members analyzed each initiative based on its viability, cost-effectiveness, the capacity of the circle, and other pertinent considerations to determine the most effective countermeasures. The grading scale was as follows: outstanding (5 points), general (3 points), and inadequate (1 point).
Confirming the Effect
- The effect was confirmed: Target achievement rate = (After improvement - Before improvement) / (Target value - Before improvement) × 100%; Progress rate = (After improvement - Before improvement) / Before improvement × 100%.
- Confirmation of intangible results: Before and after the implementation of the QCC, circle members used the self-assessment approach to evaluate eight items: responsibility, cohesion, motivation, cooperation, communication and coordination skills, quality control procedures, professional knowledge, and self-assurance. Each evaluation item was rated using three grades: 5, 3, and 1 point.
Statistical Analysis
IBM SPSS Statistics 23.0 was used to statistically evaluate the data. Before and after the adoption of the QCC, the compliance rate of patients with TB undergoing external examination was compared. The comparison was conducted using the χ2 test for categorical variables. A significance level of P < 0.05 was used to determine if the difference was statistically significant.
Results
Mask-Wearing Compliance of Patients with TB Undergoing External Examination Before the Implementation of the QCC
After the survey was conducted in September 2019, a total of 138 patients with TB underwent external examinations. Among these, 45 (32.61%) patients wore masks appropriately, while 10 (7.25%) patients wore masks incorrectly. There are four main manifestations of incorrect mask wearing, as shown in Figure 1. The poor mask-wearing compliance of patients with TB during examinations (including those who did not wear masks or wore masks incorrectly) can be summarized as follows: lack of knowledge about TB, inadequate education from nurses, limited access to masks, absence of supervision, fear of discrimination, and discomfort while wearing masks. We calculated the average value of each cause and the proportion of total causes and created a checklist before implementing the QCC and a Pareto chart (Figure 1) prior to implementing improvements. According to the “Pareto chart 80/20” rule, the identified priorities for improvement include: lack of information about TB, inadequate nursing education, limited access to masks, and lack of supervision. These initiatives account for a cumulative percentage of 83.87% (The improvement focus was 83.87%, Table 1).
 |
Table 1 Checklist of Reasons for Low Compliance Among Patients Diagnosed with TB Undergoing External Evaluation (Before Implementation) |
 |
Figure 1 Pareto chart before the improvement. |
Mask-Wearing Compliance of Patients with TB Undergoing External Examination After the Implementation of the QCC
After implementation of the QCC in December 2019, 178 patients with TB underwent external examinations. Following the deployment of the improvement measures, the compliance rate jumped from 32.61% to 83.71%, with 149 of these patients wearing masks appropriately. Additionally, 8 patients wore masks improperly, which dropped the wrong usage rate from 7.24% to 4.58% prior to the implementation. Figure 2 and Table 2 lists the reasons for poor compliance among patients with TB undergoing external examination, including those who did not wear masks or wore them inappropriately.
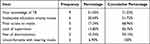 |
Table 2 Checklist of Reasons for Poor Mask Compliance Among Patients Diagnosed with TB Undergoing External Examination (After Implementation) |
 |
Figure 2 Pareto chart after the improvement. |
Comparison of Mask-Wearing Compliance of Patients with TB Undergoing External Examination Before and After the Implementation of the QCC
The difference between the two was statistically significant (χ2 = 85.635, P < 0.001, refer to Table 3). In addition, the rate of patients with TB who used masks when walking outside (83.71%) exceeded the target value (78.96%), attaining a rate of 110.25% and a progression rate of 156.70%. After the implementation of the QCC, the error rate of patients with TB who wore masks when undergoing external examinations decreased to 5.10% from 18.18% before the implementation. This difference was determined to be statistically significant (χ2 = 8.978, P = 0.003, refer to Table 3).
 |
Table 3 Compliance with Mask Use Among Patients Diagnosed with TB undergoing External Examination Before and After Implementation |
Analysis and Strategies for Poor Compliance with Mask-Wearing Among Tuberculosis Patients
This analysis was parsed using a fishbone diagram (Figure 3), enabling the identification and examination of 15 medium essential components and 16 small essential factors. Factors outside the scope of competence, such as economic factors, cultural differences, and geographical environment, were eliminated. The underlying causes contributing to poor mask-wearing compliance among patients with TB during examinations in September 2019 were identified and analyzed. Using the 80/20 rule, the leading influences on this issue were identified and plotted on a Pareto chart: (1) Medical personnel lack of professional knowledge; (2) lack of supervision materials; (3) patients have limited access to masks; and (4) patients lack disease knowledge.
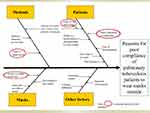 |
Figure 3 Fishbone diagram for assessing the important factors of poor compliance of wearing masks for patients diagnosed with TB undergoing external examination. |
Ten members of the circle contributed to the scoring, for a total of 150 points. In accordance with the 80/20 rule, countermeasures were implemented if the overall score was 120 points or higher. However, the ability and energy constraints of the circle were also considered. The selected countermeasures were determined by the two items with the greatest marks in each category. Eventually, the following countermeasures and implementation measures were formulated:
- Increase public health education and awareness. It is essential to undertake thorough and systematic health education suited to the cultural backgrounds and educational levels of patients using various modes of health education, including verbal communication, written materials, visual aids, and on-site demonstrations. This can help improve the efficacy of instructional endeavors. The primary focus of the education is on the causes, progression, treatment, and prevention of TB. It specifically emphasizes the significance of wearing masks to prevent the spread of TB. The objective is to ensure that patients have a scientific understanding of the disease and to enhance their adherence to treatment.
- Strengthen the training of nursing staff to enhance their knowledge, raise their awareness, and expand the scope and methods of education. The department should routinely host monthly training sessions for nurses to improve their awareness of TB (Please refer to Supplementary Material - Key Points in Tuberculosis Prevention and Control”). The head nurse should conduct weekly spot checks to ensure the assigned nurses are present and doing their duties, and a monthly theoretical exam should be conducted.
- Free surgical masks should be provided, and the locations for mask placement be prominently displayed. The primary shift should deliver surgical masks to all inpatients daily. When patients undergo external examinations, nurses should inspect mask-wearing practices and instruct patients.
- Establish an effective monitoring system with the department of auxiliary examinations. Formulating the Questionnaire on Wearing Masks for Patients with TB Undergoing External Examination is crucial. The auxiliary examination departments should collaborate on the completion of the questionnaire and provide timely feedback on any issues. Additionally, departments should take prompt measures to address any existing issues.
Comparison of the Comprehensive Abilities of Healthcare Personnel Before and After the Implementation of the QCC
Circle members saw improvements with respect to their sense of responsibility, cohesion, motivation, cooperation, communication coordination ability, quality control techniques, professional knowledge, and self-confidence after implementing the “Improving mask-wearing compliance of patients with TB undergoing external examinations” QCC project as shown in Figure 4.
 |
Figure 4 Before and after the implementation of QCC, a radar plot comparing the comprehensive skills of health care personnel. |
Discussion
The epidemic curve can be slowed by mask use in conjunction with avoiding close personal contact. One non-pharmaceutical intervention (NPI) that makes sense for combating TB is the use of masks. Mitigating the public health and economic costs of TB epidemics requires highly effective ways to stop the spread of the disease. Several steps should be taken to reduce the spread of tuberculosis and keep hospitals from being overwhelmed with patients until more effective treatments, vaccines, and healthcare resources become available. One of the NPI measures that works well for a low price and causes little to no social upheaval is masking.7 More and more nations and areas are advocating for mask legislation or recommending that their citizens do so. Previous research has shown that TB infections have decreased in mainland China since the COVID-19 outbreak. It is possible that the lockdown, when hospitals were closed, contributed to this decline.8 Similarly, Lai et al discovered that the prevalence of tuberculosis infections dropped during the COVID-19 outbreak in Taiwan because of the widespread use of protective gear, especially masks.9
TB is a chronic infectious disease transmitted by respiratory droplets, and since patients having TB are a common source of infection in clinical practice, appropriate protective measures must be taken to minimize the chances of contact between patients and their relatives and friends in the vicinity. Currently, standardized surgical masks, which are made of three layers of material, are used as a tool to isolate M. tuberculosis from the surrounding population. The risk of exhaling droplets through the mouth and so increasing the concentration of suspended M. tuberculosis in the environment is much reduced when a surgical mask is used. As a result, the spread of M. tuberculosis is impeded.
The “13th Five-Year Plan” for National Tuberculosis Prevention and Control10 was released by the State Council in February 2017. The plan emphasizes the need for
conditionally qualified areas to carry out pilot hospitalization of infectious patients diagnosed with TB and gradually transition to hospitalization of patients during the infectious period.
It also highlights the need of implementing TB infection control measures to prevent cross-infection in hospitals. Our hospital took the initiative in implementing a pilot program for hospitalizing infectious patients with TB in order to fully implement the “13th Five-Year Plan” for National Tuberculosis Prevention and Control.10 During the implementation period, we discovered the risk of “nosocomial cross-infection” for infectious patients with TB who left the hospital/ward for external examinations while still being hospitalized. As a result, the hospital implemented mask requirements for all patients with TB who left their wards for medical care. The majority of patients with TB, however, were found to not adhere to mask usage during implementation. A QCC project titled “Improving mask-wearing compliance of patients with TB during external examinations” was therefore developed and implemented at the hospital.
In this study, it was determined that the primary factors contributing to the poor mask-wearing compliance of patients with TB during external examinations were: (1) poor knowledge about TB by the patients, leading to a failure to understand the importance of wearing masks; (2) the insufficient expertise and training of healthcare professionals, as well as the limited availability of educational materials; (3) inadequate access to masks; and (4) the absence of effective regulatory measures.
Patients with TB often fail to adhere to mask-wearing guidelines as they lack understanding about the disease and fail to understand its significance. Poor knowledge about TB among patients leads to their dread of the disease and prevents them from realizing how important it is for them to wear masks. Due to this ignorance, patients fail to realize the importance of mask use when exposed to TB. Therefore, they are less likely to take necessary safety precautions. In this study, patients diagnosed with TB and their loved ones knew very little about the disease and how to treat it. Due to their inability to appreciate the necessity of mask use, compliance was low. People with lower levels of education were most likely to have incomplete or incorrect understandings of TB and the medical advice given by their doctors. Traditionally, it has been thought that breathing in dust contaminated with tuberculous bacteria is the principal route by which the disease is spread. In any case, all it takes is for a person with a compromised immune system to breath just one or two M. tuberculosis bacteria into the alveoli to get infected. As a result, it is critical that patients with TB use masks. Therefore, it is the responsibility of healthcare providers to inform patients and their families about the prevention and treatment of TB, emphasizing the necessity of mask use. By increasing the number of patients with TB who consistently wear their masks, it is possible to interrupt the chain of transmission, safeguard the vulnerable, and lower the prevalence of TB.
Due to the lack of knowledge among the public about tuberculosis, health education campaigns are desperately needed. Health education on TB prevention and treatment must be implemented on a massive scale, and the scientific awareness of the disease among patients must be improved. Comprehensive and systematic health education that is tailored to the cultural context of each patient is essential for providing effective treatment. This will enhance the effective of health education and lead to more positive outcomes. Most of the forms of health education are divided into three major types: Verbal information sharing, written and pictorial materials, and audio-visual materials. The content of health education primarily includes basic knowledge of TB, knowledge of isolation, medication guidance, pre-hospital education, psychological education, dietary and rest advice, among others. Patient compliance can be improved if they have a scientific grasp of their disease, treatment, and regression, thus nurses should take the time to calmly explain the causes, course, treatment, and prevention of TB, focusing notably on the necessity of wearing masks. Patients and their loved ones should be educated on the significance of mask use so that they can understand that masks are not just for the protection of the doctors but for their own safety as well.
Lack of professional knowledge regarding tuberculosis among medical staff, inadequate training, single content and form of education, inadequate explanation, and poor service attitude of medical staff also affect the adherence to wearing masks among patients to varying degrees, as determined by the study. It is imperative to improve the nurse-patient communication, monitoring, and subsequent care. A healthy nurse-patient connection fosters mutual understanding, coordination, and the co-creation of a pleasant atmosphere of treatment and recuperation, hence facilitating the recovery of patients. Effective nurse-patient communication can enhance patient adherence, patient satisfaction, and care quality. Regular monitoring and follow-up are essential components of both the therapy process and the conclusion of treatment. Health prescriptions should be issued for each outpatient taking medication or discharged patient, along with a detailed explanation of the contents and methods of monitoring and follow-up, and the outpatient or discharged patient should be transferred to a TB prevention and treatment institution or a designated health care institution so as to implement “centralized management”. It is imperative to establish a good doctor-patient relationship, enhance patient trust, deepen their education on mask compliance, cultivate and enhance the confidence in treatment and positive emotions among patients, and improve their compliance with wearing masks.
Due to different cultural and socio-economic backgrounds, it is important for nurses and health care professionals to be able to effectively communicate the importance of mask wearing to all patients. Health care personnel fail to provide tailored health education based on the varying cultural levels of patients, and the teaching is insufficient. There is no absolute positive correlation between cultural level and adherence, but there is a certain correlation; a tiny proportion of patients cannot adhere to the instructions of the doctor, which is primarily due to other interfering variables, such as psychological impact. Most patients fear that wearing a mask will violate their privacy and expose them to public observation. This fear of being judged hinders patients with TB from wearing masks voluntarily. In addition, most patients with TB experience varying degrees of psychological hurdles due to the long duration and poor recovery from the disease. Many patients with TB view the disease as disgusting and horrifying, causing them to conceal their condition from others. They are also concerned about the possibility of social isolation and rejection by their family and friends. Consequently, these psychological barriers contribute to feelings of apprehension, nervousness, anxiety, and low self-esteem. These negative emotions ultimately lead to a loss of motivation to effectively manage the condition and a decline in treatment adherence.
It is important to provide psychological and social assistance for patients diagnosed with TB. Today, society views tuberculosis as a disease that endangers public health; hence, people may reject and discriminate against patients diagnosed with TB, which exacerbates their inferiority complex and guilt. As a result, patients may be unwilling to wear masks willingly, resulting in a decline in adherence to preventative treatments. The nursing and caregiving personnel should actively encourage patients with TB to wear masks and provide them with outlets to communicate their discontent. Through dissemination of information, patients can realize that TB is not as dangerous as they believe. Patients can achieve a significant level of recovery if they actively participate in treatment and adhere to acceptable chemotherapy and other therapies. Considering the diverse psychological states inherent to patients, it is imperative to tailor publicity, health education, and emotional support accordingly. First, it is essential to equip patients with an exhaustive understanding of TB through disseminating foundational knowledge about the ailment. Such educational endeavors are purposed to mitigate feelings of apprehension, anxiety, perceived inferiority, and trepidation, consequently bolstering their confidence in surmounting the disease. It is vital to underscore that contemporary therapeutic modalities possess a pronounced efficacy in eradicating TB, thus augmenting the trust of patients in medical interventions. Healthcare professionals, especially nurses, are encouraged to offer amplified emotional and spiritual support to enhance the psychological well-being of patients. Such initiatives not only promote disease remission but also elevate the overall quality of life. The demeanor of nursing professionals, characterized by a composed demeanor, affable disposition, and empathetic communication, is essential. This approach facilitates a nurturing environment wherein patients feel emotionally bolstered, unburdened mentally, and receptive to treatment, all the while adhering to necessary precautions like wearing masks comfortably.
Prior to the 2019 COVID-19 pandemic, the primary method for patients with TB to obtain masks was to purchase them from hospitals and pharmacies at an expensive price, resulting in “limited access to masks”. During the outbreak, masks have become a necessity and are available for purchase in supermarkets, pharmacies, and on the internet.
Patients frequently disregard the necessity of wearing masks or refuse to do so due to the inconvenience and discomfort they cause. Due to the intensive treatment process of TB, many patients develop irritation and have a great need for comfort. Both physical and mental distress might decrease patient cooperation. Common disposable surgical masks are available in white, light blue, and light green, among other colors. There is a tiny space between the mask and the face, allowing for reasonably easy breathing. The standard for disposable surgical masks is that they have an adequate barrier effect against microorganisms expelled by the wearer during breathing, speaking, coughing, and other activities. The rate of bacterial filtration reaches 95%.
The supervisory mechanism of hospitals has a significant impact on the wearing of masks by patients with TB, therefore, the management system of hospitals should be strengthened, nursing staff should strengthen the supervision of patients wearing masks, the relevant departments should be requested to provide free masks, and professional personnel should be equipped to give guidance in the relevant aspects of checkups and visits to the clinic to remind patients of the timely provision of masks. To remind patients diagnosed with TB to wear masks on time, helpful recommendations on mask use may be placed in functional departments and wards. In addition, a supervision team can be assembled to instruct patients on the proper usage of masks in the wards. They can inform patients that wearing masks can successfully prevent the spread of TB. In addition, they can underline that patients with TB who use surgical masks can effectively inhibit the emission of droplets and reduce the concentration of M. tuberculosis. This can help in preventing the spread of TB from patients.
Implementing appropriate nursing procedures and engaging in timely exchange and conversation with patients may increase their physiological and psychological comprehension of the need of mask use and their knowledge about TB. This eliminates the line of transmission, safeguards the susceptible population, and drastically minimizes the chance of cross-infection. The rate of accurate mask wear among hospitalized patients with TB in our department increased from 31.61% before implementation to 83.71% after implementation as a result of the QCC activities. This improvement in compliance with wearing surgical masks for patients undergoing external examinations effectively prevented the spread of TB. These results are consistent with those published by Wen et al.11
The implementation of QCC activities gives a platform for circle members to showcase their talents, in a way reflecting their sense of self-worth and enhancing their personal capabilities, communication skills, and teamwork. As a result, the quality control techniques of the circle members have significantly improved.12,13 The cohesiveness of the team has been reinforced as a result of the joint efforts and use of their collective skills among the department staff to address the issue. In addition, the proactive service mentality has been emphasized, resulting in enhanced nurse-patient communication and the development of a favorable doctor-patient connection. Thus, patient satisfaction has grown, and a harmonious and secure medical atmosphere has been established.
However, the limited study length and small sample size may have influenced the results. In the future, the sample size needs to be enlarged and additional observations and research need to be conducted. In addition, this study was limited to patients with TB at a single hospital and failed to collect pertinent data from other specialized facilities. Consequently, the data acquired from this study are extremely limited and susceptible to bias. If conditions allow, a multi-center study needs to be conducted, yielding more comprehensive and objective data.
Conclusion
QCC initiatives demonstrated considerable efficacy in enhancing adherence to mask-wearing protocols during external examinations of patients with TB. This enhanced compliance is instrumental in curtailing the spread of TB within healthcare environments. The objectives of this QCC initiative are threefold. Primarily, it seeks to safeguard both the patients and their immediate family members. Subsequently, it endeavors to regulate the dissemination of TB bacteria, thereby averting potential cross-contaminations within the hospital setting. Lastly, by interrupting the transmission vector, it aims to shield the vulnerable demographic and subsequently diminish the overall incidence of TB within the broader community.
Abbreviation
QCC, Quality Control Circle.
Data Sharing Statement
The datasets used and/or analysed during the current study available from the corresponding authors Jianjun Liu and Zunjing Zhang on reasonable request.
Ethics Approval and Consent to Participate
This study was conducted with approval from the Ethics Committee of Lishui Hospital of Traditional Chinese Medicine. This study was conducted in accordance with the declaration of Helsinki. Informed consent was obtained from all participants.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. World Health Organization. Global Tuberculosis Report 2023. Geneva: World Health Organization; 2023.
2. World Health Organization. World Health Statistics 2019: Monitoring Health for the Sdgs, Sustainable Development Goals. World Health Organization; 2016.
3. World Health Organization. Global Tuberculosis Report 2021. Geneva, Switzerland: World Health Organization; 2021.
4. Song R, Zhang Y, Hong S. Effect of nurse-family joint supervision mode on compliance behavior and treatment effect of young and middle-aged patients with pulmonary tuberculosis. Med Clin Res. 2017;34(012):2486–2488. doi:10.3969/j.issn.1671-7171.2017.12.081
5. Duan Z, Nie F, Hu F. Mask-wearing status of hospitalized tuberculosis patients. Chin Nurs Manage. 2013;2013:1.
6. Yin G, Tao Y, Chen L. The application of quality control circle and deming circle in nursing quality management. Chin Gen Pract. 2017;15(02):352–354. doi:10.16766/j.cnki.issn.1674-4152.2017.02.051
7. Li T, Liu Y, Li M, Qian X, Dai SY. Mask or no mask for COVID-19: a public health and market study. PLoS One. 2020;15(8):e0237691. doi:10.1371/journal.pone.0237691
8. Xu J, Wang Y, Liu F, Yang H. Changes of tuberculosis infection in mainland China before and after the COVID-19 pandemic. J Infect. 2023;86(2):154–225. doi:10.1016/j.jinf.2022.12.008
9. Lai CC, Yu WL. The COVID-19 pandemic and tuberculosis in Taiwan. J Infect. 2020;81(2):e159–e161. doi:10.1016/j.jinf.2020.06.014
10. General Office of the Chinese State Council. “13th Five-Year Plan” national tuberculosis control plan; 2017.
11. Wen Y, Yan X. Application of quality control circle in increasing face mask wearing rate of hospitalized pulmonary tuberculosis patients. Chin J Infect Control. 2015;2015:1.
12. Ma C, Zhang L, Li R. Quality control circle practice to improve the accuracy of NICU parenteral nutrition solution allocation. J Nurs. 2019;26(21):18–20. doi:10.16460/j.issn1008-9969.2019.21.018
13. Chen J, Fang WX, Li SJ, Xiao SX, Li HJ, Situ YL. Protective effect of ginsenoside rd on lipopolysaccharide-induced acute lung injury through its anti-inflammatory and anti-oxidative activity. World J Tradit Chin Med. 2021;7:383–390. doi:10.4103/wjtcm.wjtcm_12_21
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
