Back to Journals » Patient Preference and Adherence » Volume 18
Patients’ Experiences and Preferences for Medicine Information: An International Comparison Between Malaysia, Thailand, Uganda, and England
Authors Nualdaisri P , Corlett SA , Akaso I, Katusiime B, Kitutu FE, Chua SS , Krska J
Received 15 October 2023
Accepted for publication 11 January 2024
Published 23 January 2024 Volume 2024:18 Pages 239—248
DOI https://doi.org/10.2147/PPA.S444891
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Pitchaya Nualdaisri,1,2 Sarah A Corlett,2,3 Immaculate Akaso,4 Barbra Katusiime,5 Freddy Eric Kitutu,4 Siew Siang Chua,6 Janet Krska2
1Faculty of Pharmaceutical Sciences, Prince of Songkla University, Hat Yai, Thailand; 2Medway School of Pharmacy, Universities of Kent and Greenwich, Chatham Maritime, Kent, UK; 3Pharmacy Department, Medway Foundation NHS Trust, Kent, UK; 4Department of Pharmacy, School of Health Sciences, Makerere University, Kampala, Uganda; 5School of Life Sciences, Pharmacy and Chemistry, Department of Pharmacy, Kingston University, London, UK; 6School of Pharmacy, Faculty of Health and Medical Sciences, Taylor’s University, Subang Jaya, Selangor, Malaysia
Correspondence: Pitchaya Nualdaisri, Email [email protected]
Background: Verbal and written medicine information are available to the public but the quality, ease of access, ease of understanding and use of these resources varies greatly between countries. Timely access to quality medicine information is essential to support patient safety.
Objective: This international cross-sectional survey, conducted in low-to high-income countries, aimed to compare experiences of and preferences for medicine information sources among respondents with recent medicine use.
Methods: The survey was originally developed in England (Kent), then adapted and translated for use in southern Thailand (Songkhla), Malaysia (Klang Valley), and central Uganda (Kampala). Data were analysed using simple descriptive statistics and Chi-squared tests.
Results: A total 1588 respondents were involved in the study. Community pharmacies were the primary source of medicines in all four countries (40.7 to 65.3%). Most respondents (1460; 92%) had received at least one form of information with their medicine, but provision of written medicine information (WMI) varied between countries. A manufacturer’s leaflet was the most frequent information source for patients in England, while verbal information was common in Thailand, Malaysia and Uganda. There was commonality across countries in the desire for verbal information with or without WMI (1330; 84.8%); aspects of medicine information wanted most frequently were instructions on medicine use (98.3%), indication (98.2%), name (94.4%) and possible side effects (94.3%); and the importance of providing leaflets with all medicines (87.5%). Fewer than 10% in Uganda would use internet based WMI, compared to between 20% and 55% elsewhere.
Conclusion: Preferences for medicine information are similar across countries: verbal information is seen as most desirable, and the most wanted aspects of information are common internationally. Accessibility and understandability are key influences on preferred information sources. In-country regulations and practices should ensure that all medicine users can access the information necessary to maximise safe medicine use.
Keywords: medicine information sources, patient information leaflets, patient preference, cross-country comparison, international survey
Introduction
Providing accurate information about medicines is crucial for ensuring patient safety.1 Globally, different sources of medicine information are available in multiple formats.2 In the UK and Europe, a leaflet is regularly provided with all medicines, following European regulations.3 Verbal information from health professionals also plays an important role in informing people about medicines, as well as explaining and encouraging reading of written information.1,4 Other sources include health-related websites, television, advertisements, advice from family and friends, which may offer conflicting, inaccurate, poorly written, or non-evidence-based information.5 Patient preferences for sources of medicine information differ depending on age, sex, ethnic and cultural background, health and general literacy, duration of medicine use and experiences.6 A 2007 systematic review on the role and value of written medicine information (WMI) called for more research into the content, layout and delivery of WMI, particularly patient information leaflets (PILs), and Internet-based information.7
As available medicines information has increased world-wide, there is also greater variety in the studies investigating patients’ views and experiences. However, our scoping review identified only six surveys of medicine users from African and 25 from Asian countries.2 Therefore, studies are still needed in many low and middle-income countries to confirm needs and preferences, While surveys are reported more frequently from high-income countries, several UK studies report dissatisfaction with both written and verbal information.2 This study therefore surveyed members of the public from four countries; Uganda, a low-income country, Thailand and Malaysia, middle-income countries, and England, a high-income country, to compare access to and preferences for medicine information.
Method
The study surveyed the general population in terms of their medicine information source, and their preferences for information. The data were collected in south-east England (Kent), southern Thailand (Songkhla), Malaysia (Klang Valley), and central Uganda (Kampala).
Questionnaire Construction
Extensive review of the literature was used to identify key issues and previous surveys.2 These were used to develop the questionnaire in England (PN, SC, JK) through repeated brainstorming until consensus was reached. The questionnaire was presented to a group of members of the public established by Medway School of Pharmacy (England) for comment, then individual cognitive interviews undertaken with ten other members of the public to further assess content validity.
The final questionnaire used primarily closed questions in had four sections: demographic questions, experiences of receiving/accessing different medicine information sources, views on different potential medicine information sources in terms of ease of access, understandability, personal relevance and trustworthiness, and preferences/perceived needs for medicine information. It was translated into local languages for use in other countries using a forward and back translation method. The English version was also available for use in Uganda and Malaysia. The questionnaire was uploaded onto an electronic platform, and the survey delivery method was piloted in each country with up to 30 members of the public.
Main Survey Distribution
Convenience sampling was used in all four countries. The survey was conducted in public places such as shopping centers, bus stations, and hospitals, pharmacies, and health centers.
Research assistants administered the survey in each country in face-to-face interviews, using an electronic device or a hard copy. Informed consent was sought from each potential participant and recorded on the questionnaire prior to conducting the survey.
Inclusion and Exclusion Criteria
Respondents were required to be 18 years old or above, communicate verbally in one of the languages used and to be using at least one regular medicine or had used any medicine at all in the previous three months.
People who were unable to communicate in any of the languages used, were health professionals or training in health care sciences, or did not wish to participate were excluded.
Sample Size Calculation
The overall sample size required to detect a difference of 10% in the proportion of respondents who read a PIL between countries was 650, with 80% power at a probability of 5%. Sample sizes required for individual countries were then calculated using the formula: N= [(Zα/2)2 p (1-p)/d2], where (Zα/2)2 =1.96 assuming a normal distribution, p=proportion using medicine information based on previous studies and d=level of precision (95%). Thus, based on previous studies indicating receipt of medicine information or reading of it, sample sizes required were 288 in England, 310 in Thailand, and 245 in Malaysia. In Uganda, no previous studies were available, therefore since rates of medicine use and reading of WMI are potentially lower, an assumption was made that 50% of the population had accessed some form of medicine information. Here a cluster sampling approach was used, hence a correction factor of 1.9 was used to account for heterogeneity between clusters, giving a sample size of 730 across 76 outlets.
Ethical Issues and Informed Consent
The overall study was approved by the Faculty of Sciences Ethics Committee, University of Kent. The individual surveys in each country were also approved by Medway School of Pharmacy Ethics Committee (England), Prince of Songkla University Ethics Committee (Thailand), Makerere University School of Health Sciences Research Ethics Committee (Uganda) and Human Ethics Committee, Taylor’s University (Malaysia). This study complied with the Declaration of Helsinki.
Data Analysis
Data were analysed using Statistical Package for Social Sciences (SPSS) version 22. As well as simple descriptive statistics, Chi-squared tests were used to assess differences between countries, applying a Bonferroni correction, hence p values <0.001 were considered statistically significant.
Results
Demographic Information
The total number of respondents was 1588: England 300; Thailand 352; Uganda 694; Malaysia 242. General characteristics are shown in Table 1. Over half the respondents in all four countries were female. Half the respondents in Uganda and Malaysia were in the 18–30 age range, whereas the highest proportion of respondents in England and Thailand were 31–60 years. The largest proportion of respondents had a university degree in England, Thailand, and Malaysia while there were more respondents from Uganda with a secondary school qualification as their highest education award.
 |
Table 1 Demographic Information |
A very high proportion of respondents in both Uganda (95.7%) and England (81.0%) had used a medicine regularly (on most days) in the past three months, while the reverse was true in Thailand (22.4%) and Malaysia (20.3%).
Experiences and Use of Medicines Information
The most common source of medicines was community pharmacies: England (170, 59.0%); Thailand (230, 65.3%); Uganda (325, 46.8%); Malaysia (98, 40.7%). Hospitals were another important source in Thailand (202, 57.4%), Malaysia (160, 66.1%) and Uganda (203, 29.2%). Private clinics were a major source of medicines in Malaysia (120, 49.8%), while English respondents cited health centers (118, 39.3%) and drug/retail stores (70, 23.3%) more frequently than elsewhere (Supplementary Table 1).
The majority of respondents in all countries reported having received some information with their medicines: England (255, 85.0%), Thailand (344, 97.7%), Uganda (667, 96.1%), Malaysia (194, 80.2%). Among those receiving any information, written information including PILs, package inserts (PIs), websites, or information on the medicine container was cited more frequently (197, 77.3%) than verbal information (161, 63.1%) in England. Elsewhere, written information was reported less often than verbal: Thailand 91.3% (314) verbal and 65.1% (224) written; Malaysia 88.6% (178) verbal and 52.2% (105) written; Uganda 85.9% (573) verbal and 77.6% (518) written (Supplementary Table 2).
The majority of respondents reporting having received written information in both England and Thailand indicated this was a leaflet provided in the medicine pack (Table 2). Considerably fewer respondents in Uganda and Malaysia reported receiving such a leaflet, instead the most common written information source in these countries was the manufacturer information on the medicine container. Dispensing labels/written instructions were more frequently cited than manufacturer information in England and Thailand, while the reverse was true in Uganda and Malaysia. A significantly higher proportion of respondents from England and Thailand also reported having seen information on adverts or websites than in Uganda or Malaysia (Table 2).
 |
Table 2 Written Medicine Information Sources |
More Thai respondents reported never looking at the written information they received than those from other countries (Table 3). However, of those who did read the information, significantly more Thai respondents (128, 67.4%) claimed to read it more than once than those elsewhere (range 45.8% to 55.2%). The majority of respondents everywhere looked at written information when they were first given the medicine, although again fewer in Thailand than in other countries did so (Table 3), where a higher proportion looked at it when something unexpected happened. The most common overall reason given for looking at the information was to find out how to use the medicine, although more Thai respondents than others looked at it to find out if the medicine was suitable for them, while more English respondents sought possible side effects (Table 3). Other ways in which written information was used are shown in Table 3.
 |
Table 3 Use of Written Medicine Information |
A low proportion of respondents in all countries considered that they needed more information, although the proportion was higher in Malaysia (20.6%) than elsewhere (England 9.5%; Uganda 9.6%; Thailand 11.9%). The majority of respondents in England, Uganda and Malaysia considered the information they had received easy/very easy to understand (87.1%, 81.5% 79.8% respectively), compared to only 52.3% of Thai respondents (Figure 1).
 |
Figure 1 Views on ease of understanding of all information received. |
Views on Different Medicine Information Sources
The most frequent source of medicine information that respondents from all four countries indicated they would use was verbal information from health professionals (range 91.7% to 98.9%) (Table 4), with ease of understanding being the most common reason for doing so (Supplementary Table 3). Many respondents in Thailand and Uganda would also use leaflets provided by health professionals, with trustworthiness being the most commonly cited reason. Information on the medicine container, both provided by the manufacturer and the dispenser/supplier were more commonly identified as an information source respondents would use in Thailand, Malaysia, and Uganda than in England (Table 4), although all considered ease of access and understanding as factors influencing this.
 |
Table 4 Possible Use of Medicine Information Sources |
In both England and Thailand, over 70% of respondents indicated they would use the leaflet supplied with a medicine, but this proportion was much lower in Malaysia (48.4%) and Uganda (43.0%) (Table 4). Reasons for using this leaflet also differed, with ease of access being the most common reason in both England and Malaysia, whereas few Ugandan respondents considered them easy to access (Table 5). A low proportion of Thai respondents rated leaflets as relevant to them, citing ease of understanding as the most common reason. Fewer respondents in Thailand and Uganda than in England or Malaysia considered such leaflets trustworthy (Supplementary Table 3).
 |
Table 5 Reasons for Using a Leaflet Provided with Medicines |
More than half the respondents in England and Thailand indicated they would use information on websites. The proportion who would use websites was around a third in Malaysia and less than 10% in Uganda (Table 4), with ease of access being the most frequently cited reason for their use. Government websites were considered the most trustworthy in both England and Thailand, but in Malaysia and Uganda, manufacturer websites were considered trustworthy by more respondents.
More than half the Thai respondents also indicated they would use other sources, such as advertising, news reports and mobile applications, whereas these were less popular sources in other countries; the most common reasons cited were ease of access and understanding. Social media, friends and family were cited by 28.6% of all respondents, the highest proportion being in Thailand and the lowest in Uganda.
Preferences for Medicine Information in Future
The proportion of respondents in all four countries who preferred only receiving written information about medicines was similar, 11.2% to 16.0% (Figure 2). The proportion preferring only verbal information was highest in Uganda (300, 43.3%) and lowest in England (77, 25.7%), while those preferring both verbal and written information was highest in England (175, 58.3%) and lowest in Uganda (285, 41.1%) (Figure 2). A small number of respondents indicated a preference for information via other routes including social media, friends and family and television in both Thailand (5, 1.4%) and Malaysia (18, 7.9%).
 |
Figure 2 Preferences for form of medicine information. |
Of those desiring written medicine information, the most preferred option among English respondents (152, 67.9%) was a leaflet with the medicine, whereas the most preferred source for respondents elsewhere was the medicine container: Thai (149, 68.7%), Ugandan (339, 86.3%) and Malaysian (87, 62.6%). However, 87.5% of those giving an opinion considered that providing leaflets with medicines to all patients was extremely/very important: Uganda 94.4%; Thailand 90.0%; Malaysia 80.4%; England 79.7%. Information on a website was preferred by small numbers in each country, being highest in England (35, 15.6%) and Malaysia (14, 10.1%). Despite this, the majority of respondents in Malaysia (79.6%), Thailand (71.5%) and England (52.7%) considered it extremely/very important to provide information on a government website; insufficient responses to this question were received in Uganda.
Respondents from all four countries had similar views on the four most necessary aspects of written information: how to use the medicine (98.3%), indication (98.2%), name of medicine (94.4%) and possible side effects (94.3%) (Table 6).
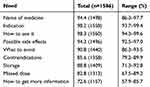 |
Table 6 Need for Aspects of Written Medicine Information |
Discussion
Information Sources
Community pharmacies were the most common source of medicines in all four countries, but fewer English respondents received verbal information about their medicine than in Thailand, Uganda and Malaysia. Many previous studies from around the world show verbal information from health professionals is the main source of medicine information2,6,8–15 Our findings confirm previous studies2,7,16–18 suggesting a large majority of people prefer to receive verbal information from a health worker, with or without written information because of ease of understanding and trustworthiness.
A higher proportion of respondents in England received written information, particularly a medicine leaflet, than in the other countries and most prefer it as their written source of information, because of easy accessibility. Fewer respondents in Uganda and Malaysia reported receiving a leaflet than in England or Thailand. The majority of Thai respondents had received a leaflet with their medicine, but few considered such leaflets relevant to them. Thai respondents were also least likely to look at the written information provided with their medicine. Overall, the provision of leaflets with medicines was considered important by 87.5% of respondents.
In Uganda and Malaysia, manufacturer information on the container was a more commonly reported information source than leaflets, however, although this was considered useful by many respondents in all four countries, the instructions provided by the medicine supplier were consistently preferred over manufacturer information.
Many respondents in England, Thailand, and Malaysia would also consider using other information sources such as websites, mobile applications, and social media, as has been found in other countries,19 although this was less common in Uganda. Almost a fifth of Malaysian respondents considered they needed more information, similar to other studies,1,19,20 more than in the other three countries. Overall, this suggests that the information received, whether written, verbal or both, was perceived as sufficient for their needs by the majority of respondents. However, it is acknowledged that perceived needs are affected by participants’ lived experiences and when describing their needs individuals reflect through their own lens.
Regulations and Practices
Differences in experiences and views between the four countries may be due in part to differing regulations and medicine supply practices. In England, almost all medicines are supplied as original packs which include a PIL, the content of which has been regulated since 1977.3 It is therefore unsurprising that leaflets were the most commonly encountered and most preferred written information source in England and considered easy to access. The age distribution of our sample which meant that a high proportion used regular medicines may also have resulted in greater familiarity with PILs. The results are similar to a previous survey in which most people considered PILs easy to access, but fewer considered them trustworthy.21 PILs are subjected to user-testing22 prior to use, which may explain why English respondents were most likely to find leaflets and written information overall easy to understand.
In Thailand, regulations require that a written package insert (PI) in Thai be provided,23 but PILs are voluntary and infrequently produced by manufacturers. If full packs are purchased, the leaflet within is therefore most likely to be a PI, designed for health professionals, rather than a PIL, designed for patients.18,24 Guidelines for preparing PILs were introduced in Thailand in 2013,25 and many generic PILs for commonly used medicines are produced by the Thai regulatory body and available on a website,26 which people find easier to read than PIs.27 In practice, however, many medicines in Thailand are supplied as individual strips in pre-printed plastic bags on which dosage instructions are hand-written, thus the PI contained within the original pack is not provided to the purchaser. Therefore, while Thai patients have experience of receiving leaflets and over 80% of the respondents in our survey would use them, more would use the information on the container, either manufacturer information, or instructions written by the supplier.
In Uganda, guidelines exist for written information supplied with medicines, which must contain either a PI or a PIL.28 However, as in Thailand, medicines are frequently provided as part-packs, or strips, in envelopes with hand-written dosage instructions. This was the most common source of WMI reported. The use of original packs with leaflets is much less frequent, hence Ugandan respondents were least likely to have received a leaflet with a medicine and very few considered them easy to access. Medicines are available from community pharmacies in Kampala and other cities, but in rural areas, they are mainly supplied from health centers and licensed drug shops, where a trained health professional is usually, but not always, present,29 or other unlicensed medicine outlets. Staff supplying medicines from health centres must provide verbal information,30 which, together with cultural expectations of verbal advice, may have influenced the strong preference for verbal information. No previous studies have examined the availability of WMI in Uganda, but there may be a general paucity of written information. This, together with low health literacy levels, may contribute to poor medicine use and information practices, such as medicine sharing, known to be widespread in Uganda.31 Perhaps because of the apparent lack of WMI, almost all respondents in Uganda considered it important to provide leaflets with medicines to all patients. Potential use of websites and social media as information sources was, not surprisingly, much lower in Uganda than elsewhere, given that Uganda has the lowest percentage of people utilizing the Internet of the four countries.32
In Malaysia, original packs are more commonly provided. Regulations require that, if a product is sold without a PIL, all the information expected on a PIL must be printed on the product label.33 Leaflets must be aimed at consumers and available in English and Malay. However, a study of 133 over-the-counter products found that 31% were sold without PILs, plus wide variation in the content of leaflets and labels.34 Only 40% of Malaysian respondents in our study reported receiving a leaflet with a medicine and they were the least likely to use one. A previous survey in Penang found the majority of the general public had adequate information about their medicines, with over 80% reading the label for dosage and directions for use, but fewer reading the ingredients, indication and safety information.17 Poor medicine practices including medicine sharing have also been found in Malaysia.35 A quality use of medicines campaign attempting to improve this suggested that television, radio and the internet were potentially useful methods of promoting safe medicine use.36 Only around 20% in our survey would use television and radio as information sources, while slightly more would use government and manufacturer websites.
Strengths and Limitations
The strengths of this study were that the survey was developed with general public involvement and tested in each country prior to use. The sample size was sufficiently large to enable comparisons between countries. It is also the first such survey to be reported from Uganda.
However, there were necessarily limitations. The geographical sub-regions were conveniently selected and tended to exclude rural populations, plus we used convenience sampling methods, therefore our findings should not be generalized beyond these regions. The number of people approached who declined to participate was not recorded. The higher proportion of females to males in all four countries is not unusual for health-related surveys, however the proportion with a university education was above the national average for Thailand and Malaysia. This would have affected literacy levels and thus views and experiences. We did not attempt to measure literacy levels. In Uganda, all respondents were recruited from health-related centers to increase the probability of recent medicine use, hence the proportion using medicines regularly was higher than in other countries.
Conclusion
The preferred source of medicine information is verbal, from health professionals. Ease of access to written information is a key determinant of its use; the medicine packaging is therefore an important source. Respondents from all countries agreed on their key information needs. Therefore regulations, where these exist, which guide the nature and content of PILs should be enforced to ensure that all users are provided with written information which is easy to access and trustworthy, thereby facilitating informed patient choice and safe medicine use.
Practice Implications
Over 80% of all respondents wanted verbal information. Therefore, healthcare professionals need to provide such information using good communication techniques to ensure patient recall and understanding.23,25,37
Respondents in all four countries desire WMI and most consider the provision of leaflets an important mechanism. The desirable content of WMI was consistent across the four countries, and in line with that found in other studies.7,38 While most found the WMI they had received easy to understand, previous studies have shown that use of local languages with or without pictograms, and simple, non-medical terms are important.38
Funding
This work was supported by a Royal Thai Government Ph.D. Scholarship for Pitchaya Nualdaisri.
Disclosure
The authors have no conflicts of interest to declare.
References
1. Raynor DT. The importance of medicines information for patients. Prescriber. 2007;18(2):60–62. doi:10.1002/psb.15
2. Nualdaisri P, Corlett SA, Krska J. Provision and need for medicine information in Asia and Africa: a scoping review of the literature. Drug Saf. 2021;44(4):421–437. doi:10.1007/s40264-020-01038-8
3. Letts M. Always Read the Leaflet Getting the Best Information with Every Medicine. London: TSO (The Stationery Office); 2005.
4. World Health Organization. Promoting rational use of medicines. Available from: https://www.who.int/activities/promoting-rational-use-of-medicines.
5. Kusch MKP, Haefeli WE, Seidling HM. How to meet patients’ individual needs for drug information-A scoping review. Patient Prefer Adherence. 2018;12:2339–2355. doi:10.2147/PPA.S173651
6. Ho CN, Ko Y, Tan ML. Patient needs and sources of drug information in Singapore: is the internet replacing former sources? Ann Pharmacother. 2009;43(4):732–739. doi:10.1345/aph.1L580
7. Raynor DK, Blenkinsopp A, Knapp P, et al. A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines. Health Technol Assess. 2007;11(5):1–6.
8. Patel S, Dowse R. Understanding the medicines information-seeking behaviour and information needs of South African long-term patients with limited literacy skills. Heal Expect. 2015;18(5):1494–1507. doi:10.1111/hex.12131
9. Raynor DK, Savage I, Knapp P, Henley J. We are the experts: people with asthma talk about their medicine information needs. Patient Educ Couns. 2004;53(2):167–174. doi:10.1016/S0738-3991(03)00126-5
10. Balmer C. The information requirements of people with cancer: where to go after the ‘patient information leaflet’? Cancer Nurs. 2005;28(1):36–46. doi:10.1097/00002820-200501000-00005
11. Krska J, Morecroft CW. Patients’ use of information about medicine side effects in relation to experiences of suspected adverse drug reactions: a cross-sectional survey in medical in-patients. Drug Saf. 2013;36(8):673–680. doi:10.1007/s40264-013-0065-3
12. Saleem H, Ghoto MA, Memon N, Dayo A, Suheryani I, Shafique S. Assessment of patients awareness towards pharmacotherapy and their sources of drug information in different areas of Hyderabad, Pakistan. Int Res J Biol Sci. 2015;4(8):56–59.
13. Sevikyan A, Kazaryan I, Amirkhanyan A, Melikyan M. Patients’ expectations on receiving medicines information from community pharmacies. Res Soc Adm Pharm. 2017;13(3):e10–e11. doi:10.1016/j.sapharm.2017.02.088
14. Perera T, Ranasinghe P, Perera U, et al. Knowledge of prescribed medication information among patients with limited English proficiency in Sri Lanka. BMC Res Notes. 2012;5(1):1. doi:10.1186/1756-0500-5-658
15. Hamrosi KK, Raynor DK, Aslani P. Pharmacist, general practitioner and consumer use of written medicine information in Australia: are they on the same page? Res Soc Adm Pharm. 2014;10(4):656–668. doi:10.1016/j.sapharm.2013.10.002
16. Liu LST, Goh BQ, Tang WP, Lo FL, Khoo RSY, Lim CJF. Drug information needs and concerns of primary care patients with newly prescribed chronic medications. Proc Singapore Healthc. 2018;27(4):294–298. doi:10.1177/2010105818779605
17. Dawood OT, Hassali MA, Saleem F, Ibrahim IR. Assessment of self-reporting reading of medicine’s labels and the resources of information about medicines in general public in Malaysia. Pharmacol Res Perspect. 2018;6(2). doi:10.1002/prp2.387
18. Wongtaweepkij K, Krska J, Pongwecharak J, Jarernsiripornkul N. Experiences and views of medicine information among the general public in Thailand. Patient Prefer Adherence. 2020;14:1073–1082. doi:10.2147/PPA.S257454
19. Amin MEK, Chewning BA, Wahdan AMH. Sources of drug information for patients with chronic conditions in Alexandria, Egypt. Int J Pharm Pract. 2011;19(1):13–20. doi:10.1111/j.2042-7174.2010.00069.x
20. Afolabi MO, Akinwale VO, Akinyemi OA, Irinoye AI. Patient use and perception of medicine information leaflets. Pharmacoepidemiol Drug Saf. 2012;21(1):110.
21. O’Donovan B, Rodgers RM, Cox AR, Krska J. Use of information sources regarding medicine side effects among the general population: a cross-sectional survey. Prim Heal Care Res Dev. 2019;20(e153):1–9.
22. European Commission. Guideline on the readability of the label and package leaflet of medicinal products for human use. EC Pharmaceuticals Committee. 2009. Available from: https://ec.europa.eu/health/sites/health/files/files/eudralex/vol-2/c/2009_01_12_readability_guideline_final_en.pdf.
23. Thai food and drug administration. guideline for leaflet development for drug research and innovation 2019. Available form: https://www.fda.moph.go.th/sites/oss/SharedDocuments/SmPC-PIL_HPEPguideline_updatedMay2019.pdf.
24. Phueanpinit P, Pongwecharak J, Krska J, Jarernsiripornkul N. Medicine information leaflets for non-steroidal anti-inflammatory drugs in Thailand. Int J Clin Pharm. 2016;38(1):25–29. doi:10.1007/s11096-015-0220-2
25. Thai Food and Drug Administration. Guideline for Leaflet Development for Drug research and Innovation 2013. Available from: http://www.rapat.or.th/images/column_1344932177/ya-20131219-03.pdf.
26. Division of Innovative Health Products. Patient information leaflets. 2022. Available from: https://www.fda.moph.go.th/sites/oss/SitePages/patientinformaionleafletpage2.aspx.
27. Wongtaweepkij K, Krska J, Pongpunna S, Jarernsiripornkul N, Jarernsiripornkul N. Thai patients drug safety knowledge and perceptions relating to different forms of written medicine information: a comparative study. Patient Prefer Adherence. 2022;Volume 16:1141–1152. doi:10.2147/PPA.S361447
28. Ministry of Health Uganda. The national drug policy and authority (registration) regulations. 2014. Available from: https://www.nda.or.ug/wp-content/uploads/2022/03/Drug-Registration-Regulation.pdf.
29. Mayora C, Kitutu FE, Kandala NB, Ekirapa-Kiracho E, Peterson SS, Wamani H. Private retail drug shops: what they are, how they operate, and implications for health care delivery in rural Uganda. BMC Health Serv Res. 2018;18(1):1–12. doi:10.1186/s12913-018-3343-z
30. Ministry of Health Uganda. National drug authority. Available from: https://www.nda.or.ug/.
31. Kalyango JN, Hall M, Karamagi C. Home medication management practices and associated factors among patients with selected chronic diseases in a community pharmacy in Uganda. BMC Health Serv Res. 2012;12(1). doi:10.1186/1472-6963-12-323
32. The World Bank. Individuals using the Internet (% of population) - Thailand, Uganda, Malaysia, United Kingdom. 2022. Available from: https://data.worldbank.org/indicator/IT.NET.USER.ZS?locations=TH-UG-MY-GB.
33. National Pharmaceutical Regulatory Agency (NPRA) Ministry of health Malaysia. drug registration guidance document (drgd) third edition, third revision 2022.Available from: https://www.npra.gov.my/index.php/en/component/sppagebuilder/925-drug-registration-guidance-document-drgd.html.
34. Mittal P, Gan XY, Sim AY, et al. Adherence of safety information on over-the-counter product labels and leaflets to the regulatory guidelines in Malaysia. J Pharm Pract Res. 2018;48(3):204–211. doi:10.1002/jppr.1351
35. Dawood OT, Hassali MA, Saleem F. Factors affecting knowledge and practice of medicine use among the general public in the state of Penang, Malaysia. J Pharm Heal Serv Res. 2017;8(1):51–57. doi:10.1111/jphs.12167
36. Ting CY, Abd Wahab MS, Lee KS, Tan RTH, Ming LC. A cross-sectional study on the use of, preference for, and perceived reliability of mass media for drug-related information among the general public in Sarawak. Ther Innov Regul Sci. 2017;51(2):212–220. doi:10.1177/2168479016674041
37. Roter DL, Rudd RE, Comings J. Patient literacy, a barrier to quality of care. Commun Heal Educ. 1998;13:313–341.
38. Nualdaisri P, Corlett SA, Krska J. The effectiveness and value of written medicine information across Asia and Africa: systematic review. Drug Saf. 2021;44(12):1283–1295. doi:10.1007/s40264-021-01114-7
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
