Back to Journals » International Journal of Women's Health » Volume 16
Multimodal and Interdisciplinary Interventions for the Treatment of Localized Provoked Vulvodynia: A Scoping Review of the Literature from 2010 to 2023
Authors Rains A , Bajzak K , Miller ME, Swab M , Logan GS , Jackman VA, Gustafson DL
Received 29 September 2023
Accepted for publication 13 December 2023
Published 15 January 2024 Volume 2024:16 Pages 55—94
DOI https://doi.org/10.2147/IJWH.S436222
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Marleen van Gelder
Alex Rains,1 Krisztina Bajzak,2 Michelle E Miller,2 Michelle Swab,3 Gabrielle S Logan,4 Victoria A Jackman,5 Diana L Gustafson6
1Department of Medicine, University of Chicago, Chicago, IL, USA; 2Discipline of Obstetrics and Gynecology, Memorial University, St. John’s, Newfoundland & Labrador, Canada; 3Health Sciences Library, Faculty of Medicine, Memorial University, St. John’s, Newfoundland & Labrador, Canada; 4Department of Anesthesiology, Perioperative and Pain Medicine, Max Rady College of Medicine, University of Manitoba, Winnipeg, MB, Canada; 5Faculty of Medicine, Memorial University, St. John’s, Newfoundland & Labrador, Canada; 6Division of Community Health and Humanities, Faculty of Medicine, Memorial University, St. John’s, Newfoundland & Labrador, Canada
Correspondence: Alex Rains, Email [email protected]
Introduction: Localized provoked vulvodynia (LPV) is a chronic condition characterized by pain in the vulvar vestibule, which can be provoked by pressure or touch and which is not tied to a clear underlying cause. Research into the etiology of and most appropriate treatment strategy for LPV is still limited.
Methods: Using Arksey and O’Malley’s model for scoping reviews, we evaluated the research question: what is the current evidence regarding the efficacy/effectiveness of multimodal or interdisciplinary interventions for the treatment of LPV? We collated and analyzed articles from 2010 to 2023 to capture the current research landscape.
Results: Our review identified 27 studies, which either compared treatments between classes (eg pharmacologic versus psychologic modalities) or described interdisciplinary treatment programs. We identify several trends in the literature. First, outcome measures are inconsistent between studies, often unvalidated, and may not adequately mirror patient concerns. Second, the absence of appropriate comparator groups in many studies restricts providers’ ability to appraise which treatments may be most efficacious. Third, selection bias and demographic homogeneity limit generalizability. Finally, we highlight the need for head-to-head trials of vestibulectomy with other treatments considered first line for vulvodynia management.
Conclusion: There is insufficient evidence to suggest the superiority of one treatment modality for LPV relative to others or to recommend a particular interdisciplinary management strategy. Future research should use a head-to-head design where sham control is impossible, incorporate patient-centered outcome measures, and investigate impacts of treatment among diverse samples of LPV patients.
Keywords: multidisciplinary, interdisciplinary, multimodal, chronic pain, vulvodynia, dyspareunia
Introduction
Chronic pain is recognized as a significant public health burden that impacts the social, emotional, and physical functioning of those living with it.1 Among a wide range of chronic pain conditions is vulvodynia, a vulvar pain condition of at least 3 months’ duration unrelated to a clear underlying cause.2 Vulvodynia may be generalized to the whole of the vulva, or localized to specific structures such as the clitoris and vestibule. It may be provoked by touch or vaginal insertion, or occur independent of provocative stimuli.2 The most common form of vulvodynia is localized provoked vulvodynia, or LPV.3 While the exact etiologies of each form of vulvodynia remain to be determined, LPV is the most well-studied given its relative prevalence.
The Vulvodynia Guideline4 and 2013 Vulvodynia Guideline Update5 have played a pivotal role in influencing clinical care for LPV. These documents provide a treatment algorithm consisting of vulvar care measures, topical, oral and injectable medications, physiotherapy and biofeedback, dietary modifications, supplements, and psychological therapies, with vestibulectomy reserved as last-line management. In the absence of a professional society-endorsed guideline with recommendations graded by evidence, many clinicians derive their management strategies from these publications. The continued paucity of clear consensus recommendations for LPV treatment may contribute to the high variability of practice patterns among providers.6
The underlying mechanisms of pain in vulvodynia are not well understood. Allodynia of the vestibule, as demonstrated by cotton swab testing (CST) on examination, implies a neuropathic component. Pelvic tension myalgia is a frequent comorbidity and psychological and relationship distress often accompany physical symptoms. Given this constellation of symptoms and findings, multimodal therapy would seem to be an intuitive approach. However, many existing recommendations for multimodal management of LPV are extrapolated from findings in other chronic pain literature,7 with limited evidence to propose how pain due to vulvodynia directly maps onto the mechanisms of other chronic pain conditions.8 To evaluate multimodal interventions specifically directed towards management of vulvodynia, this scoping review aims to synthesize literature published since 2010 evaluating the efficacy of multimodal approaches to the management of LPV.
Methods
To identify, collate, and evaluate relevant literature that addresses the question of the effectiveness or efficacy of treatments and interventions in the management of LPV, this scoping review employs Arksey and O’Malley’s five-stage framework.9
A team that included a health sciences librarian and content and methodology experts developed a search using controlled vocabulary and keyword terms relating to LPV management from 2010 to 2021. An updated search of the literature from 2021 to March 2023 was subsequently undertaken. The initial search was run in PubMed and translated into other subject-specific databases (Appendix 1). The start date was selected because the knowledge and nomenclature around vulvodynia has evolved with time, and we aim to capture contemporary findings and insights around LPV management.
There is no clear consensus as to terminology describing interventions that incorporate multiple treatment modalities into a single treatment program. Authors referred to these interventions as multidisciplinary (ie, work involving multiple separate disciplines) or interdisciplinary (ie, integrating treatment categories to create a synthesized whole). For clarity in our review, we refer to these publications as interdisciplinary. Studies of multimodal (ie, studies comparing interventions across classes not integrated into a single treatment program) management of LPV were also included in this review.10 Appendix 2, outlines inclusion and exclusion criteria. Only primary studies were selected. Reviews and meta-analyses were excluded. Studies that did not include a clear diagnosis of LPV were excluded. Studies where treatments implied underlying pathology were excluded, as vulvodynia is defined as having no identifiable underlying cause.11,12 Articles that focused on diagnosis or risk factors were also excluded. Studies focused on a single class of intervention (ie, pharmacological, psychological, and physical modalities) were separated out into multiple publications given the volume of studies and are reported elsewhere.13 Studies of somatocognitive therapy14,15 are described in the psychological therapies publication rather than here, as the emphasis of these interventions is on developing conscious bodily awareness and cognitive retraining to change movement and function. Somatocognitive therapy is a unique, psychologically oriented intervention delivered by a group of physiotherapists in Norway. While the practice combines cognitive psychotherapy with therapeutic principles of Mensendieck physiotherapy, the psychological component of intervention differentiates it from interdisciplinary programs, which incorporate both physiotherapy and psychological treatments as independent components of care.
Covidence, a literature review management tool, was used to store and screen all databases’ search results. Title and abstract screening and full-text screening were completed by two reviewers. Consensus between two content experts (KB and MM) was used to resolve any disagreements around study inclusion at these stages. Data were extracted within Covidence by one reviewer and confirmed by a second to ensure accuracy. A comprehensive narrative synthesis of study findings was compiled.
Results
The review produced 27 publications between 2010 and 2023 that compared treatments across modalities or applied multimodal/interdisciplinary approaches (see Figure 1 for PRISMA diagram16). Study details are summarized below and charted in Tables 1–2.
 |
Figure 1 PRISMA 2020 Flow Diagram. Abbreviations: PRISMA, preferred reporting items for systematic reviews and meta-analyses; LPV, localized provoked vulvodynia. Notes: Adapted from Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Online). 2020;37:n71. doi:10.1136/bmj.n71.16 |
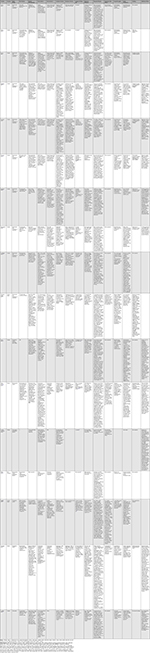 |
Table 1 Multimodal Studies |
 |
Table 2 Interdisciplinary Program Studies |
Physiotherapy versus Pharmacologic Interventions
One randomized treatment versus treatment trial by Morin et al produced three publications17–19 comparing topical lidocaine 5% ointment applied to vestibule nightly versus weekly physiotherapy sessions, including manual techniques and education from a physical therapist. The first publication17 followed 181 patients randomized to a 10-week course of either treatment. Both treatments showed improvements in pain and sexual distress, though only physiotherapy yielded improvements in sexual function and self-assessed improvement. The second publication18 followed 201 participants (including the 181 from the 2015 study) randomized to the treatments discussed above. Findings were consistent with a prior study.17 The third publication19 followed the same cohort as the 2016 publication with 195 of the 201 participants assessed 6 months after the end of treatment. The study found that physical therapy had superior outcomes in pain with intercourse, pain quality, sexual function, sexual distress, satisfaction, and participants’ impression of change both at post-treatment and at 6-month follow-up. Among the final sample, 1 participant dropped out due to a dermatitis reaction to lidocaine and 15 participants (15%) reported minor irritation. No other adverse events were reported.
Psychotherapy versus Pharmacologic Interventions
Three randomized treatment versus treatment trials compared 12 weeks of cognitive-behavioral couple therapy (CBCT) sessions with participants and their partners with topical 5% lidocaine ointment applied to the vestibule nightly. Two publications20,21 followed the same 108 participants. The third publication22 followed 84. One report20 found improvements in sexual function, sexual distress, and pain catastrophizing at post-treatment and 6-month follow-up among both groups, though those in the CBCT group experienced greater satisfaction with treatment and had greater improvements in anxiety and pain catastrophizing. Other publications21,22 examined sexual communication patterns (SCP), which may be associated with relational and sexual satisfaction, between participants and their partners throughout the course of treatment. A 2022 study21 reported that improved collaborative communication mediated the effect of CBCT, but not lidocaine, on sexual satisfaction, function, and distress. This study also found that neither group of partners reported improvement to negative SCP with time.21 A 2017 study reported that collaborative SCP increased with CBCT but not lidocaine.22 Contrary to a 2022 study, they found that negative SCP significantly decreased for participants and their partners over the course of CBCT, with participants in the lidocaine group also reporting decreased negative SCP.
These studies had a randomized design and close participant monitoring, but there was no control for attention from a health professional, which the authors felt may have accounted for some outcomes. There was also no control for continued use of lidocaine or CBCT homework exercises during the follow-up period. Exclusion criteria prohibited the engagement of those not attempting penetrative sexual activity or who experienced significant relational distress or health problems. Regarding treatment adherence, two studies20,21 found that couples in CBCT attended an average of 10.6 out of 12 sessions and completed 63% of homework exercises, while participants in the lidocaine arm applied the cream 79.4% of nights in the treatment period. Five couples assigned to CBCT in the 2017 study22 dropped out over the course of therapy, and three participants withdrew from lidocaine treatment.
Two randomized studies compared a ten-session group CBT (GCBT) program with topical 1% hydrocortisone cream applied twice daily to the vulvar vestibule for the same period. The first followed 97 participants, 52 of whom received GCBT, and 45 who received hydrocortisone.23 The second followed 97 participants, 46 of whom received GCBT and 51 who used hydrocortisone.24 The first study reported improved pain during intercourse and sexual dysfunction in both groups, with GCBT producing greater decreases in pain and pain catastrophizing, increased treatment satisfaction, and improved global pain.23 The other found improvements in pain and sexual function at post-treatment and 6-month follow-up in both groups, with greater effects in the GCBT group.24 Neither study had a placebo group and each only offered one medical management option.
Psychotherapy versus Physiotherapy
One study25 compared individual CBT (ICBT) to pelvic floor physiotherapy. Twenty women were randomly assigned to one of the eight-session treatment programs. Outcome measures related to pain and sexual functioning were assessed pre- and post-treatment, and at 6-months post-treatment. Both treatment groups showed improvement in pain with intercourse that persisted up to 6 months with no statistically significant differences between treatment groups. Furthermore, ICBT resulted in improved sexual functioning and physiotherapy resulted in reduced pelvic floor muscle tone. Underpowering and the absence of a control group may limit interpretation of findings. The author concluded that women with LPV who present with pelvic hypertonicity may be better suited for pelvic floor rehabilitation, whereas women with high pain rumination or sexual functioning problems may be better suited for ICBT.
Multimodal Treatment versus Multimodal Treatment
One study26 recruited 19 (of an intended 30) LPV participants randomized to either “traditional acupuncture” (TA) or “non-traditional acupuncture” (NTA) for 18 treatments over 12 weeks. Both groups also used vestibular lidocaine 5% ointment four times daily. Authors did not consider NTA to be a “sham” procedure as they state that acupuncture needle insertion affects circulating endogenous opioids and their receptors. Outcomes were assessed post-treatment and 3 months later. While ten were randomized to TA and nine to NTA, only seven participants per group were included in the final analysis, precluding statistical comparisons. Almost all had tried medication and physiotherapy, although it was unclear if use was ongoing. Baseline vulvar VAS pain by participant recall was higher in the NTA group. While some pain outcomes were comparable or favored TA at 12 weeks, 24-week outcomes favored NTA. Participants expected a 60% pain reduction, and tampon test and CST pain VAS improved from 30% to 60%. More NTA participants were satisfied with their pain relief. Participant blinding was effective, with only 2 (14%) correctly guessing group assignment. Participants were highly compliant. Five adverse events attributed to acupuncture were considered mild and two dropouts were attributed to lidocaine. Authors concluded that acupuncture for LPV was acceptable, well tolerated, and warrants further investigation.
Descriptive Studies Involving Multiple Interventions/Interdisciplinary Classes
A case series35 evaluated a combination of pelvic muscle floor therapy (PMFT) and lidocaine 2% gel without a comparator. This study evaluated general wellbeing and health, perceived vulvar pain, sexual function, and pain with vaginal penetration among 45 participants. Participants underwent 30-min sessions with a physiotherapist, which involved vulvar desensitization with lidocaine as well as education, use of vaginal dilators, lifestyle counseling, and sexuality coaching. Duration of treatment varied based on individual progress, lasting 4–20 sessions. Authors reported improvements in all measures but acknowledge that no RCTs exist which study this intervention more rigorously.
Another case series36 evaluated three partnered patients who were treated with oral amitriptyline, vestibular estrogen and hydrocortisone creams, and biweekly behavioral sex therapy, which involved use of vaginal dilators and sensate focus exercises (engaging in non-penetrative forms of physical intimacy with a partner). Duration of treatment spanned from 5 to 16 sessions with a behavioral sex therapist. While partners were encouraged to join therapy sessions, only one of the three participants’ partners attended these sessions consistently. Authors reported this participant experienced “gratifying” intimacy and minimal pain with intercourse and another reported successful resumption of spontaneous intercourse with her partner and that the final participant withdrew due to relationship issues. Authors concluded that pain improved in scenarios where couples were motivated to follow the treatment protocol, but acknowledged that general conclusions could not be made based on the small number of cases.
A case series37 examined the efficacy of 5% dextrose injections administered after application of a multi-agent topical anesthetic followed by 3 min of compression daily for 3 days prior to “central core excision” of the 12 o’clock region of the vestibule in patients who had failed posterior vestibulectomy. This intervention was offered to participants with >4/10 NRS pain with CST. Fourteen participants had mean age 30 and mean NRS pain 7.3/10 had pain reduction to 2.8/10 after three days of injection, prior to the excision. An undisclosed number presented 6 months post-procedure with a mean pain score of 2.3/10. It is difficult to attribute the improvement to the anesthetic cocktail, dextrose injection, ischemic compression, the surgical procedure or the combination as there were no comparison groups.
In a series of papers and an abstract,7,38–41 authors outlined an interdisciplinary group program for LPV and impact in terms of pain and functioning. In a 10–12-week program, participants were placed in cohorts, given an information binder, and moved through structured interdisciplinary educational sessions on LPV, sexuality, mindfulness, and CBT. Individual physiotherapy (PT) sessions included instruction on biofeedback, pelvic floor relaxation, and the use of “accommodators.” LPV diagnosis was based on history and examination, including the CST, by a program gynecologist. Validated questionnaires were used to establish pre-participation, immediate post-participation, and longer term (up to 6 months) outcome measures. A subgroup also participated in a qualitative narrative study regarding their experiences and perceived program benefits.
Although limited by participation and reporting bias, the participants in a qualitative study39 (n=19) reported the program increased their knowledge regarding LPV and gave them useful tools and skills. There was a sense of validation and support through the use of a group setting led by specialists knowledgeable in the condition. Participants felt empowered with improved mood/psychological wellbeing. At immediate post-treatment assessment 53.8% reported decreased pain and 41.2% reported no change and the remaining 5% reported an increase.
On quantitative measures (n=132;7 n=31141), Female Sexual Distress Scale (FSDS) decreased immediately post-treatment and pain on the Female Sexual Function Index (FSFI)-pain subscale improved. A substantial number of outcome measures were missing for participants, even though most completed the program. On 2–18-month follow-ups, improvements in sex-related distress, FSFI-pain, sexual satisfaction, and desire were sustained, although pain showed lesser improvement. The authors acknowledge they could not account for other medication use, placebo effect, or the natural course of the disease whereby there is spontaneous improvement in symptoms without intervention in a subset of individuals. These studies provided long-term follow-up, although none accounted for the high numbers of dropouts over time. This is a common phenomenon in longitudinal studies, however if the conclusion is additive benefits over time, participation bias should be accounted for. In other words, persons who saw benefits were more likely to continue to participate in the study as opposed to those who did not, thus inflating the benefits of participation.
In a retrospective case series,42 researcher asked participants of their interdisciplinary program to complete pain and sexual functioning scales 3–7 years post participation to be compared to their recollection of pre-program pain and population controls for function. The program consisted of 12 structured steps, whereby all participants completed steps 1–9 and if appropriate completed steps 10–12 (see Table 1). Seventy participants completed the program and 64 agreed to take part in the study. Following completion of the 9-step program, 42% of participants had also received psychotherapy and 23% had undergone surgery. From their recollection, pain had decreased by 3.6 points on the NRS, however all participants continued to have significantly impaired function based on the FSFI, FSDS, and NRV-SE (Dutch Relationship Questionnaire) compared to the population means. The program had some perceived benefit and was tolerated by patients with 81% of participants reporting a reduction in their pain and 80% were inclined to recommend the program to other participants with PVD. While 11% reported no change in pain and 8% reported an increase, it did not describe which additional steps of the program these participants had completed (ie, vestibulectomy). Demographic characteristics and concomitant therapy use (ie, medications) were also unreported among these participants.
Multimodal/Interdisciplinary Management Followed by Vestibulectomy versus Continued Multimodal/Interdisciplinary Management
There were five cohort studies of patients choosing surgical intervention after multimodal/interdisciplinary management compared with those who continued multimodal/interdisciplinary management.27–29,31–33 Two incorrectly identified their studies as case-control.31,33 There was also a single case report of a 19-year-old female unable to have sexual intercourse who underwent vestibulectomy after incomplete resolution of symptoms with physical therapy and medical management,30 and a case series of posterior vestibulectomy after 10 weeks of physical therapy and cognitive-behavioral sex therapy consultation among 61 patients.34
Mainly, participants choosing vestibulectomy were compared with those who chose continued multimodal/interdisciplinary management: 16 versus 50,29 44 versus 23,31 and 39 versus 27,33 respectively. In the study by Davis et al, 17 of 239 had “surgery”, but the surgical procedure was unspecified.27 The study by Baggish compared 234 participants undergoing vestibulectomy combined with Bartholin-gland excision, called “radical vestibulectomy”, 170 participants undergoing vestibulectomy combined with paraurethral gland excision, called “simple vestibulectomy”, and 98 continuing multimodal/interdisciplinary management.32 Vestibulectomy obstructs the Bartholin gland duct; therefore, gland excision may have been used to prevent cyst formation, a reported postoperative complication. However, there was a high rate of pudendal neuralgia with gland excision, so this was discontinued. Conversely, some patients required reoperation for persistent periurethral pain.32 Tommola et al performed “posterior vestibulectomy.”33 Patients chose surgery after 4–9 months of multimodal/interdisciplinary management.32,33 Patients were diagnosed by physician assessment and/or by long-term symptom duration. Two studies did not report meaningful demographics.31,32 Otherwise, participants were mainly young and nulliparous with about 5 years symptom duration, and baseline NRS pain intensity of 7–9/10.27,29,33 The follow-up period after vestibulectomy ranged from 1 year32 to over 3 years.33 Of note, in Tommola et al, median follow-up time was significantly shorter in the vestibulectomy group (3.9 years) versus in those conservatively managed (6.4 years).33
Baggish was the only investigator to find vestibulectomy clearly superior to conservative management for dyspareunia.32 Vestibulectomy was superior for CST pain in three out of five of the studies29,32,33 and vulvar pain in one.31 One found no difference in vulvar sensitivity.29 CST pain was incongruent with dyspareunia in two studies.29,33 Baggish found a negative CST in those who had radical vestibulectomy and pain-free intercourse, while a third of those conservatively managed who reported “tolerably low” dyspareunia had positive CST with NRS pain of 5–6/10.32 Lambert et al reported that NRS pain decreased from 6.9/10 pre-procedure to 3.7/10 post-procedure, though interviews were conducted retrospectively, 1–7 years after surgery.34 Vestibulectomy was found to be effective in secondary LPV but not primary LPV. Belkin at al. were the only investigators who found vestibulectomy superior to improved sexual function compared with conservative management.31 Gungor Ugurlucan reported pain-free dilator use and improved ability to have intercourse after treatment. She also found that vestibulectomy resulted in increased frequency of intercourse in the treated individual.30 Lambert et al reported that 90% of patients found intercourse possible after surgery.34 In contrast, Davis et al found that, although many other outcomes improved, attempts at intercourse did not.27 Overall, vestibulectomy was not superior to other treatments for quality of life. Davis et al found that the only treatment category that predicted superior outcomes was “surgery”, but only for depressive symptoms. They also found that LPV symptoms tend to improve over time, even without treatment.27
In terms of limitations, duration of follow-up was unspecified by Belkin et al.31 Missing follow-up data were disproportionately higher in the conservatively managed groups in two studies.29,31 One reported that participants estimated their baseline vulvar sensitivity retrospectively at 36-month follow-up.29 Davis et al diagnosed some participants via telephone alone.27 Also, after baseline questionnaires, all participants were offered a 30-min telephone conversation with a clinical sexologist and information on resources in their area, which may have confounded results. Additionally, outcome improvement was reported for each group, but not compared between groups. In all study categories, the outcome assessor was generally not blinded to group assignment. All but two vestibulectomy patients first tried conservative management, also potentially confounding results. Whether participants continued some form of conservative management was generally not reported.
Among adverse events after vestibulectomy, most concerning was pudendal neuralgia related to radical vestibulectomy described by Baggish.32 However, this appeared attributable to excision of the Bartholin gland, which was abandoned in favor of a simple vestibulectomy. Among patients undergoing a typical vestibulectomy, other adverse events were fissures, described in 8% of participants in one study33 and Bartholin gland cysts in 5% described by another.32 Aside from Baggish,32 only one other study reported one patient who had persistent pain at 1 year follow-up, treated with gabapentin.29 Baggish found all vestibulectomy patients complained of dryness post-operatively,32 while Tommola et al found the use of lubricant for coitus to be higher in those conservatively managed.33
Discussion
This scoping review analyzed 27 peer-reviewed, primary study publications of LPV management using interdisciplinary and multimodal approaches. Given the lack of quality head-to-head trials, there is still insufficient evidence to recommend one class of intervention above others or to support interdisciplinary management specific to LPV.
Studies were primarily published in Canada, the United States, and Europe. In general, participants were young, with most studies reporting average ages in the 20s. Most were partnered, highly educated, nulliparous, and had a pain duration of 3–7 years. The study by Spoelstra et al was unique in that two-thirds of participants were parous.42 Of the studies that reported the gender of participants’ partners, the vast majority were in heterosexual relationships. Demographic data around race and ethnicity were largely underreported. The Vancouver-based group's interdisciplinary program papers7,38–41 did include demographics; however, the majority of participants (60–80%) were “Caucasian”/Euro-Canadian. Diagnosis of LPV was often made through a gynecologist’s assessment or using CST. Several studies also limited participation to individuals reporting dyspareunia during the majority of intercourse attempts. Although scores on CST have been shown to correlate with other pain measures such as dyspareunia,43 our review of pharmacologic management for LPV13 demonstrated that improvement in CST did not always coincide with improvement in dyspareunia. Results of this review are consistent with this finding.
Randomized studies included comparisons of pharmacologic treatments for LPV with other treatment modalities, such as physiotherapy and psychotherapy. Broadly speaking, these studies described superior outcomes for non-pharmacologic treatments. However, many employed only one medication as pharmacotherapy and did not control for educational sessions or empathetic attention when accounting for some improvements associated with other treatment modalities. Furthermore, medications used included either topical lidocaine 5% or hydrocortisone 1%, which may not treat LPV as effectively as other pharmacologic therapies. As hydrocortisone is not indicated for vulvodynia medical management, it is possible that treatment benefit stemmed from moisturizing effects, rather than the active ingredient.5
All but one study of structured program-based interdisciplinary management for LPV arose from a single study group.42 These studies are all large observational case series and likely include overlapping participants. The consistent structure and data collection support the program, but efficacy is uncertain due to participation bias, which may inflate improvement in pain among participants. Additionally, one publication states patients are more likely to accept pharmacological treatments over non-pharmacological ones.39 The magnitude of improvement in participants may be because patients who expected pharmacological treatment chose not to participate and/or those that agreed to participate were more open to improvement with non-pharmacological treatments. Participants were also excluded if deemed “hostile” or “anxious.” Although the numbers at follow-up were significantly less, and the researchers do not account for the dropouts, it is encouraging that participants report long-lasting and perhaps continued improvements at 6-months follow-up. However, it is unclear whether participants continued receiving treatment during the follow-up period. A significant proportion of potential participants declined assessment due to scheduling conflicts and inability to commute.7 This limits generalizability. There is, however, promising research in virtual delivery of vulvar pain programs making programs, if effective, more accessible.44,45
One study randomized participants to traditional versus non-traditional acupuncture.26 While the small sample size, use of topical lidocaine and lack of a true placebo group precluded the authors from drawing conclusions regarding treatment effectiveness, there were valuable lessons regarding study design. The addition of topical lidocaine 5% contributed to drop-outs and may have confounded effects of acupuncture. Also, a placebo arm for acupuncture is difficult to achieve, though authors compared traditional and non-traditional techniques, postulating that any penetration with acupuncture needles would affect endogenous opioids. Indeed, 24-week pain outcomes were superior with non-traditional acupuncture. Another study comparing acupuncture with other treatments found that while all other groups, including those with no treatment, had improvement in pain, acupuncture did not.27 However, only 6 of the 239 participants underwent this therapy. At present, there is a lack of well-powered studies of acupuncture for LPV.
A number of studies evaluated outcomes of vestibulectomy compared to conservative management. One cohort study had over four hundred vestibulectomy patients with a follow-up duration of 1 year.32 The longest duration of follow-up was of 39 vestibulectomy patients followed for approximately 6 years,33 exceeding follow-up durations prior to 2010.8 Among all studies, all but two patients undergoing vestibulectomy had prior multimodal treatment, and some also continued afterwards. Some vestibulectomy studies demonstrated superior CST results; however, improvements in dyspareunia were most often comparable to conservative management. Two studies followed similar procedures for both conservative and surgical management with 35 combined vestibulectomy patients and follow-up duration of 3 to 6 years.29,33 Unfortunately, missing data make it difficult to draw conclusions from one study.29 While Tommola et al found less severe posterior vestibular pain on CST in the posterior vestibulectomy group, this did not translate into clinical outcomes.33 Equal reductions in dyspareunia and treatment response were seen between groups. The exception to this pattern was the cohort study by Baggish,32 which showed dramatically superior success rates, defined as absent or minimal pain with intercourse, for vestibulectomy compared to conservative management. However, the only patients included were those with one-year follow-up data and no information was provided on dropouts, a potential source of bias. There was also no systematic outcome evaluation using validated measures, and the assessor was not blinded to group assignment.
Vestibulectomy studies had generally reassuring low complication rates. One study32 was the outlier, with a 13% rate of pudendal neuralgia. However, this was clearly associated with the degree of dissection required for Bartholin’s gland excision and was abandoned for that reason. Once this was omitted, there were no further reports of pudendal neuralgia.
Constructing adequate comparator groups was a challenge reported in several studies. Blinding is difficult with vestibulectomy, acupuncture, psychologically oriented interventions, and structured interdisciplinary programs due to lack of realistic “sham” procedures. Therefore, at a minimum, the assessor of subjective outcomes should be blinded to group assignment, although this too may be difficult for vestibulectomy due to possible evidence of surgical scar. In addition, only one study27 included a no-treatment arm to analyze possible spontaneous improvements to LPV with time. However, in this study, researchers did not compare treatments to each other, but rather analyzed which treatments yielded desired outcomes.
Heterogeneity and inaccuracy in outcome measures makes comparisons challenging and efforts should be made to standardize this in the literature. For example, Numeric Rating Scale (NRS) for dyspareunia was often used, though it was often incorrectly labeled as Visual Analogue Scales (VAS). VAS, a validated measure through which patients indicate pain severity,43 uses a 100 mm, unmarked, continuous line. NRS, which has not received the same validation as VAS, asks patients to choose an integer from 0 to 10 indicating pain severity. Other outcome measures included questionnaires such as the FSFI, FSDS, and the McGill pain questionnaire, and a wide array of measures were used to assess quality of life, sexual functioning, patient satisfaction, and impression of change. Several studies comparing psychological interventions to other treatments used outcomes such as catastrophizing, self-efficacy, anxiety, and sexual communication. Although LPV pain improvement may yield psychosocial benefits, the choice of these measures may have skewed the results in favor of psychological interventions. In several studies of interdisciplinary programs, authors noted that provider attention and educational components of treatment may have influenced participant satisfaction. Participants identified education and validation of their complaints as legitimate positively impacted psychological wellbeing, consistent with other studies of vulvar pain.39,46,47
While many studies showed improvements in psychological wellbeing and decreased pain, it was often emphasized that participants did not engage or attempt intercourse more often, which highlights the problematic phallocentricity that underlies many studies of vulvar pain. The definition of LPV does not include dyspareunia and, while this is a common symptom, focusing on dyspareunia propagates penetrative intercourse as the “gold standard”, undermining the validity of other forms of sexual activity. Additionally, it excludes patients for whom sexual activity holds lower value over other measures of wellbeing, such as comfort with clothing or menstrual products. Other studies discuss in more detail phallocentricity and restrictive cultural norms of sexual activity.47–49
Our findings support head-to-head studies of vestibulectomy as a first-line treatment compared to other active treatments. Reassuringly low complication rates, including studies, which comprehensively report complications,33 coupled with long-term follow-up, support vestibulectomy as a potential first-line treatment for LPV. Traditionally, vestibulectomy has been reserved as a last-line treatment, despite evidence of efficacy.4,5 It is worth noting that more “conservative” treatments are not without adverse events such as pain and medication side effects. Improvement may require long-term use prior to benefit. There is also a substantive population of patients for whom vestibulectomy may be the preferred or only treatment option as physiotherapy or interdisciplinary programs may not be feasible due to time constraints, availability and financial considerations. With appropriate informed consent regarding what is known regarding complication rates, and uncertainty of effectiveness in a population that has not already failed other management options, patients may indeed choose to participate in randomized trials of vestibulectomy for potentially equivalent treatment effectiveness. Researchers should review the literature on demographic characteristics associated with favorable outcomes of vestibulectomy in selecting appropriate candidates for whom this may be offered as a first-line treatment.
There is concern regarding adverse events of vestibulectomy as there is a general lack of consistency, transparency and confidence regarding comprehensive assessment and reporting. Future reporting of adverse events should include lack of improvement, worsening of pain (detailing severity and duration), incidence of postoperative Bartholin’s gland or inclusion cysts, wound dehiscence/infection, readmission for postoperative pain management, and vaginal/introital dryness. In addition, researchers should report on perceived etiology and outcomes of complication management. By establishing more transparent reporting practices, vestibulectomy can be better evaluated both in terms of its effectiveness and side effect profile.
Future research should compare treatments from various modalities using well-designed randomized studies. Attention should be paid to using standard-of-care treatments from each therapeutic arm and non-treatment arms where appropriate to evaluate effects of the natural course of LPV. Authors should use validated outcome measures such as VAS and tools such as the Vulvovaginal Symptoms Questionnaire to measure psychosocial outcomes associated with LPV.50 Research should also include more diverse participants from various races, ethnicities, age ranges, sexual orientations, and gender identities to enhance generalizability of findings and improve recommendation quality for clinical practice. Similarly, expanding educational programming across the gender/sexuality spectrum will better mirror the diverse attitudes and practices of those living with LPV.
Strengths and Limitations
This scoping review is a thorough description of the recent literature around LPV management relating specifically to interventions across modalities and interdisciplinary interventions. This paper details the breadth of current research in the field. Given our search design was a scoping review rather than a systematic review or meta-analysis, our aim was not to address one specific clinical question nor to direct clinical practice.51 However, we have highlighted several outstanding questions and future opportunities for researchers evaluating multimodal/interdisciplinary management strategies for LPV.
As our scoping review was limited to contemporary management of LPV, we excluded studies published prior to 2010, though these continue to carry weight in clinical practice. These are outlined in several exceptional articles including a review by Andrews.8 We also recognize that this paper only details interventions that are compared across treatment modalities or that integrate an interdisciplinary approach to management. Our original goal was to include all peer-reviewed publications on treatment effectiveness. However, given the breadth of the literature, we opted to publish several papers based on treatment category. This paper focuses on multimodal and interdisciplinary comparisons, while our other manuscripts address pharmacological, physical, and psychological interventions. As was the case in our review of pharmacotherapy,13 interventions that implied underlying pathology of vulvar pain were excluded, which is consistent with the clinical definition of vulvodynia.2
Conclusions
This scoping review identified a lack of convincing head-to-head trials of different treatment modalities for LPV as well as a lack of well-designed studies of multimodal interventions. Shortcomings highlighted by researchers include a) suboptimal pharmacologic choices in head-to-head trials; b) an absence of studies rigorously comparing multimodal interventions, vestibulectomy, and acupuncture with other established treatments for LPV; c) possible participation bias related to engagement with intensive treatment protocols; and d) the use of unvalidated or inappropriate measures to gauge treatment efficacy. We also noted that interdisciplinary program studies had e) significant participation and recall bias. We recommend that future studies include appropriate comparator groups or involve blinded assessors, especially when creating a sham or placebo is not feasible for a given intervention. As such, head-to-head trials may represent the most promising avenue for comparing treatment options. Outcome measures should include those which are validated and patient-oriented, that is, those which appropriately mirror LPV patients’ concerns and goals.
Regarding participant selection, studies of LPV continue to underreport demographic data and, when reported, appear to include a disproportionate number of white, highly educated, partnered, heterosexual women. Researchers are encouraged to diversify their participant sample to improve generalizability of their findings.
This is only one portion of a larger scoping review analyzing an array of LPV treatments. The breadth and variability of management strategies for LPV expose the need for GRADE-structured evidence-based consensus guidelines and recommendations for appropriate outcome measures and reporting of adverse events.
Acknowledgments
We gratefully acknowledge the contributions of Katherine Iannuzzelli, a medical student at Rush Medical College in Chicago, IL, US, and Liam Jackman, a medical student at University of Toronto, Toronto, ON, Canada, who contributed to the early stages of this project.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287–333. doi:10.1016/j.ejpain.2005.06.009
2. Bornstein J, Goldstein AT, Stockdale CK, et al. ISSVD, ISSWSH and IPPS consensus terminology and classification of persistent vulvar pain and vulvodynia. Obstet Gynecol. 2016;127(4):745–751. doi:10.1097/AOG.0000000000001359
3. Harlow BL, Kunitz CG, Nguyen RH, Rydell SA, Turner RM, MacLehose RF. Prevalence of symptoms consistent with a diagnosis of vulvodynia: population-based estimates from 2 geographic regions. Am J Obstet Gynecol. 2014;210(1):
4. Haefner HK, Collins ME, Davis GD, et al. The vulvodynia guideline. J Low Genit Tract Dis. 2005;9(1):40–51. doi:10.1097/00128360-200501000-00009
5. Stockdale CK, Lawson HW. Vulvodynia guideline update. J Low Genit Tract Dis. 2014;18(2):93–100. doi:10.1097/LGT.0000000000000021
6. Lua LL, Hollette Y, Parm P, Allenback G, Dandolu V. Current practice patterns for management of vulvodynia in the United States. Arch Gynecol Obstet. 2017;295(3):669–674. doi:10.1007/s00404-016-4272-x
7. Brotto LA, Yong P, Smith KB, Sadownik LA. Impact of a multidisciplinary vulvodynia program on sexual functioning and dyspareunia. J Sex Med. 2015;12(1):238–247. doi:10.1111/jsm.12718
8. Andrews JC. Vulvodynia interventions-systematic review and evidence grading. Obstet Gynecol Surv. 2011;66(5):299–315. doi:10.1097/OGX.0b013e3182277fb7
9. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi:10.1080/1364557032000119616
10. Choi BC, Pak AW. Multidisciplinarity, interdisciplinarity and transdisciplinarity in health research, services, education and policy: 1. Definitions, objectives, and evidence of effectiveness. Clin Invest Med. 2006;29(6):351–364.
11. Burrows LJ, Goldstein AT. The treatment of vestibulodynia with topical estradiol and testosterone. Sex Med. 2013;1(1):30–33. doi:10.1002/sm2.4
12. Langlais EL, Lefebvre J, Maheux-Lacroix S, Bujold E, Fortier M, Bouchard C. Treatment of secondary vestibulodynia with conjugated estrogen cream: a pilot, double-blind, randomized placebo-controlled trial. J Obstet Gynaecol Can. 2017;39(6):453–458. doi:10.1016/j.jogc.2016.10.011
13. Bajzak K, Rains A, Bishop L, et al. Pharmacological treatments for localized provoked vulvodynia: a scoping review. Int J Sex Health. 2023;35(3):427–443. doi:10.1080/19317611.2023.2222114
14. Danielsen KG, Dahl-Michelsen T, Håkonsen E, Haugstad GK. Recovering from provoked vestibulodynia: experiences from encounters with somatocognitive therapy. Physiother Theory Pract. 2019;35(3):219–228. doi:10.1080/09593985.2018.1442540
15. Haugstad GK, Wojniusz S, Kirschner R, Kirste U, Lilleheie I, Haugstad TS. Somatocognitive therapy of women with provoked vulvodynia: a pilot study. Scand J Pain. 2019;19(4):725–732. doi:10.1515/sjpain-2019-0011
16. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2020;37:n71. doi:10.1136/bmj.n71
17. Morin M, Dumoulin C, Bergeron S, et al. Randomized controlled trial of multimodal physiotherapy treatment compared to overnight topical lidocaine in women suffering from provoked vestibulodynia. Int Urogynecol J. 2015;26(Suppl 1):S23–S174.
18. Morin M, Dumoulin C, Bergeron S, et al. Randomized clinical trial of multimodal physiotherapy treatment compared to overnight lidocaine ointment in women with provoked vestibulodynia: design and methods. Contemp Clin Trials. 2016;46:52–59. doi:10.1016/j.cct.2015.11.013
19. Morin M, Dumoulin C, Bergeron S, et al. Multimodal physical therapy versus topical lidocaine for provoked vestibulodynia: a multicenter, randomized trial. Am J Obstet Gynecol. 2021;224(2):
20. Bergeron S, Vaillancourt-Morel MP, Corsini-Munt S, et al. Cognitive-behavioral couple therapy versus lidocaine for provoked vestibulodynia: a randomized clinical trial. J Consult Clin Psychol. 2021;89(4):316–326. doi:10.1037/ccp0000631
21. Rancourt KM, Bergeron S, Vaillancourt-Morel MP, Lee-Baggley D, Delisle I, Rosen NO. Sexual communication mediates cognitive-behavioral couple therapy outcomes: a randomized clinical trial for provoked vestibulodynia. J Fam Psychol. 2022;36(7):1073–1083. doi:10.1037/fam0000968
22. Rancourt K. Sexual communication in couples coping with provoked vestibulodynia: associations with biopsychosocial outcomes and trajectories of change with intervention [dissertation]. Halifax, NS: Dalhousie University; 2017.
23. Bergeron S, Khalifé S, Dupuis MJ, McDuff P. A randomized clinical trial comparing group cognitive- behavioral therapy and a topical steroid for women with dyspareunia. J Consult Clin Psychol. 2016;84(3):259–268. doi:10.1037/ccp0000072
24. Desrochers G, Bergeron S, Khalifé S, Dupuis MJ, Jodoin M. Provoked vestibulodynia: psychological predictors of topical and cognitive-behavioral treatment outcome. Behav Res Ther. 2010;48(2):106–115. doi:10.1016/j.brat.2009.09.014
25. Goldfinger CA. A randomized comparison of individual cognitive-behavioural therapy and pelvic floor rehabilitation in the treatment of provoked vestibulodynia [dissertation]. Kingston, ON: Queen’s University; 2013.
26. Hullender Rubin LE, Mist SD, Schnyer RN, Chao MT, Leclair CM. Acupuncture augmentation of lidocaine for provoked, localized vulvodynia: a feasibility and acceptability study. J Low Genit Tract Dis. 2019;23(4):279–286. doi:10.1097/LGT.0000000000000489
27. Davis SN, Bergeron S, Binik YM, Lambert B. Women with provoked vestibulodynia experience clinically significant reductions in pain regardless of treatment: results from a 2-year follow-up study. J Sex Med. 2013;10(12):3080–3087. doi:10.1111/jsm.12309
28. Aalto AP, Huhtala H, Mäenpää J, Staff S. Quality of life after surgery vs. conservative treatment for local provoked vulvodynia. J Low Genit Tract Dis. 2017;21(4):S209–214. doi:10.1097/LGT.0000000000000318
29. Aalto AP, Huhtala H, Mäenpää J, Staff S. Combination of treatments with or without surgery in localized provoked vulvodynia: outcomes after three years of follow-up. Biores Open Access. 2019;8(1):25–31. doi:10.1089/biores.2018.0044
30. Gungor Ugurlucan F. Surgical treatment of vaginismus secondary to vulvar vestibulitis syndrome. J Sex Med. 2016;13(5):S187. doi:10.1016/j.jsxm.2016.03.250
31. Belkin Z, Jutrzonka S, Burrow L, Christopher K, Goldstein A. Vulvar vestibulectomy for provoked vestibulectomy-a retrospective case-control study. J Sex Med. 2014;11(suppl 4):2764–2771. doi:10.1111/jsm.12668
32. Baggish MS. Diagnosis and management of vulvar vestibulitis syndrome in 559 women (1991–2011). J Gynecol Surg. 2012;28(2):75–82. doi:10.1089/gyn.2012.0018
33. Tommola P, Unkila-Kallio L, Paavonen J. Long-term well-being after surgical or conservative treatment of severe vulvar vestibulitis. Acta Obstet Gynecol Scand. 2012;91(9):1086–1093. doi:10.1111/j.1600-0412.2012.01466.x
34. Lambert B, Bergeron S, Desrosiers M, Lepage Y. Introital primary and secondary dyspareunia: multimodal clinical and surgical control. Sexologies. 2012;21(1):9–12. doi:10.1016/j.sexol.2011.10.001
35. Close A, Culha MG, Albert V, Valancogne G. Exclusive manual perineal rehabilitation with lidocaine 2% gel in the treatment of provoked vestibulodynia: results from a single-arm interventional study. Int J Impot Res. 2023;35(2):157–163. doi:10.1038/s41443-022-00537-9
36. Ghizzani A, Toto G, Luisi S. Behavioral sex therapy and medications associated in the treatment of provoked vulvodynia: efficacy on pain and sexuality in three illustrative cases. Minerva Obstet Gynecol. 2022;74(3):302–307. doi:10.23736/S2724-606X.22.04894-1
37. Yee A, Uloko M, Mueller J, Goldstein I. Perineural 5% dextrose injection treatment and central core excision of the 12:00 vestibule as adjunctive therapies to complete vestibulectomy in select patients with neuroproliferative vestibulodynia. J Sex Med. 2022;19(8):S42–S43. doi:10.1016/j.jsxm.2022.05.137
38. Brotto LA. Efficacy of the multidisciplinary vulvodynia program for treating women with provoked vestibulodynia. Pain Res Manag. 2012;17(3):200.
39. Sadownik LA, Seal BN, Brotto LA. Provoked vestibulodynia-a qualitative exploration of women’s experiences. BC Med J. 2012;54:22–28.
40. Yong PJ, Sadownik L, Brotto LA. Concurrent deep-superficial dyspareunia: prevalence, associations, and outcomes in a multidisciplinary vulvodynia program. J Sex Med. 2015;12(1):219–227. doi:10.1111/jsm.12729
41. Smith KB, Sadownik LA, Dargie E, Albert AYK, Brotto LA. Multidisciplinary treatment for provoked vestibulodynia: treatment trajectories, predictors, and moderators of sexual distress and pain. Clin J Pain. 2019;35(4):335–344. doi:10.1097/AJP.0000000000000682
42. Spoelstra SK, Dijkstra JR, van Driel MF, Weijmar Schultz WC. Long-term results of an individualized, multifaceted, and multidisciplinary therapeutic approach to provoked vestibulodynia. J Sex Med. 2011;8(2):489–496. doi:10.1111/j.1743-6109.2010.01941.x
43. Foster DC, Beth Kotok M, Huang LS, et al. The tampon test for vulvodynia treatment outcomes research: reliability, construct validity, and responsiveness. Obstet Gynecol. 2009;113(4):825–832. doi:10.1097/AOG.0b013e31819bda7c
44. Bullemor-Day P, Coope N, Murrill J, Van Der Walt H, Ahmed N. Treating sexual dysfunction during the pandemic: can virtual psychosexual group interventions for women experiencing painful sex be effective? HIV Med. 2021;22(suppl 2):109–110.
45. Hess Engström A, Bohm-Starke N, Kullinger M, et al. Internet-based treatment for vulvodynia(EMBLAA) - randomized controlled study. J Sex Med. 2022;19(2):319–330. doi:10.1016/j.jsxm.2021.11.019
46. LePage K, Selk A. What do patients want? A needs assessment of vulvodynia patients attending a vulvar diseases clinic. Sex Med. 2016;4(4):e242–e248. doi:10.1016/j.esxm.2016.06.003
47. Webber V, Miller ME, Gustafson DL, Bajzak K. Vulvodynia viewed from a disease prevention framework: insights from patient perspectives. Sex Med. 2020;8(4):757–766. doi:10.1016/j.esxm.2020.07.001
48. Groven KS, Raheim M, Hakonsen E, Haugstad GK. “Will I ever be a true woman?” An exploration of the experiences of women with vestibulodynia. Health Care Women Int. 2016;37(8):818–835. doi:10.1080/07399332.2015.1103739
49. Shallcross R, Dickson JM, Nunns D, Mackenzie C, Kiemle G. Women’s subjective experiences of living with vulvodynia: a systematic review and meta-ethnography. Arch Sex Behav. 2018;47(3):577–595. doi:10.1007/s10508-017-1026-1
50. Erekson EA, Yip SO, Wedderburn TS, et al. The vulvovaginal symptoms questionnaire: a questionnaire for measuring vulvovaginal symptoms in postmenopausal women. Menopause. 2013;20(9):973–979. doi:10.1097/GME.0b013e318282600b
51. Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi:10.1186/s12874-018-0611-x
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
