Back to Journals » Patient Preference and Adherence » Volume 18
Medication-Free Treatment in Mental Health Care How Does It Differ from Traditional Treatment?
Authors Standal K , Solbakken OA, Rugkåsa J , Halvorsen MS , Abbass A, Wirsching C, Brakstad IE, Heiervang KS
Received 15 August 2023
Accepted for publication 18 December 2023
Published 3 February 2024 Volume 2024:18 Pages 315—335
DOI https://doi.org/10.2147/PPA.S435610
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Kari Standal,1 Ole Andre Solbakken,2 Jorun Rugkåsa,3– 5 Margrethe Seeger Halvorsen,2 Allan Abbass,6 Christopher Wirsching,2 Ingrid Engeseth Brakstad,2 Kristin S Heiervang7,8
1District Psychiatric Center Nedre Romerike, Akershus University Hospital, Lørenskog, Norway; 2Department of Psychology, University of Oslo, Oslo, Norway; 3Health Services Research Unit, Akershus University Hospital, Lørenskog, Norway; 4Department of Mental Health, Oslo Metropolitan University Oslo, Norway; 5Centre for Care Research, University of Southeastern Norway, Porsgrunn, Norway; 6Faculty of Medicine, Dalhousie University, Nova Scotia, Canada; 7Research and Development Department, Division of Mental Health Services, Akershus University Hospital, Lørenskog, Norway; 8Centre of Medical Ethics, Faculty of Medicine, University of Oslo, Oslo, Norway
Correspondence: Kari Standal, District Psychiatric Center Nedre Romerike, Akershus University Hospital, Akershus universitetssykehus HF, DPS Nedre Romerike, Postboks 1000, Lørenskog, 1478, Norway, Tel +47 679 60 155, Email [email protected]
Background: Norwegian authorities have implemented treatment units devoted to medication-free mental health treatment nationwide to improve people’s freedom of choice. This article examines how medication-free treatment differs from treatment as usual across central dimensions.
Methods: The design was mixed methods including questionnaire data on patients from a medication-free unit and two comparison units (n 59 + 124), as well as interviews with patients (n 5) and staff (n 8) in the medication-free unit.
Results: Medication-free treatment involved less reliance on medications and more extensive psychosocial treatment that involved a culture of openness, expression of feelings, and focus on individual responsibility and intensive work. The overall extent of patient influence for medication-free treatment compared with standard treatment was not substantially different to standard treatment but varied on different themes. Patients in medication-free treatment had greater freedom to reduce or not use medication. Medication-free treatment was experienced as more demanding. For patients, this could be connected to a stronger sense of purpose and was experienced as helpful but could also be experienced as a type of pressure and lack of understanding. Patients in medication-free treatment reported greater satisfaction with the treatment, which may be linked to a richer psychosocial treatment package that focuses on patient participation and freedom from pressure to use medication.
Conclusion: The findings provide insights into how a medication-free treatment service might work and demonstrate its worth as a viable alternative for people who are not comfortable with the current medication focus of mental health care. Patients react differently to increased demands and clinicians should be reflexive of the dimensions of individualism–relationism in medication-free treatment services. This knowledge can be used to further develop and improve both medication-free treatment and standard treatment regarding shared decision-making.
Trial Registration: This study was registered with ClinicalTrials.gov (Identifier NCT03499080) on 17 April 2018.
Keywords: medication-free, mental health care, psychotropics, choice
Introduction
Since 2015, all Regional Health Trusts in Norway are required to provide medication-free treatment to people with mental disorders within the structure of dedicated units. This has resulted from an instruction by the Ministry of Health,1 which is unprecedented worldwide.
The official aim of medication-free units is that, as far as clinically justifiable, patients should have the opportunity to choose whether they want medication as part of their treatment.1 The policy emerged partly from the lobbying by a coalition of user organizations that viewed medication-free treatment as a means to avoid coercion, pressure or persuasion related to medication.2 Local protocols of the health regions have clarified that patients treated in medication-free units may use psychotropics if they wish.3,4
In this article, medication-free treatment refers to services developed in response to the governmental decision mentioned above. Medication-free treatment is interpreted to mean that the service is free from medication pressure and involuntary treatment with medication, rather than free from all use of psychotropic medication.
Medication has been a central part of treatment for severe mental disorders in Western medicine since the 1950s,5 but only about half of patients with a severe psychiatric disorder adhere to their medication regimen.6 The World Health Organization (WHO) has recently criticized mental health care internationally for being too restricted to a biomedical model of illness that places psychotropic drugs at the center of treatment.7 Referring to the United Nations Convention on the Rights of Persons with Disabilities (CRPD),8 the WHO has called for eliminating involuntary admission and treatment.7
Historically, other initiatives for the treatment of severe mental disorders have explicitly prioritized the psychosocial component over medication. Some of the most well known are Chestnut Lodge (1920–2000),9 Kastanjebakken (1977–2000),10 Soteria (1969–ff),11,12 and Open Dialogue (1980s–ff).13 Common elements are the emphasis on relationships,10,11,14–16 flexibility and adaptation, a supportive environment, and finding meaning in the person’s experiences.11,14–16 These treatments vary in therapeutic intensity.11,14,16,17 Although none of these treatment ban medications, they typically use them more sparingly than in traditional health care and believe that other elements are more central to long-term improvement.9–12,15,16
By 2018, medication-free treatment was offered at 25 locations in Norway.18 The services are not uniform, but the most common characteristics are that treatment is provided within inpatient open wards, patients with a severe mental disorder are prioritized, and the treatment is influenced by a recovery-oriented tradition.18,19
The recovery approach is characterized by a focus on connectedness, hope, identity, meaning of life, and empowerment (CHIME).19 The recovery tradition focuses on personal recovery: that is, a recovery process that is defined and experienced individually as opposed to clinical recovery that is located within an illness frame of understanding. This approach also highlights that clinical recovery is heterogeneous and does not follow a set course of illness. The recovery tradition emphasizes that treatment services should be based on the views of individual patients rather than on professional priorities.20 Although medications are recognized as important treatment options within the recovery approach,21 this approach has criticized traditional services for handling the medication issue dogmatically.20
Earlier investigations of medication-free treatment services in Norway indicate that these services offer more psychosocial treatment22 and require more staff resources23,24 compared with standard treatment. Staff experience an increased focus on client participation23 or shared decision-making22 and using less medication, and an increased focus on patients’ responsibility for their own health, group therapy, and processes to facilitate recovery.23 Staff sometimes find it challenging to balance a patient’s needs with treatment guidelines, the legal framework, and available resources.24 Patient interviews reveal experiences of increased responsibility and freedom, a less pathologizing language, being seen as humans as opposed to being labelled, greater unity between users and staff, and improved involvement of family, friends and their network.25
There is an ongoing debate about whether such units provide something new and are needed.26,27 To our knowledge, no articles in peer-reviewed journals have reported a broad investigation into the characteristics of medication-free units compared with traditional treatment. The characteristics of current medication-free treatment regimens and differences from those of traditional services should be explored in greater detail.
The aim of the present study was to investigate the characteristics of medication-free treatment as compared with traditional approaches. Using quantitative data, we compared the provision and experience of treatment in a medication-free unit with that in treatment-as-usual units at the same level of care. We used qualitative interviews with patients and staff at the medication-free unit to explore their views and experiences of how the medication-free unit compared with other relevant experiences.
Materials and Methods
Setting
The setting for this study was one medication-free unit and two standard care (treatment as usual or TAU) units under a general university hospital in the metropolitan Oslo area in Norway. The hospital has a catchment population of 500,000 and contains both urban and rural communities. The medication-free unit is representative of such services for most common characteristics.18 The unit officially opened as a medication-free unit on 1 March 2017 and had been in operation for about 1 year at the start of data collection. The characteristics of the units are shown in Table 1.
 |
Table 1 Characteristics of the Included Treatment Units |
Design
The design was for a preplanned parallel multi-sample mixed methods,32 observational and pragmatic study within a naturalistic treatment setting. The point of integration between the quantitative and qualitative methods was mainly in the analysis stage. We compared the medication-free unit with TAU using validated measures and questionnaires to ascertain the extent of psychosocial treatment, treatment with medication, and formal assessments; measures of patients’ experiences of treatment in terms of their satisfaction, shared decision-making, alliance, support for personal recovery, help with medication and respect for their not wanting to use medication. We also analyzed the results of interviews with staff and patients about the medication-free unit in which participants compared their experiences of the unit with other relevant work/treatment experiences. For staff, this focused on the ward before becoming a medication-free unit, and for patients, this mostly related to other treatment experiences.
The purpose of using multi-sample mixed methods was to obtain a more nuanced perspective of the relevant phenomena. A parallel design was deemed feasible and adequate. The main reason mixed methods was deemed suitable in this study was the complexity of the phenomenon of study. The phenomenon of medication-free treatment units has unclear boundaries toward treatment as usual. The explorative potential of the qualitative approach, as well as having several approaches illuminating the same questions, seemed useful for capturing this new phenomenon. It also seemed a suitable way to strengthen our inferences. We reckoned that integrating quantitative and qualitative approaches would provide a test of corroboration and complementarity. Moreover, the design enables both comparison with treatment as usual, for which the standardized aspects of the quantitative approach are well suited, and exploration of unique aspects of this setting.
Criteria for Inclusion and Exclusion
The inclusion criteria for patients were intended to capture the widest possible range of people on standard treatment stays that were comparable across units. Eligible patients were patients on a planned stay during the recruitment period who were deemed capable of being interviewed and/or completing forms in Norwegian and who consented to participate. The exclusion criteria were emergency stays and self-referral admissions, which are shorter stays that do not follow the standard treatment program, or inability to participate (being unable to be interviewed or complete forms in Norwegian).
The inclusion criteria for staff were intended to capture people with experience both before and after the introduction of medication-free treatment who had much patient involvement and were possible to anonymize. Eligible staff were milieu personnel who had been employed for ≥1 a year at the time of inclusion and who were working full time and mainly during the day.
Sampling Procedures
The recruitment periods for the questionnaires were from May 2018 to April 2020 and September 2020 to the end of March 2021, with a break in between because of the Covid-19 pandemic. Only the neighboring TAU unit continued recruiting patients after the break. Data for all patients were collected during their treatment stay. Interviews were conducted from January to March 2018. Staff were purposively sampled through leaders at the unit and were informed and asked for consent by the interviewer. Patients were recruited through therapists who distributed information and consent forms at the beginning of each admission.
Regarding the questionnaire sample, power calculations were made for the primary outcome variable (OQ-45–2) of the larger study described in Heiervang,33 yielding a required sample size of 224. For this article, we did posthoc sensitivity calculations with the program G*Power34 on the nonsignificant results indicating that we had adequate power to detect about medium sized differences (Supplement, Table S1–3). All nonsignificant results were below medium in size. Hence there may be below medium sized differences that could have been detected in a larger sample.
We had a goal of recruiting about eight participants for each interview sample, as this was deemed a suitable size for forming part of a mixed methods design.
Data Collection
We piloted the study routines in which we also gathered feedback from participants regarding questionnaires and interview guides. Questionnaires and clinical measures were completed by patients or their clinicians during the treatment period. One author (IEB) and another psychology student performed semi-structured individual face-to-face interviews with staff and patients, respectively. The interviews lasted 50–60 minutes and were audio-recorded.
Overview of the Data
An overview of the data is presented in Table 2.
 |
Table 2 Overview of the Data |
Questionnaires
Questions were completed by patients or their clinician, as indicated in Table 2. Medications were grouped according to the Norwegian Medication Handbook.35 Questions on treatment received are adapted to the present context from forms developed by a certified research institute.36,37 Otherwise, questions are derived from a larger study on a similar patient group with minor modifications. Translated versions of questionnaires can be found in the Supplement, Figure S1–10.
Standardized Clinical Measures
Table 3 shows the standardized clinical measures used in this study.
 |
Table 3 Measures of Treatment Experiences Obtained by Patient Report |
 |
Table 4 Sample Characteristcs |
 |
Table 5 Psychosocial Treatment Received, Medication-Free Treatment versus TAU |
 |
Table 6 Treatment with Psychotropics and Assessment for the Medication-Free Treatment versus TAU |
 |
Table 7 Patient-Rated Experiences of Admission to Medication-Free Treatment versus TAU |
 |
Table 8 I Have Been Respected for My Wish Not to Use Medication (MedSupport Question 7) Details |
Interview Guides
An interview guide for patient interviews was developed in collaboration between a student and authors KS, MSH, and KSH, and was based on the literature and a previous study of medication-free services.44 Topics included patients’ understanding and expectations of medication-free treatment and attitudes about this treatment approach, as well as whether, and why, medication-free treatment was important for them, how the treatment compared with other treatment experiences, and whether, and how, they experienced shared decision-making. An interview guide for staff interviews was developed in collaboration between KS, IEB, and KSH. Topics included how staff participants view, understand, and experience the medication-free mandate compared with more traditional approaches. Translated versions can be found in the Supplement.
Analyses
Analyses were mainly parallel track analyses, meaning that quantitative and qualitative analyses were conducted separately first, and findings were then integrated. However, the different strands were allowed to talk to each other, and some crossover track analysis occurred in the integration phase.
Quantitative Analyses
Cronbach’s alpha for internal consistency reliability for all multi-item measures was >0.80 (details are shown in the Supplement, Table S4). Numerical questionnaire data were analyzed using IBM SPSS Statistics (version 26) and are reported as frequency and valid per cent (valid %) or mean (M) and standard deviation (SD) as appropriate. Psychotropic drugs were grouped according to the Norwegian Medication Handbook (Norsk legemiddelhåndbok).35 Differences between groups were identified using independent sample t-tests (sample characteristics) and one way between groups analysis of variance (ANOVA) (treatment characteristics) for continuous variables and chi-squared tests for categorical variables.
Although our interest was in differences between regimens, we also performed ward level analyses (Supplement, Tables S5–8) to more robustly assess the degree to which medication-free treatment stands out. We expected there could be spillover effects between the neighboring wards. Sensitivity analysis without outliers was performed to assess the impact of outliers.
Qualitative Analyses
The qualitative interview data were analyzed using a combination of thematic analysis45 and systematic text condensation.46 Thematic analysis involves flexible stepwise analysis wherein, after familiarization, the data are first coded in terms of basic meaning units and these codes are then sorted into broader themes.45 Audio files were transcribed verbatim and coded and sorted using the program NVivo 14.23.1.(38). Initially, KS reviewed the transcripts using predominantly inductive coding of the interviews, and the coding was grouped according to the research questions of the overarching project.33 Given that the medication-free mandate is not sharply delineated from TAU, all distinguishing features of this unit were included in the findings. Relationships with the mandate were discussed in the discussion part. The codes were then sorted into broader themes separately for patients and staff data. The data in each theme were then condensed,46 and these condensates from the patients and staff were combined into higher-level themes through an iterative process involving KSH, JR, MSH, IEB, and CW. Finally, we revisited the transcripts to check whether the final themes resonated with the data.
Integration of Results
The qualitative and quantitative data were integrated with the help of joint displays, which are regarded as a way to depict, juxtapose, and analyze data.32,47 Joint displays compare qualitative and quantitative data and can be used to provide integrative statements.32 Rows were used for the overall issues addressed or identified in the data, and columns were used for the quantitative and qualitative results. We investigated convergence, divergence and complementarity in the results and used these analyses to develop integrative statements across all results. In this process, the qualitative data were revisited to determine if they could further illuminate quantitative findings, allowing for some crossover track analysis. For example, the finding of higher patient satisfaction in medication-free treatment guided an investigation in the qualitative material of which changes were positively regarded by the patients.
Results
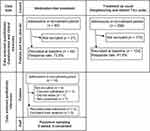
Participant Flow Chart
Figure 1 shows participant flow
Questionnaire Sample
Sample characteristics are summarized and compared between regimens in Table 4.
According to mental health measures, participants in both conditions scored above clinical cut off on OQ-45–2,48 in the moderate- to severe pathology range on GAF49 and below normal range on affect consciousness.50 Diagnoses were diverse, the most common being affective disorders (42%), trauma/stress-disorders (14.4%), personality disorders (13.3%), and psychosis (11.6%) (Supplement, Table S9). Fewer participants in medication-free treatment used psychotropics at baseline (78% versus 91.1%). This research sample seems representative when compared with other sources for admissions during the recruitment period on available demographics (Supplement, Tables S10 and 11). The exception was for some diagnostic groups in the TAU group, in which patients with psychosis and personality disorders were underrepresented by 10.2% and 9.2%, respectively, compared with the hospital statistics.
Patient Interview Sample
Two patient participants were men, and three were women. To protect their confidentiality, female pseudonyms are used for all participants in the quotations presented here, and we do not report on their diagnoses. They ranged in age from 25 to 50 years, and included people born in Norway and elsewhere. One participant had never used psychotropic medication. The rest had attempted to stop taking such medication, either during the current stay or previously. Four of the five patient participants were not taking medication at the time of the interview. Medication groups mentioned were selective serotonin reuptake inhibitors (SSRIs), serotonin and noradrenalin reuptake inhibitors (SNRIs), anxiolytics, hypnotics, antipsychotics, and beta-blockers. Four had previously been admitted to an open psychiatric ward.
Staff Interview Sample
Seven staff participants were women, and one was a man. We have used female pseudonyms to protect anonymity. Five were nurses or assistant nurses, and the others had other professional backgrounds, which we do not report for confidentiality reasons. They had an average of 14 years’ experience in mental health care and 12 years in this treatment unit, ranging from a few years to several decades.
Treatment Characteristics
Quantitative Analyses of Comparative Treatment Characteristics: Treatment Elements, Type and Magnitude
Table 5 shows aspects of received psychosocial treatment.
Participants in the medication-free treatment had about twice as long treatment stays and a higher mean intensity of psychosocial treatment elements with a large51 effect size (η2 0.13–0.45 on regimen level comparison). Regarding the number of psychosocial treatment elements received, although the regimen level analysis indicated more elements in medication-free treatment than in TAU, there was no clear pattern at the ward level (Supplement, Table S5 and 6).
Findings on treatment with psychotropics and assessment are displayed in Table 6.
Fewer patients in the medication-free treatment group received treatment with medication by medium sized52 effects (phi 0.3–0.4 for regimen level comparisons). Regimen level analyses showed a larger reduction in the medication dose during treatment in MFT. However, the effect size was below medium51 and differences were not significant at the ward level.
Patients’ Experience of Admission Rated According to Various Dimensions
Table 7 shows patients experiences of the admission overall, and Table 8 shows details of the question about being respected for not wanting medication.
Participants in the medication-free treatment group were more satisfied with their treatment, as measured by the CSQ-8; the effect size was medium51 (η2 0.06). They were also more likely to feel respected for the wish not to use medication, both when including all patients and only those without a community treatment order (CTO); the effect sizes were large51 (η2 0.22–0.24). No patients in the medication-free treatment reported not being respected for their wish not to use medication. The experience of not being respected was more common in the 6 months before admission than during admission in the included units.
Supplemental Analyses of Outliers and Ward Level Trends
Sensitivity analyses without outliers did not change the results of the analyses.
Visual inspection of ward level patterns for spillover-effects (Supplement, Tables S5 and S7) shows the neighboring TAU ward was mostly more similar to the other TAU ward than to Medication-free ward. Regarding receiving assessment the pattern may indicate spillover effects with the two neighboring wards being more similar in doing less assessment than the distant TAU. There were no substantial effects on ward level (table S4).
The oneway between groups analysis of variance on ward level shows statistically significant differences in patient satisfaction F(2, 131) = 4.0, being respected for not wanting medication F(2, 26) = 6.9, treatment duration F(2, 179) = 84.6, and intensity of psychosocial treatment F(2, 44) = 12.6. Effect sizes calculated using eta squared was medium51 for satisfaction (0.06), and large51 for being respected for not wanting medication (0.22) and treatment duration (0.49). Post-hoc comparisons using the Tukey HSD test indicated that MFT differs from both comparison wards in higher patient satisfaction (M = 28.5, SD = 3.5), to a greater extent being respected for not wanting medication (M = 4.8, SD 0.5), and longer duration of treatment (M = 8.9 weeks, SD 2.2). Regarding categorical variables, there is significantly less treatment with medication on medication-free unit compared with both comparison wards on patient report and neighboring TAU ward on clinician report, with medium to large53 effect sizes (Cramer’s V 0.3–0.5). Distant TAU ward had insufficient clinician reports to be compared.
Hence, medication-free treatment robustly distinguishes itself from both wards regarding satisfaction, duration, intensity of psychosocial treatment, extent of treatment with medication, and being respected for not wanting medication.
Qualitative Analyses of Comparative Treatment Characteristics
In the qualitative analyses, both patients and staff expressed that the notion of medication-free treatment was somewhat ambiguous and that the name seems more “radical” than its manifestation in practice (ie, that medications are not prohibited). The border between mandate and specific content on this ward (eg, the Illness Management and Recovery (IMR) program) was unclear and how the medication-free mandate unfolded in practice, as compared with other approaches, was often difficult to depict. However, as shown below, both patients and staff described medication-free treatment overall as involving less use of medication and a greater focus on other forms of treatment, as well as increased availability of options for patients to reduce or not use medication. Staff also understood the mandate to encompass a more restrictive use of controlled substances, which are traditionally regarded as addictive.
Medication-Free Treatment Promotes Less Reliance on Medication During the Recovery Process
Both patients and staff reported that, in medication-free treatment, medication played a less central role in the recovery process and patients had greater support to reduce or not use medication. Patient participants reported they were now being listened to regarding medication issues, which contrasted with some of their previous experiences in other units in which they had experienced pressure to use medication:
(…) I notice a huge difference between him and other doctors (…) he doesn’t give a lot of medications. On the other ward, it was like “tell us if you need Imovane [sleeping pill]” or “say if you need …”, and I am like, “No thanks, I’m fine”. While here, [name of the doctor] is very like “no” because he wants to try other things first. And I think that is very good. (Bella, patient)
Staff described that the purpose of the unit was to provide patients the opportunity to manage their condition without using medication, especially those with a severe disorder for which staff would previously have had concerns about reducing their use of medication. However, this change had not been straightforward because reducing or discontinuing medication needs to be balanced against the risk of increased symptoms, and a careful approach is needed:
I am quite glad that patients can come in, and even if they have, ehm, a serious diagnosis, they can look at which medications are good for them and try to taper. And one has tapered medication for some patients but increased again because some develop psychosis or something else, and one tries to make changes carefully. (Beatrice, staff)
Staff could experience conflict between the patient’s wishes and the potential for worsening of the patient’s disorder:
At the same time we experienced she got more symptoms and delusions, and some of the other inpatients started to act differently, they showed a lot of care for this person, but we received feedback that, ehm, there were strange things at times (…) So we tapered as far as possible, together with the person, and it was sad to hear she was admitted to the acute ward a week after discharge. (…) She called the ward shortly after discharge saying she had gotten the wrong medications home and believing we had poisoned her and, I experienced that unsettling. (…) she wanted to taper more. (…) But I think we managed to create a good cooperation that that was not wise here and now (…) And that she perhaps should maintain the current dose a while longer. (…) she did not experience her symptoms as dangerous or unpleasant, she felt she got in touch with something good, and actually wanted to be there. (Donna, staff)
Staff described that, with medication-free treatment, they were more restrictive in prescribing controlled substances. Some believed it is important for patients to learn to manage their disorder without such substances because medication only removes the symptoms and not the problem. It was experienced as problematic when patients come to a medication-free ward with the intention of withdrawing from the use of controlled substances but change their mind after admission:
…there were instances where we had people who wanted controlled substances, and we don’t think that belongs on a medication-free ward (…) Now is their opportunity to really tackle this without (…) That is what is the purpose of our ward. (Gina, staff)
Staff participants sometimes perceived a conflict between the restrictive stance and avoiding the patient either suffering, compromising/disgracing themselves, or being in a state in which it is difficult to form an alliance.
Some staff participants described the idea of reducing medication for serious disorders as new and challenging, but they increasingly observed that it is possible. Some noted that working in the medication-free treatment unit had increased their awareness of potential overmedication in more traditional approaches. Those who said that their attitudes had not changed in this regard also described themselves as having been critical of the prominence of medication in psychiatry from before the implementation of medication-free treatment.
Medication-Free Treatment Promotes a Wider Range of Psychosocial Treatment Activities
Both patient and staff participants discussed the greater availability of psychosocial treatments and improvements in the treatment program. They believed that a greater focus on alternatives to medication is inherent to the mandate. Patient and staff participants described that patients are offered alternatives to medication to manage difficult feelings, such as talking through and receiving explanations:
More important alternatives than taking that pill. (…) it is dialogue. To talk things through. Focus on relaxation, focus on just feeling what happens in the body. And they [staff] are very good at explaining what actually happens physically in the body (…) When you have anxiety or when you are afraid or sad, or happy for that matter. In addition, the psychologists here are very good at… explaining why we have the different feelings. So, it becomes more logical why I react as I do because the feelings are actually made for different purposes (…) And it is so good to hear that, because then I sort of understand why I react as I do. In another way. (Diana, patient)
Staff noted that medication-free treatment is more tangible, active, and longer lasting. They described a more personal approach in group settings, which helped to foster group cohesion and experiences of community, recognition, and mutual learning. Before medication-free treatment was initiated, patients were discouraged from discussing their treatment with each other. However, the staff perceived that the culture within the unit was changing toward more openness. This may be reflected in patients’ experiences of having more room to express their feelings and to hear staff participants’ perspectives on their emotional reactions.
Staff described positive feedback from patients:
This IMR program, of course, is something that works, I feel. (…) It is a concrete tool that the patient works with (…) So I would say it is for the better. (…) In my experience, they have been very satisfied, those we have had again here. They say this should have come 20 years ago. (…) [They have] been in the system so many years, and nothing has worked, it has sort of been vague. (…) those two here now, they said this will be the last time, the last admission. So, that says a lot, it was quite moving to hear this. (Anna, staff)
The Treatment is More Demanding
All participants described the program as more intense and with higher expectations of patient participation, individual responsibility, and hard work than in other approaches. “it is actually quite a high pressure. (…) as I say to the patients, when you are here for 8 weeks you are actually at school” (Beatrice, staff). “Here, the crucial difference is that there is a lot of work. And that is a big advantage” (Elise, patient).
The theme of the high demand was not explicitly related to the medication-free mandate, and some staff participants related it to the recovery approach. Staff participants described that their role now had changed in that they were expected to take a step back and leave more work to the patient. Greater emphasis on group work meant less routine one-on-one contact between members of staff and patients. This also meant that patients needed to utilize the group setting for support or else initiate contact with the staff themselves. Staff participants regarded it as important that patients take responsibility for asserting their need for support, just as they would have had to outside the hospital setting. A similar attitude of needing to work harder and assuming more responsibilities was observed to affect the work of staff. However, they described this as more mixed than what was the case for patients; for example, the tasks were more demanding in some areas whereas other aspects of their work had become easier.
Patient participants described that other experienced inpatient settings involved greater emphasis on relaxation, and some expressed it had felt like being in “storage”. Several patients described the increased demands and higher level of activity in medication-free treatment as largely positive. Some connected this to a stronger sense of purpose and agency and described that the degree of pressure resulting from these expectations increased the likelihood of following through. However, some also experienced that this led to too much pressure and that they received insufficient support in asserting their individual needs.
Among staff participants, there were divided opinions as to whether the increased demands on patients narrow the patient population who attend the ward. Some noted that it is important to recognize the level of need for patients while simultaneously expecting patients to learn and develop. Such expectations were viewed as therapeutic interventions in themselves, which could help motivate patients, promote their agency, and aid recovery:
…the only thing we can promise them is hard work. (…) Over time, and that it is tough, and it will be hard work. And then you see a spark is lit. When you understand the treatment program (…) Then you want to try. (…) And they become motivated. (Fanny, staff)
Conversely, some staff participants noted that patients must be functioning rather well to be in the unit. Given the increased patient preparations around expectations, staff suspected that the patients eventually admitted to the unit represented a self-selected group of patients motivated to undertake the hard work:
…I think they are very prepared, when, ehm, when they come that it is hard work. (…) It is no rest home to be here for eight weeks. (…) There is much to take in, much to go through and much to cope with. (…) and we understand that, but they want to. (…) So, I believe those who choose to come here, they are motivated for it. (Heidi, staff)
Staff participants mentioned patients who had stated they were too depressed to be in the medication-free unit and others who wanted to come back and try again when they were feeling better. Given the changed role of the staff, there was some uncertainty about which patients the treatment would be suitable for and how to handle the more fragile patients within the new treatment approach.
The Status of Shared Decision-Making Compared with Traditional Services is Complex Overall, but Patients Have More Freedom to Reduce or Not Use Medication
As mentioned previously, patients and staff participants experienced that medication-free treatment provided patients with a greater influence regarding reduction of medication. However, staff participants also felt patients had less influence regarding the opportunity to receive controlled substances. These changes were understood to form part of the medication-free mandate. Both patient and staff participants described that the focus on individual goals in IMR as well as a treatment program fostering more patient activity contributed to increased patient ownership of the process. Some patients described that spending more time in treatment increased their influence overall. Staff reported that they now collected patients’ views and feedback more systematically to adjust the treatment program. There were mixed reports of the experience of coercion in patient interviews; some patient participants reported feeling safer, but others still feared being coerced.
Some patients seemed to feel empowered by the high expectations for treatment activities and taking on responsibilities. Despite the higher expectations for participation, they expressed a feeling of autonomy about this and internalized the sense of responsibility for participation in ways they had not before:
There is more going on. One works more and decides more for oneself. Or, one decides there as well, but one sort of has to… how shall I explain? One has to choose to participate in what is going on. (…) you sort of have to “yes, now I am going to IMR”, you can’t just sit and not take part in what happens when you are here… at least I think! (…) you have the responsibility to participate, in a way. You have responsibility for your treatment. And I think that is very good (…) if I sleep long then no one comes and like… or they come eventually, but they give you some time. While at [another ward] it was more like “now it is this, now we have to go”, “now you shall participate on this”, “now you shall do that”. While here it is like “Well, you have slept. That’s it, then you missed it”. (…) I find it wonderful [laughing] (…) For example I was not on IMR today because I felt queasy, and I just said I was not up to it. And then that was understandable (…) they don’t give in right away. It is like “but why not?” “but you could try and maybe it gets better” (…)» (…) it is okay that they ask as long as it does not cross that line. (Bella, patient)
As indicated above, other patient participants experienced the expectation as pressure and expressed a need for greater support in asserting their own needs:
…but I didn’t manage to say so much… I kept a lot to myself. (…) Yes, there is a lot of shame. Ugh, it is shame. I have it still. But I am working on it. (…) They should have asked me… I wish they had asked me how much I can manage. (.) Because when they say that it is. [thinking], yes when they say that it is mandatory. Then one feels one has to. (…) but at the same time, I was not conscious when I sat there. I heard nothing and I said nothing. (Anita, patient)
Integration and Integrative Statements Regarding Characteristics of Medication-Free Treatment
The mixed matrix for the integration of results is shown in Table 9. The integrated findings are summarized in integrative statements in the table
 |
Table 9 Joint Display for the Integration of Results |
Medication
The quantitative findings show less medication use on the medication-free ward and that patients feel more respected for not wanting medication than what was the case on the comparison wards. The qualitative findings elaborate upon how both patients and staff experience that medications play a less central role and complements by showing that there is an increased belief in medication-free alternatives among some staff and that they are also more restrictive regarding controlled substances the patients may want. Hence, both quantitative and qualitative results point to medication playing a less central role in medication-free treatment, providing more support for alternative paths.
Psychosocial Treatment
The quantitative findings document that the extent of psychosocial treatment differs from comparison wards. The qualitative findings document that this is experienced by both patients and staff, and that they also experience a richer treatment program characterized by increased openness and group cohesion. Hence, more extensive psychosocial treatment is reflected in both qualitative and quantitative findings.
Assessment
The extent of formal assessment seems equal to standard treatment in the quantitative findings, and is not mentioned in the qualitative findings regarding experience of treatment. It is mentioned regarding expectations for treatment, which is elaborated in Standal, Solbakken, Rugkåsa, Martinsen, Halvorsen, Abbass and Heiervang.54 Patterns on ward level indicate there may be spillover effects masking differences. hence, we cannot conclude strongly that this is similar.
Higher Demands
The finding regarding higher demands in medication-free treatment is most explicitly found in the qualitative material but may also be reflected in the higher intensity of psychosocial treatment elements in the quantitative data. The qualitative data elaborate the form it takes and how this is experienced differently by different patients.
Patient Influence
The quantitative findings indicate no substantial differences in overall patient influence except regarding being respected for the wish not to use medication, which is greater on the medication-free ward. The qualitative findings corroborate, complement and nuances this by showing that while there was increased support for using less medication, there were more restrictions on using controlled substances. While several changes were experienced to increase patient influence (goal focus in IMR, fostering patient activity, more time, collecting feedback more systematically), higher demands and more mandatory activity could lead to both increased and reduced senses of empowerment.
Patient Satisfaction
The quantitative findings indicate greater patient satisfaction on the medication-free ward. The qualitative findings complement this by showing changes that are regarded as positive by patients. Hence, greater satisfaction may be linked to a richer psychosocial treatment that focuses on patient participation and freedom from pressure to use medication.
Discussion
The core features of medication-free treatment were understood and experienced by both patient and staff participants as involving less use of medication and more focus on other forms of treatment, as well as patients having more room for reducing or not using medication. Staff also understood the mandate to encompass a more restrictive use of controlled substances that are traditionally regarded as addictive. Our findings suggest that staff participants have developed a greater belief in the potential for medication-free treatment but that the withdrawal of medications is complex and not straightforward. Another feature that distinguished medication-free treatment from traditional treatment was higher expectations of patients regarding their activity and responsibility. This may also be indirectly related to the medication-free mandate. Patients in medication-free treatment reported greater satisfaction with treatment, which may be linked to a richer psychosocial treatment that focuses on patient participation and freedom from pressure to use medication.
Our findings are similar to those of other investigations of medication-free services in terms of the less intense focus on medication as a means to recovery, more extensive psychosocial treatment, a greater focus on individual responsibility and staff experience of the challenges in balancing different issues.22–25 There also seems to be a common focus on patient influence.22,23,25 However, in our study, this seems to play out in nuanced ways, and the general measures of shared decision-making support for personal recovery, and alliance were not substantially different between medication-free treatment and TAU.
Overall, the ward seems to fulfil the main purpose of medication-free units, which is to contribute to the increased freedom of choice regarding medications. The ward is perceived as providing more alternatives to medication and as free from pressure to use medication. Patient satisfaction is greater in medication-free treatment than in TAU. However, the withdrawal of medication in patients with a serious disorder is not simple and straightforward, and staff are aware of the need to balance different issues. Nevertheless, they seem to provide a treatment environment in which patients feel more supported in choosing a medication-free path.
Although patients in medication-free treatment reported feeling significantly more respected for not wanting medication with a large effect size, few patient participants reported not being respected overall in the included wards (n = 5 or 7% of the patient respondents). There may be spillover effects in the hospital at large, or the units that participated in this study may have a greater awareness of this issue due to their participation in this study. Patients reported experiences before admission indicate that this is more prevalent elsewhere in mental health care (n = 24 or 25.8% of those for whom the question was applicable).
Changes toward a culture that values openness and expression of feelings may follow from the specific elements implemented, such as in the IMR program, which encourages patients to find support persons among their fellow patients.21 These changes may also follow from a greater focus on the psychosocial aspects of treatment in general, although there is no strict contradiction to the use of medication. If patients do not manage their feelings through medication, they must deal with them in other ways, which typically involves talking and sharing. Staff participants referred to former policies that prohibited patients from talking about their treatment with each other. Such policies aim to protect patients, but they also stifle openness. When the focus is on the psychosocial aspects, it may be less feasible, or even desirable, to protect patients in this way. Challenges occurring during interactions may be viewed as opportunities to learn, as well as necessary costs when working psychotherapeutically.
Participants noted the greater demands on the patients in the medication-free unit. Within this was a focus on individual responsibility, which seems to be a shared feature of several medication-free units.23,25 In our material, this was not explicitly linked to the medication-free mandate but sometimes to the recovery approach. However, both the recovery approach and medication-free mandate share an inherent critique of the traditional approaches in mental health care that minimize the patient’s influence regarding medication.20 The recovery tradition also positions itself as an alternative to the traditional approach by shifting emphasis from professional accountability and control, which rewards passivity and compliance, to personal responsibility and self-management.55 Therein lies a probable link between the medication-free mandate, recovery approach, focus on individual responsibility, and focus on more active ways of coping.
There is a tension within the recovery tradition regarding individualism in the sense of highlighting individual responsibility.56 This focus has been criticized for neglecting structural, environmental and societal conditions, and challenges.56–58 The user organization Recovery in the bin distinguishes between the initial grassroots recovery movement and a newer co-opted recovery version that is consistent with neoliberalism.58 Price-Robertson, Obradovic and Morgan56 have promoted the notion of relational recovery, which highlights the idea of humans as interdependent relational beings. This aligns with the more radical conceptualization of empowerment as a collective and political struggle for the rights of underprivileged groups, which includes raising awareness about connections between a person’s life and outer societal conditions, as well as the possibility that others in the same circumstances may experience the same struggles.59 With the focus on individual responsibility, several medication-free units, including this one, seem to be on the more individualistic path.23,25 Our results suggest that this can lead to feeling both more and less empowered.
The underlying question of the place for individual responsibility is fraught with philosophical and political issues, and difficult to pinpoint empirically. However, it is important to undertake continuous reflections on how different positions affect and shape interactions with different patients, including their opportunities for shared decision-making. Our findings indicate that patient needs and wishes may be difficult to express when they conflict with expectations in the treatment culture, whether related to adherence to medication or assuming responsibility and working hard. Hence, reflexivity is crucial for avoiding pitfalls in either direction.
Strengths and Limitations
Mixed-methods designs give the opportunity for a more in-depth investigation of the influences at play in this context. This can facilitate theoretical generalization as well as the triangulation of results obtained using different methods.
The disadvantage of the local nature of the study is that data from different contexts were not available. The results may be colored by the unique characteristics of the local medication-free unit compared with the available alternatives and how these are presented to the patients via referrers, the media, the medication-free unit, or other sources. The unit under study, like most MFT units in Norway, is at an intermediate level of care and excludes the most acute conditions. Hence, MFT might appear different in other populations.
The patients were not randomized to medication-free treatment but rather prepared in advance to enable them to make a choice whether this was the right treatment regimen for them. Hence, we may have missed including participants who may have been more critical of the focus in this particular ward.
The response rate for the questionnaires on the medication-free ward was high (73.8%), and lower in the TAU unit (41.5%). However, our research sample was fairly representative of the population admitted to the wards during the inclusion period. There may have been bias in the selection for interviews because about half of the patients declined to participate in the interview, and the resulting sample was small. From what is known about the reasons for declining such participation, we may have missed including the most distressed patients.
According to posthoc sensitivity calculations there may be below medium sized differences that could have been significant in a larger sample.
Because interview participants were sampled before the questionnaire participants and questionnaire recruitment stretched over years, changes in the ward over time may have affected the data sources differently.
Conclusions
The core features of medication-free treatment involve less use of medication, a greater focus on psychosocial aspects in the process of recovery, and more room for patients to reduce or not use medication. In the medication-free ward, patients reported feeling more supported in choosing a medication-free path even as medication was withdrawn carefully, and staff participants were aware of the risks and complexity. The psychosocial treatment in the medication-free unit is more extensive and entails a culture of openness and room for patients to express their feelings, and a greater focus on individual responsibility and intensive work. Our findings of more extensive psychosocial treatment, less reliance on medications, a greater focus on individual responsibility, and staff struggles with specific dilemmas are similar to those reported by other investigations of medication-free services.22–25
This study illustrates how a medication-free treatment service works and that it can provide a viable alternative for people not comfortable with the current focus of medication in mental health care. Alluding to debates within and around the recovery tradition, mental health professionals should be conscious of the dimensions of individualism–relationalism in such treatment services.
Future Directions
Shared decision-making is complex, and we need greater clarity about how to create a healthcare system that is flexible enough to accommodate individual patients’ needs in the best possible manner. To improve shared decision-making in mental healthcare at large, one could examine the attitudes of mental health professionals toward medication-free treatment, identify potential barriers to its implementation and develop strategies to address these barriers and promote the integration of medication-free options into standard care. Factors that contribute to patient satisfaction in medication-free treatment could be investigated in more detail and across units to identify specific aspects of psychosocial treatment that are most valued by patients. We need more knowledge about long-term outcomes and cost effectiveness of different treatment strategies and in different populations.
Abbreviations
MFT, Medication-free treatment; TAU, Treatment as usual; C, Clinician; P, Patient; CTO, Community treatment order; WHO, World Health Organization; CRPD, United Nations Convention on the Rights of Persons with Disabilities; DDD, Defined daily dose according to the WHO; OQ, Outcome Questionnaire; AII, Affect Integration Inventory; GAF-F/S, Global Assessment of Functioning, function scale and symptom scale; SSRIs, Selective serotonin reuptake inhibitors; SNRIs, Serotonin and noradrenalin reuptake inhibitors; IMR, Illness Management and Recovery.
Trial Registration
This study is registered at ClinicalTrials.gov (NCT03499080), date 17/04/2018.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are not publicly available due to privacy regulations. The data contain health information and may be indirectly identifiable, hence are regarded as personal sensitive data. We do not have permission to share them outside of the research group.
Ethics Approval and Consent
The study was conducted in accordance with the Declaration of Helsinki and approved by the Regional Committee for Ethics in Research (2017/1056/REK sør-øst B.) and the Privacy Ombudsman at Akershus University Hospital (17–134). Participants gave written, informed consent before participation. All participants’ names are pseudonyms, and consent includes the publication of anonymous results.
Acknowledgments
We thank our participants, all the personnel at the involved treatment services, leaders and support personnel in the project. We especially thank Wenche Brandtzæg Nikolaisen, Anders Skogen Wenneberg, Bodil Skiaker, Camilla Kvaase, Lene Paulsen, Astrid Tiltnes, Svein Mossige, and Odd Arne Tjersland.
Christopher Wirshing is now at Lovisenberg hospital, Center for Mental Health and Addiction
Ingrid Engeseth Brakstad is now at the hospital Nordlandssykehuset, Districtpsychiatric center Lofoten and Vesterålen
IEB, CW, and Astrid Tiltnes have each written their master’s theses on the interview material. Public availability of their theses has been postponed until late 2023 to allow for the planned publication of articles on the research material. Themes and formulations under the introduction and method sections may overlap with previous publications on the same project,18,54,60 since the same project has investigated several research questions54,60 and we have previously written about the same phenomena and presented our project.18 However, results of our investigation of characteristics of medication-free treatment have not been published previously. A preprint61 is uploaded on Research Square.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Akershus University Hospital. The role of the funding body was to initiate the research project and provide salary and general working conditions.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Helse- og omsorgsdepartementet, Medikamentfrie tilbud i psykisk helsevern - oppfølging av oppdrag 2015 [Medication-free services in mental health care —- Follow-up of mission 2015]; 2015. Available from: www.regjeringen.no.
2. Fellesaksjonen for medisinfri behandling. Grunndokument. Fellesaksjonen for medisinfrie behandlingsforløp i psykiske helsetjenester. Available from: http://medisinfrietilbud.no/grunndokument/.
3. Helse Nord. Protokoll for medikamentfritt døgntilbud i Helse Nord; 2016. Available from: https://shorturl.at/dIL23.
4. Helse Sør-Øst. Overordnet protokoll for medisinfri behandling innen psykisk helsevern; 2016.
5. Sohler N, Adams BG, Barnes DM, Cohen GH, Prins SJ, Schwartz S. Weighing the evidence for harm from long-term treatment with antipsychotic medications: a systematic review. Am J Orthopsych. 2016;86(5):477–485. doi:10.1037/ort0000106
6. Semahegn A, Torpey K, Manu A, Assefa N, Tesfaye G, Ankomah A. Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta-analysis. Syst Rev. 2020;9(1):17. doi:10.1186/s13643-020-1274-3
7. World Health Organization (WHO). Guidance on Community Mental Health Services: Promoting Person-Centred and Rights-Based Approaches. World Health Organization; 2021.
8. United Nations (UN), United Nations Convention on the Rights of Persons with Disabilities; 2006. http://www.un.org/esa/socdev/enable/rights/convtexte.htm.
9. McGlashan TH, Carpenter WT. Identifying unmet therapeutic domains in schizophrenia patients: the early contributions of Wayne Fenton from Chestnut Lodge. Schizophrenia Bulletin. 2007;33(5):1086–1092. doi:10.1093/schbul/sbm082
10. Hauff E, Varvin S, Laake P, Melle I, Vaglum P, Friis S. Inpatient psychotherapy compared with usual care for patients who have schizophrenic psychoses. Psychiatric Serv. 2002;53(4):471–473. doi:10.1176/appi.ps.53.4.471
11. Mosher LR. Soteria and other alternatives to acute psychiatric hospitalization: a personal and professional review. J Nerv Mental Dis. 1999;187(3):142–149. doi:10.1097/00005053-199903000-00003
12. Calton T, Ferriter M, Huband N, Spandler H. A systematic review of the soteria paradigm for the treatment of people diagnosed with schizophrenia. Schizophrenia Bulletin. 2008;34(1):181–192. doi:10.1093/schbul/sbm047
13. Seikkula J, Aaltonen J, Alakare B, Haarakangas K, Keränen J, Lehtinen K. Five-year experience of first-episode nonaffective psychosis in open-dialogue approach: treatment principles, follow-up outcomes, and two case studies. Psychother Res. 2006;16(2):214–228. doi:10.1080/10503300500268490
14. Kafka JS. Chestnut Lodge and the psychoanalytic approach to psychosis. J Am Psychoanal Assoc. 2011;59(1):27–47. doi:10.1177/0003065111400906
15. Waugaman RM. Chestnut Lodge: an unreal place. Contemp Psychoanal. 2019;55(1):2):24–44. doi:10.1080/00107530.2019.1569921
16. Bergström T, Seikkula J, Alakare B, et al. The family-oriented open dialogue approach in the treatment of first-episode psychosis: nineteen-year outcomes. Psychiatry Res. 2018;270:168–175. doi:10.1016/j.psychres.2018.09.039
17. Friis S. Reflections on psychotherapeutic approaches to schizophrenic psychoses: past, present and future, by Alanen, de Chávez, Silver & Martindale. Scandinavian Psychoanalc Rev. 2010;33(1):47–51. doi:10.1080/01062301.2010.10592854
18. Standal K, Heiervang KS. Medisinfri behandling – et omstridt og etterlengtet tilbud. Medication-free treatment – controversial and awaited. Professional article. Tidsskrift Psykisk Helsearbeid. 2018;15(04):335–346. doi:10.18261/issn.1504-3010-2018-04-07
19. Slade M, Leamy M, Bacon F, et al. International differences in understanding recovery: systematic review. Epidemiol Psychiatr Sci. 2012;21(4):353–364. doi:10.1017/S2045796012000133
20. Slade M, Amering M, Oades L. Recovery: an international perspective. Epidemiol Epsichiatr Soc. 2008;17(2):128–137. doi:10.1017/s1121189x00002827
21. Mueser KT, Gingerich S. Kurs i personlige ferdigheter og mestringsstrategier for personer med alvorlige psykiske lidelser. (Hurtigoversetter.no. Adjusted by Karina M. Egeland, Sigrun Heskestad, Kristin S. Heiervang, Trans.): Hazelden; 2011.
22. Øvernes LA Medikamentfrie behandlingsforløp for personer med psykoselidelser. Erfaringer fra pilotprosjektet i Helse Bergen. 2019. Available from: https://helse-bergen.no/avdelinger/psykisk-helsevern/medikamentfritt-behandlingstilbod.
23. Wærness G Det går ikke knirkefritt, dette her. Miljøterapeuters erfaringer med medikamentfri behandling i psykisk helsevern. Universitetet i Tromsø; 2019. Available from: https://munin.uit.no/handle/10037/20247.
24. Oedegaard CH, Ruano AL, Blindheim A, et al. How can we best help this patient? Exploring mental health therapists’ reflections on medication-free care for patients with psychosis in Norway. Int J Ment Health Sys. 2022;16(1):1–19. doi:10.1186/s13033-022-00529-8
25. Bjørgen D, Kvisle IM, Johansen KJ, Leinan TBS, Benschop AR, Kildal C Legemiddelfri behandling – mitt liv, mitt valg! Bruker spør Bruker-evaluering av de legemiddelfrie behandlingstilbudene i fire helseregioner; 2020:
26. Røssberg JI. En debatt om alt og ingenting [A debate about everything and nothing]. Tidsskrift Norsk Psykologforening. 2021;58(7):608–611.
27. Berg HG Ahus frarøvet meg 15 år [Akershus University Hospital robbed me of 15 years]. Nettavisen 2016 https://www.nettavisen.no/nyheter/-ahus-frarovet-meg-15-ar/3423264411.html.
28. Monsen JT, Monsen K. Affekter og affektbevissthet: et bidrag til integrerende psykoterapimodell. In: Holte A, Nielsen GH, Rønnestad H, editors. Psykoterapi og psykoterapiveiledning Teori, empiri og praksis. Gyldendal Akademisk; 2000:71–90:chap 3.
29. Miller SD, Hubble MA, Chow D, Seidel J. Beyond measures and monitoring: realizing the potential of feedback-informed treatment. Psychotherapy. 2015;52(4):449–457. doi:10.1037/pst0000031
30. Seikkula J, Arnkil TE. Åpen dialog i relasjonell praksis. Respekt for annerledeshet i øyeblikket. Gyldendal Akademisk; 2013.
31. Hammer J, Heggdal D, Lillelien A, Lilleby P, Fosse R. Medisinfri etter basal eksponeringsterapi. Drug-free after basal exposure therapy. Tidsskriftet Den norske legeforening. 2018;138(6). doi:10.4045/tidsskr.17.0811
32. Tashakkori A, Johnson RB, Teddlie C. Foundations of Mixed Methods Research. Integrating Quantitative and Qualitative Approaches in the Social and Behavioral Sciences.
33. Heiervang KS. Medication Free Treatment: characteristics, Justification and Outcome. Trial registration. Clinicaltrials.gov Identifier: NCT03499080. Available from: https://clinicaltrials.gov/ct2/show/NCT03499080?term=Kristin+Heiervang&recrs=ab&cntry=NO&rank=1.
34. Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. doi:10.3758/BRM.41.4.1149
35. Foreningen for utgivelse av Norsk legemiddelhåndbok. Norsk legemiddelhåndbok. Available from: https://www.legemiddelhandboka.no/.
36. Ruud T, Gråwe RW, Hatling T Akuttpsykiatrisk behandling i Norge – resultater fra en multisenterstudie. SINTEF A310; 2006. Available from: https://sintef.brage.unit.no/sintef-xmlui/bitstream/handle/11250/2442757/SINTEF%2bRapport%2bA310.pdf?sequence=2&isAllowed=y.
37. Ruud T, Reas D. Distriktspsykiatriske sentre, tjenestetilbud og brukertilfredshet: status og variasjon 2002. STF78 A035008; 2002. Available from: https://www.sintef.no/globalassets/upload/helse/helsetjenesteforskning/stf78a035008.pdf.
38. Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluat Prog Plann. 1982;5(3):233–237. doi:10.1016/0149-7189(82)90074-x
39. Williams J, Leamy M, Bird V, et al. Development and evaluation of the INSPIRE measure of staff support for personal recovery. Social Psychiatry Psychiatric Epidemiol. 2015;50(5):777–786. doi:10.1007/s00127-014-0983-0
40. Tracey TJ, Kokotovic AM. Factor structure of the Working Alliance Inventory. Psychol Assess. 1989;1(3):207–210. doi:10.1037/1040-3590.1.3.207
41. Drivenes K, Vederhus J-K, Haaland VØ, et al. Enabling patients to cope with psychotropic medication in mental health care: evaluation and reports of the new inventory MedSupport. Medicine. 2020;99(1):e18635. doi:10.1097/MD.0000000000018635
42. Barr PJ, Forcino RC, Thompson R, et al. Evaluating CollaboRATE in a clinical setting: analysis of mode effects on scores, response rates and costs of data collection. BMJ Open. 2017;7(3):e014681. doi:10.1136/bmjopen-2016-014681
43. Barr PJ, Thompson R, Walsh T, Grande SW, Ozanne EM, Elwyn G. The psychometric properties of CollaboRATE: a fast and frugal patient-reported measure of the shared decision-making process. J Med Int Res. 2014;16(1):e2. doi:10.2196/jmir.3085
44. Ødegaard C. Medication free treatment in psychosis: the meaning of choice for people with psychosis – a qualitative exploration. University of Bergen; 2019. https://www.uib.no/en/cih/122122/christine-%C3%B8degaard-medication-free-treatment-psychosis.
45. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi:10.1191/1478088706qp063oa
46. Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scandinavian J Public Health. 2012;40(8):795–805. doi:10.1177/1403494812465030
47. Schoonenboom J, Johnson RB. The case comparison table: a joint display for constructing and sorting simple tables as mixed analysis. In: The Routledge Reviewer’s Guide to Mixed Methods Analysis. Routledge; 2021:277–288.
48. Gilles-Thomas D. Scoring and Interpreting the Outcome questionnaire-45. Summary from the OQ-45 Administration and Scoring Manual. 1998.
49. Karterud S, Pedersen G, Løvdahl H, Friis S. Global funksjonsskåring – Splittet versjon. Bakrgunn og skåringsveiledning. Klinikk for Psykiatri, Ullevål sykehus; 1998.
50. Solbakken OA, Monsen JT. Validation of the affect integration inventory short form (AII-SF-42). Int J Psychol Psychol Ther. 2021;21(1):107–122.
51. National University Academic Success Center. Partial Eta Squared; 2023. Available from: https://resources.nu.edu/statsresources/eta.
52. Cohen J. Statistical Power Analysis for the Behavioral Sciences.
53. Pallant J. SPSS Survival Manual.
54. Standal K, Solbakken OA, Rugkåsa J, et al. Why service users choose medication-free psychiatric treatment: a mixed-method study of user accounts. Research article. Patient Prefer Adher. 2021;15:1647–1660. doi:10.2147/PPA.S308151
55. Slade M 100 ways to support recovery: a guide for mental health professionals; 2009. Available from: https://shorturl.at/syGX5.
56. Price-Robertson R, Obradovic A, Morgan B. Relational recovery: beyond individualism in the recovery approach. Adv Ment Health. 2017;15(2):108–120. doi:10.1080/18387357.2016.1243014
57. Harper D, Speed E. Uncovering recovery: the resistible rise of recovery and resilience. Stud Soc Just. 2012;6(1):9–26. doi:10.26522/ssj.v6i1.1066
58. Recovery in the Bin, Edwards BM, Burgess R, Thomas E. Neorecovery: a survivor led conceptualisation and critique [Transcript].
59. Askheim OP. Empowerment – ulike tilnærminger. In: Askheim OP, Starrin B, editors. Empowerment i teori og prakis. Gyldendal Akademisk; 2007:21–34:chap 2.
60. Standal K, Solbakken OA, Jš B, Abbass A, Heiervang KS. Are People Worse off in Medication-Free Mental Health Treatment Than in Treatment as Usual? A Noninferiority Study of Medication-Free Inpatient Treatment in Mental Health Care. District Psychiatric Center Nedre Romerike, Akershus University Hospital; 2023.
61. Standal K, Solbakken OA, Rugkåsa J, et al. Medication-free treatment in mental health care. How does it differ from traditional treatment?. Research Square. 2023. doi:10.21203/rs.3.rs-3038199/v2
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.