Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 14
Lifting the Mask on Musculoskeletal Manifestations of COVID-19: Results of an Interview-Based Study
Authors Tharwat S , Shabana NM, Nassar MK
Received 30 May 2022
Accepted for publication 19 September 2022
Published 4 October 2022 Volume 2022:14 Pages 211—220
DOI https://doi.org/10.2147/OARRR.S376289
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Chuan-Ju Liu
Samar Tharwat,1 Noran Mohamed Shabana,2 Mohammed Kamal Nassar3
1Rheumatology and Immunology Unit, Internal Medicine Department, Mansoura University, Mansoura, Egypt; 2Mansoura Manchester Programme for Medical Education, Faculty of Medicine, Mansoura University, Mansoura, Egypt; 3Mansoura Nephrology & Dialysis Unit (MNDU), Department of Internal Medicine, Faculty of Medicine, Mansoura University, Mansoura, Egypt
Correspondence: Samar Tharwat, Mansoura University Hospital, El Gomhouria St, Mansoura, Dakahlia Governorate, Egypt, Tel +20 1091784143, Fax +2 50 2202834, Email [email protected]
Background: Coronavirus disease of 2019 (COVID-19) is considered a multi-system disease that might present with or develop complications during the acute phase of illness. The aim of this study was to describe the characteristics of musculoskeletal (MSK) manifestations in patients with COVID-19 infection and investigate their clinical correlations.
Methods: This study was carried out on 110 patients with a history of RT-PCR confirmed COVID-19 infection. They completed a questionnaire that covered detailed information on their sociodemographic characteristics, clinical data of COVID-19 infection in addition to MSK discomfort form based on the Nordic MSK Questionnaire.
Results: The mean age of the patients was 37.7 years (SD 12.9), 72.7% were females. The majority of patients (90.9%) reported MSK symptoms that occur during or shortly after the acute attack of COVID-19 infection. The median duration of onset of MSK symptoms was 2 days from the first day of COVID-19 infection (min-max: 0– 45 days) with a median duration of MSK symptoms of 7 days. Myalgia was the main complaint (85.5%) followed by arthralgia 90 (81.8%). However, swollen joints were reported in only 9 patients (8.2%). According to the body areas, maximum number of patients felt pain at the lower back (60%), followed by neck (39.1%), and upper back (32.5%) followed by right and left shoulder (20.9%). Patients with MSK manifestations were associated higher severity of COVID-19 infection (p < 0.001), prolonged duration of COVID-19 symptoms (p < 0.001) and higher prevalence of fatigue (p < 0.001).
Conclusion: MSK manifestations are common in COVID-19 patients and related to disease severity, duration and fatigue.
Keywords: musculoskeletal, COVID-19, Nordic MSK Questionnaire
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a new form of coronavirus was discovered in Wuhan, China, and has since spread throughout the world.1 The virus can cause asymptomatic infection or flu-like symptoms such as fever, cough, and shortness of breath.1 The condition can also lead to severe acute respiratory syndrome, pneumonia, and death in certain cases.2
Coronavirus disease of 2019 (COVID-19) is considered a multi-system disease that might present with or develop complications during the acute phase of illness. These complications include not only respiratory,3 but also cardiovascular,4 renal,5 gastrohepatic, thromboembolic,6 neurological,7 cerebrovascular,8 and autoimmune diseases.9
Patients with moderate and severe COVID-19 infection have also reported a significant musculoskeletal (MSK) burden, including skeletal muscle, bone, and joint abnormalities.10 Symptoms involving myalgia, arthralgia and muscle weakness can make it difficult for patients to perform activities of daily living like walking.11 Ironically, some of these MSK manifestations may occur before the most prevalent COVID-19 symptoms in some patients.3 The magnitude of viral replication, fever, and respiratory and systemic symptoms, including MSK manifestations, are directly correlated with interleukin-6 (IL-6) and tumor necrosis factor α (TNFα) levels in plasma and upper respiratory secretions.12 Also, proinflammatory conditions associated with prolonged ventilator times have been linked to muscle and bone manifestations.13
Identifying the MSK characteristics of the disease would be valuable and could provide further information to help with COVID-19 diagnosis and patient management. Thus, the aim of this study was to determine the frequency and pattern of MSK manifestations in patients with COVID-19 infection and investigate their clinical correlations.
Methods
Study Population
This interview-based cross-sectional study was conducted at the period from 25th July to 10th August 2021 at Internal Medicine department, Mansoura University Hospital. The work adhered to the 1995 Helsinki Declaration’s ethical standards and was approved by the Institutional Research Board of the Faculty of Medicine, Mansoura University (approval registration number: R.21.10.1469).
The study involved one hundred and ten patients (80 females, 23 males) from those who visited general medical outpatient clinic (follow-up or new cases). The inclusion criteria included patients aged >18 years old with a history of confirmed COVID-19 infection (by positive RT-PCR for COVID-19) in the last 8 months. Patients who had malignancies or any chronic rheumatic, MSK, or neurological disease before COVID-19 infection were excluded from the start. The study was explained to all participants, and written informed consent was obtained from all of them.
The Questionnaire
The questionnaire was created by the present authors and then revised and refined (Supplementary Data 1). It was distributed to the patients in Arabic version. The questions were written in an attempt to be as straightforward as possible. Answers were limited to yes/no questions (closed-ended questions). The questions covered detailed information on demographic and socioeconomic data including gender, age, marital status, residence, occupation, education, smoking habit and socioeconomic level. Participants were asked to indicate if they had ever been told by a doctor that they had any of the following conditions: diabetes mellitus, hypertension, chronic kidney disease or chronic lung disease, using a yes/no answer.
Participants were also enquired about their contact with a known COVID-19 case before getting infected. They were asked to mark the manifestations they were having at the time of COVID-19 infection and the positive investigations that confirmed their diagnosis. Additionally, they were questioned about the severity of COVID-19 infection, their need for oxygen supply or hospital admission and the duration of COVID-19 infection (from the first day until symptoms resolved).
The questionnaire also included questions about the MSK manifestations experienced by the patients during or shortly after infection with COVID-19, their onset (from the first day of COVID-19 infection), severity and duration.
The final part of the questionnaire is based on the Nordic Musculoskeletal Questionnaire, which has already been validated14 to determine the distribution of these MSK manifestations. It explores the prevalence of MSK disorders or discomfort in the neck, shoulder, elbow, wrist/hand, upper and lower back, ribs, hip/thigh, knee, leg or ankle and foot.
A team of six Internal Medicine staff members evaluated the generated questionnaire for input, critical appraisal, and content validation. On this premise, no new items were added, four were eliminated, and three were reworded. Following that, a preliminary questionnaire was developed and tested in a small group of participants (n = 15). The internal consistency of the questionnaire was determined using Cronbach’s alpha. The reliability coefficient was 0.83, indicating that the internal consistency was good.
Patients were contacted (in person) and informed about the questionnaire. Patients with a low level of education were given instructions on how to complete the questionnaire. The responses were then recorded into a Microsoft Excel spreadsheet.
Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics version 21 (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, version 21.0. Armonk, NY: IBM Corp). After examining the distribution of continuous variables for normality using the Shapiro–Wilk test, continuous variables with a normal distribution were described in mean ± standard deviation (SD) while those with abnormal distribution in median (minimum–maximum). Categorical variables were described in frequency (n) and percentage (%). For normally distributed data, the significance of differences between two groups was tested using the independent samples t-test, and for non-parametric variables, the Mann–Whitney test. For comparisons between qualitative variables, Chi-square or Fisher exact tests were used, as appropriate. The statistical significance level was p ≤ 0.05.
Results
A total of 110 patients with a history of confirmed COVID-19 infection were included in this study (Table 1), with a mean age of 37.7 years (SD 12.9), 72.7% were females and most of them were employed (60%). Ninety-two patients (83.6%) were nonsmokers, while about 31 (28.2%) had associated comorbid conditions. The majority of patients (90.9%) reported MSK symptoms (pain, discomfort, numbness) that occurred during or shortly after the acute attack of COVID-19 infection.
 |
Table 1 Demographic, Clinical Data of the Study Patients According to Musculoskeletal Manifestations |
As shown in Table 2, the median duration of onset of MSK symptoms was 2 days from the first day of COVID-19 infection (min-max: 0–45 days). The median duration of MSK symptoms was 7 days with maximum duration up to 7 months. Myalgia was the main complaint (85.5%) followed by arthralgia 90 (81.8%). However, swollen joints were reported in only 9 patients (8.2%). No one reported infectious arthritis. The severity of arthralgia ranged from mild (18.2%), moderate (32.7%), severe (23.6%) and very severe (7.3%).
 |
Table 2 Musculoskeletal and Rheumatic Manifestations Associated with COVID-19 Infection |
The distribution of MSK symptoms is shown in Figure 1. According to the body areas, maximum number of patients felt pain at the lower back (60%), followed by neck (39.1%), and upper back (32.5%) followed by right and left shoulder (20.9%). Left and right elbows were the least affected body areas (9.1% and 8.2% respectively).
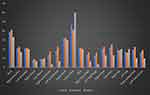 |
Figure 1 Distribution of MSK manifestations (pain, discomfort, numbness) associated with COVID-19 infection. |
There was no significant difference between patients with MSK symptoms and those without regarding their sociodemographic data. However, patients with MSK manifestations were associated with a more severe COVID-19 infection (p < 0.001). Additionally, significant difference existed between both groups regarding the presenting manifestations of COVID-19 infection such as shortness of breath (p = 0.006), loss of taste (p < 0.001), loss of smell (p = 0.001), loss of appetite (p = 0.001), headache (p < 0.001) and fever (0.013). Patients with MSK symptoms were also associated with prolonged duration of COVID-19 symptoms (p < 0.001) and higher prevalence of COVID-19-related fatigue (p < 0.001) as illustrated in Table 3.
 |
Table 3 COVID-19 Infection Data According to Musculoskeletal Manifestations |
Discussion
It has been demonstrated that coronavirus infections, like other respiratory illnesses, can cause MSK symptoms that range from arthralgia to spurious and chronic arthritis.15 However, COVID-19-related MSK complaints may not be linked to the development of pneumonia. Therefore, clinicians should be aware of COVID-19 variable onset to prevent missing a diagnosis, especially when respiratory symptoms are absent at the time of presentation.16
This is the first detailed study of MSK manifestations encountered by patients with COVID-19 infection, which utilizes Nordic MSK Questionnaire. The study includes those diagnosed with COVID-19 infection and provides data on the relation between MSK symptoms and clinical parameters in these patients.
The present study revealed that COVID-19 patients had a heavy MSK symptom burden. Also, the high prevalence of MSK symptoms was associated with higher severity of COVID-19 infection (p < 0.001), prolonged duration of COVID-19 symptoms (p < 0.001) and higher prevalence of fatigue (p < 0.001).
The most important result in this study is the high prevalence (90.9%) of MSK symptoms (pain, discomfort, numbness) related to COVID-19 infection. These results are much more higher than that of other studies, in which post-COVID-19 myalgia was found to be from 4.5% to 36% common, while post-COVID-19 arthralgia was shown to be from 6% to 27% common.17
This study confirmed the high prevalence of fatigue in COVID-19 patients, which was reported in almost all surveyed patients (90%). There is increasing concern regarding this point as recent research has found that more than half of patients suffer from fatigue, while other studies have found greater rates of arthralgia/myalgia symptoms.18,19
COVID-19 individuals may experience myalgia that lasts longer than typical viral infections and is resistant to conventional analgesics.20 This study found that the median duration of onset of MSK symptoms was 2 days from the first day of COVID-19 infection (min-max: 0–45 days). The MSK manifestations persisted up to 7 months in some patients.
The current study determined that myalgia was the main complaint (85.5%) followed by arthralgia (81.8%). These results are in accordance with recent studies indicating that myalgia is the most common MSK manifestation in COVID-19 patients.21,22 According to the Office for National Statistics, people infected with the new variant of COVID-19 found in the South East of England (known as B.1.1.7 or VUI 202012/01) are more likely to develop myalgia than those infected with other versions.23
Myalgia is the result of a cytokine response and widespread inflammation,24 as it is usually linked to MSK pain in the acute phase of COVID-19 infection.25 Additionally, it is associated with a higher risk of postoperative death among these patients.26
Arthralgia is also one of the symptoms that people with COVID-19 experience.27 Myalgias and arthralgias have been lumped together as a single entity in COVID-19 studies.16 In COVID-19, viral arthralgia is less common than myalgia, but it has been reported in other coronavirus infections.28,29 Patients with COVID-19 presented with acute arthralgia are typically younger, with no previous arthritic episodes or inflammatory joint effusions.16
The severity of arthralgia in the surveyed patients ranged from mild (18.2%), moderate (32.7%), severe (23.6%) and very severe (7.3%). COVID-19 arthralgia is usually more severe and has a variable onset, whereas generalized body pain and myalgia are usually milder and occur in association with fever or respiratory symptoms.16
In the current study, swollen joints were reported in only 9 patients (8.2%). Acute arthritis is known to be caused by viral infections.30 Post COVID-19 arthritis has been reported,31,32 and arthritis may even be the initial presenting symptom of COVID-19 infection.33 However, coronaviruses usually cause arthralgia and myalgia rather than clinical arthritis.27–29
Although the pathophysiology of viral-associated arthritis is yet unexplained, molecular mimicry is thought to play a role in the activation of the inflammatory process.34 There have been reports of molecular mimicry in the context of SARS-CoV2, and this mechanism could be involved in the pathogenesis of both the acute systemic infection and the post-infective viral-related immunological repercussions.35–37 Also, COVID-19 invasion receptors expressed in the MSK system were thought to be a possible target for the angiotensin-converting enzyme 2 (ACE2) enzyme.38,39
Despite the fact that classical reactive arthritis (ReA) is linked to urogenital and gastrointestinal infections, nonclassical ReA can be triggered by a wide range of infections.40 ReA can be caused by COVID-19 infection, and few cases of post-COVID-19 ReA have been published since the emergence of COVID-19.41–43
Only one case of septic arthritis induced by Neisseria meningitidis in a COVID-19 patient has recently been reported.44 However, no one reported infectious arthritis in our surveyed patients.
In this study, when we assessed the distribution of MSK symptoms among COVID-19 patients, maximum number of patients felt pain at the lower back (60%), followed by neck (39.1%), and upper back (32.5%) followed by right and left shoulder (20.9%). In an extension cohort study carried out on COVID-19 patients, joint pain and myalgia were both common; if regional, joint pain was most common in the knee, foot–ankle, and shoulder, while myalgia was most common in the lower leg, arm, and shoulder girdle.45 In another single-center cohort study conducted on 300 participants, two phone interviews were conducted (2-week and 1-month after hospitalization) and MSK symptoms were inquired with a standardized questionnaire, the authors found that back pain, arthralgia, myalgia, low back pain, and neck discomfort were the most frequent MSK symptoms.46
In this study, there was no significant difference between patients with MSK symptoms and those without regarding their gender or age. In contrast, another study found that fatigue, myalgia, and joint pain were more common in female patients with COVID-19 infection.45
SARS patients with moderate and severe infections have a significant MSK burden.47–49 The results of the current study indicated that patients with MSK manifestations were associated with higher severity of COVID-19 infection (p < 0.001) with prolonged duration of COVID-19 symptoms (p < 0.001) and higher prevalence of fatigue (p < 0.001). These results are in agreement with those obtained by Bakılan and coauthors50 who found that higher frequency of dyspnea, respiratory symptoms in addition to longer duration of hospital stay are related to post-COVID-19 MSK symptoms.
A number of limitations need to be noted regarding the present study. First, the study only included patients who were admitted to an Internal Medicine clinic. Our findings cannot be applied to all COVID-19 patients. Second, the method of data collection, which was based on self-reporting, may have influenced the study outcome. Third, the number of participants was to some extent small to give an acceptable value. Fourth, the majority of the patients in this study were females, which is atypical for COVID-19 infection, and the mean age was younger than in most previously published studies. Finally, the lack of a control group was another limitation.
However, there are many strengths to this study; this is one of the earliest studies conducted in Egypt and addresses the involvement of MSK system in COVID-19 patients. Also, the questionnaire is comprehensive and straightforward, and an in-person interview was conducted.
For future endeavors, improving the population size and involving a control group are highly recommended. Further research is needed to establish the prevalence of MSK manifestations in the general population after COVID-19.
Conclusion
MSK manifestations are common in COVID-19 patients and related to disease severity and duration. Therefore, recognizing the MSK aspects of the disease would be valuable and could provide further information to help with the diagnosis and management of COVID-19 patients.
Abbreviations
COVID-1, coronavirus disease of 2019; IL-6, interleukin-6; MSK, musculoskeletal; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; SD, standard deviation; TNFα, tumor necrosis factor α.
Data Sharing Statement
The data are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
A written informed consent was obtained from all participants, and Ethical Approval was obtained from Institutional Research Board of the Faculty of Medicine, Mansoura University (approval registration number: R.21.10.1469).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
No potential conflict of interest was reported by the authors.
References
1. Harapan BN, Yoo HJ. Neurological symptoms, manifestations, and complications associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease 19 (COVID-19). J Neurol. 2021;268:3059–3071. doi:10.1007/s00415-021-10406-y
2. Hui DS, Azhar EI, Madani TA, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020;91:264–266. doi:10.1016/j.ijid.2020.01.009
3. Zhao H, Shen D, Zhou H, Liu J, Chen SJ. Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol. 2020;19:383–384. doi:10.1016/S1474-4422(20)30109-5
4. Madjid M, Safavi-Naeini P, Solomon SD, Vardeny OJ. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020;5:831–840. doi:10.1001/jamacardio.2020.1286
5. Gross O, Moerer O, Weber M, Huber TB, Scheithauer SJ. COVID-19-associated nephritis: early warning for disease severity and complications? Lancet. 2020;395:e87–e8. doi:10.1016/S0140-6736(20)31041-2
6. Jiménez D, García-Sanchez A, Rali P, et al. Incidence of VTE and bleeding among hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Chest. 2021;159:1182–1196. doi:10.1016/j.chest.2020.11.005
7. Favas T, Dev P, Chaurasia RN, et al. Neurological manifestations of COVID-19: a systematic review and meta-analysis of proportions. Neurol Sci. 2020;41:3437–3470. doi:10.1007/s10072-020-04801-y
8. Yamakawa M, Kuno T, Mikami T, et al. Clinical characteristics of stroke with COVID-19: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2020;29:105288. doi:10.1016/j.jstrokecerebrovasdis.2020.105288
9. Galeotti C, Bayry JJ. Autoimmune and inflammatory diseases following COVID-19. Nat Rev Rheumatol. 2020;16:413–414. doi:10.1038/s41584-020-0448-7
10. Disser NP, De Micheli AJ, Schonk MM, et al. Musculoskeletal consequences of COVID-19. J Bone Joint Surg Am. 2020;102:1197. doi:10.2106/JBJS.20.00847
11. Abdullahi A, Candan SA, Abba MA, et al. Neurological and musculoskeletal features of COVID-19: a systematic review and meta-analysis. Front Neurol. 2020;11:687. doi:10.3389/fneur.2020.00687
12. Misra DP, Agarwal V, Gasparyan AY, Zimba OJ. Rheumatologists’ perspective on coronavirus disease 19 (COVID-19) and potential therapeutic targets. Clin Rheumatol. 2020;39:2055–2062. doi:10.1007/s10067-020-05073-9
13. Kizilarslanoglu MC, Kuyumcu ME, Yesil Y, Halil MJ. Sarcopenia in critically ill patients. J Anesth. 2016;30:884–890. doi:10.1007/s00540-016-2211-4
14. Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233–237. doi:10.1016/0003-6870(87)90010-X
15. Marks M, Marks JL. Viral arthritis. Clin Med. 2016;16:129. doi:10.7861/clinmedicine.16-2-129
16. Hoong CWS, Amin MN, Tan TC, Lee JE. Viral arthralgia a new manifestation of COVID-19 infection? A cohort study of COVID-19-associated musculoskeletal symptoms. Int J Infect Dis. 2021;104:363–369. doi:10.1016/j.ijid.2021.01.031
17. Shanbehzadeh S, Tavahomi M, Zanjari N, Ebrahimi-Takamjani I, Amiri-Arimi SJ. Physical and mental health complications post-COVID-19: scoping review. J Psychosom Res. 2021;147:110525. doi:10.1016/j.jpsychores.2021.110525
18. Goyal P, Choi JJ, Pinheiro LC, et al. Clinical characteristics of Covid-19 in New York city. N Engl J Med. 2020;382:2372–2374. doi:10.1056/NEJMc2010419
19. Escalera-Antezana JP, Lizon-Ferrufino NF, Maldonado-Alanoca A, et al. Clinical features of the first cases and a cluster of Coronavirus Disease 2019 (COVID-19) in Bolivia imported from Italy and Spain. Travel Med Infect Dis. 2020;35:101653. doi:10.1016/j.tmaid.2020.101653
20. Kucuk A, Cumhur Cure M, Cure EJ. Can COVID-19 cause myalgia with a completely different mechanism? A hypothesis. Clin Rheumatol. 2020;39:2103–2104. doi:10.1007/s10067-020-05178-1
21. Batur EB, Korez MK, Gezer IA, Levendoglu F, Ural OJ. Musculoskeletal symptoms and relationship with laboratory findings in patients with COVID‐19. Int J Clin Pract. 2021;75:e14135. doi:10.1111/ijcp.14135
22. Ramani SL, Samet J, Franz CK, et al. Musculoskeletal involvement of COVID-19: review of imaging. Skeletal Radiol. 2021;50:1763–1773. doi:10.1007/s00256-021-03734-7
23. Mahase E. Covid-19: sore throat, fatigue, and myalgia are more common with new UK variant. BMJ. 2021;372:n288.
24. Lippi G, Wong J, Henry BM. Myalgia may not be associated with severity of coronavirus disease 2019 (COVID-19). World J Emerg Med. 2020;11:193. doi:10.5847/wjem.j.1920-8642.2020.03.013
25. Fernández-de-Las-Peñas C, Rodríguez-Jiménez J, Fuensalida-Novo S, et al. Myalgia as a symptom at hospital admission by severe acute respiratory syndrome coronavirus 2 infection is associated with persistent musculoskeletal pain as long-term post-COVID sequelae: a case-control study. Pain. 2021;162:2832–2840. doi:10.1097/j.pain.0000000000002306
26. Huang Y, Tu M, Wang S, et al. Clinical characteristics of laboratory confirmed positive cases of SARS-CoV-2 infection in Wuhan, China: a retrospective single center analysis. Travel Med Infect Dis. 2020;36:101606. doi:10.1016/j.tmaid.2020.101606
27. Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. NEJM. 2020;382:1708–1720. doi:10.1056/NEJMoa2002032
28. Friedman N, Alter H, Hindiyeh M, Mendelson E, Shemer Avni Y, Mandelboim MJV. Human coronavirus infections in Israel: epidemiology, clinical symptoms and summer seasonality of HCoV-HKU1. Viruses. 2018;10:515. doi:10.3390/v10100515
29. Memish ZA, Perlman S, Van Kerkhove MD, Zumla AJ. Middle East respiratory syndrome. Lancet. 2020;395:1063–1077. doi:10.1016/S0140-6736(19)33221-0
30. Varache S, Narbonne V, Jousse‐Joulin S, et al. Is routine viral screening useful in patients with recent‐onset polyarthritis of a duration of at least 6 weeks? Results from a nationwide longitudinal prospective cohort study. Arthritis Care Res. 2011;63:1565–1570. doi:10.1002/acr.20576
31. Joob B, Wiwanitkit VJ. Arthralgia as an initial presentation of COVID-19: observation. Rheumatol Int. 2020;40:823. doi:10.1007/s00296-020-04561-0
32. Parisi S, Borrelli R, Bianchi S, Fusaro EJ. Viral arthritis and COVID-19. Lancet Rheumatol. 2020;2:e655–e7. doi:10.1016/S2665-9913(20)30348-9
33. Peral-Garrido ML, Calabuig I, Tovar-Sugrañes E, et al. Case series of acute arthritis during COVID-19 admission. Ann Rheum Dis. 2021;80:e58–e. doi:10.1136/annrheumdis-2020-217914
34. Fujinami RS, von Herrath MG, Christen U, Whitton JL. Molecular mimicry, bystander activation, or viral persistence: infections and autoimmune disease. Clin Microbiol Rev. 2006;19:80–94. doi:10.1128/CMR.19.1.80-94.2006
35. Cappello FJ. Is COVID-19 a proteiform disease inducing also molecular mimicry phenomena? Clin Microbiol Rev. 2020;25:381–382.
36. Cappello F, Marino Gammazza A, Dieli F, Conway de Macario E, Macario AJ. Does SARS-CoV-2 trigger stress-induced autoimmunity by molecular mimicry? A hypothesis. J Clin Med. 2020;9:2038. doi:10.3390/jcm9072038
37. Angileri F, Legare S, Gammazza AM, de Macario EC, Macario AJ, Cappello FJ. Molecular mimicry may explain multi-organ damage in COVID-19. Autoimmun Rev. 2020;19:102591. doi:10.1016/j.autrev.2020.102591
38. Cabello‐Verrugio C, Morales MG, Rivera JC, Cabrera D, Simon FJ. Renin‐angiotensin system: an old player with novel functions in skeletal muscle. Med Res Rev. 2015;35:437–463. doi:10.1002/med.21343
39. Ding Y, He L, Zhang Q, et al. Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS‐CoV) in SARS patients: implications for pathogenesis and virus transmission pathways. J Pathol. 2004;203:622–630. doi:10.1002/path.1560
40. Kim T-H, Uhm W-S, Inman RD. Pathogenesis of ankylosing spondylitis and reactive arthritis. Curr Opin Rheumatol. 2005;17:400–405. doi:10.1097/01.bor.0000163447.44037.c4
41. Yokogawa N, Minematsu N, Katano H, Suzuki TJ. Case of acute arthritis following SARS-CoV-2 infection. Ann Rheum Dis. 2021;80:e101–e. doi:10.1136/annrheumdis-2020-218281
42. Ono K, Kishimoto M, Shimasaki T, et al. Reactive arthritis after COVID-19 infection. RMD Open. 2020;6:e001350. doi:10.1136/rmdopen-2020-001350
43. Saricaoglu EM, Hasanoglu I, Guner RJ. The first reactive arthritis case associated with COVID‐19. J Med Virol. 2021;93:192–193. doi:10.1002/jmv.26296
44. Ducatez N, Chancel M, Douadi Y, et al. Primary meningococcal arthritis in a COVID-19 18-year-old man: a case report and review of the literature. BMC Infect Dis. 2021;21:1–4. doi:10.1186/s12879-021-06211-7
45. Karaarslan F, Güneri FD, Kardeş SJ. Long COVID: rheumatologic/musculoskeletal symptoms in hospitalized COVID-19 survivors at 3 and 6 months. Clin Rheumatol. 2022;41:289–296. doi:10.1007/s10067-021-05942-x
46. Karaarslan F, Demircioğlu Güneri F, Kardeş SJ. Postdischarge rheumatic and musculoskeletal symptoms following hospitalization for COVID-19: prospective follow-up by phone interviews. Rheumatol Int. 2021;41:1263–1271. doi:10.1007/s00296-021-04882-8
47. Tsai L, Hsieh S, Chang YJ. Neurological manifestations in severe acute respiratory syndrome. Acta Neurol Taiwan. 2005;14:113.
48. Leung TW, Wong KS, Hui AC, et al. Myopathic changes associated with severe acute respiratory syndrome: a postmortem case series. Arch Neurol. 2005;62:1113–1117. doi:10.1001/archneur.62.7.1113
49. Griffith JF. Musculoskeletal Complications of Severe Acute Respiratory Syndrome. Semin Musculoskelet Radiol. © Thieme Medical Publishers; 2011.
50. Bakılan F, Gökmen İG, Ortanca B, et al. Musculoskeletal symptoms and related factors in postacute COVID‐19 patients. Int J Clin Pract. 2021;75:e14734. doi:10.1111/ijcp.14734
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
