Back to Journals » Patient Preference and Adherence » Volume 18
Knowledge of Common Symptoms of Rheumatic Diseases and Causes of Delayed Diagnosis in Saudi Arabia
Authors Al-Mehmadi BA , Alelaiwi MMM, Alnumayr HSA, Alghamdi BS, Alomari BA, Alzahrani HS
Received 9 November 2023
Accepted for publication 17 February 2024
Published 8 March 2024 Volume 2024:18 Pages 635—647
DOI https://doi.org/10.2147/PPA.S448999
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Bader A Al-Mehmadi,1 May Musaad M Alelaiwi,2 Haya Sulaiman A Alnumayr,3 Basil Saeed Alghamdi,4 Bandar Abdullah Alomari,4 Hayat Saleh Alzahrani5
1Department of Internal Medicine, College of Medicine, Majmaah University, Al-Majmaah, 11952, Saudi Arabia; 2College of Medicine, Majmaah University, Al-Majmaah, Saudi Arabia; 3College of Medicine, Qassim University, Buraydah, Saudi Arabia; 4Department of Internal Medicine, King Fahad Hospital, Medina, Saudi Arabia; 5Department of Family and Community Medicine, College of Medicine, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia
Correspondence: Hayat Saleh Alzahrani, Department of Family and Community Medicine, College of Medicine, Princess Nourah bint Abdulrahman University, P.O. Box 84428, Riyadh, 11671, Saudi Arabia, Tel +96611822000, Email [email protected]; [email protected]
Purpose: The aim of this study is to determine the general population’s knowledge on the different symptoms of rheumatic diseases, the key factors for diagnosis delays from the patient’s perspective, the length of delay from the onset of symptoms to the diagnosis, and the effect this holds on the disease activity, response to therapy, and the development of complications and nonreversible deformities in patients diagnosed with rheumatic diseases.
Patients and Methods: This is a cross-sectional study. Our target study population were the residents of Saudi Arabia. Data were collected via an online questionnaire and analyzed with SPSS.
Results: The overall prevalence of rheumatic disease in our cohort was 8.7%. Joint pain (75.7%), joint swelling (47.1%) and morning stiffness (32.9%) were the first and most common presenting symptom. Persistence of symptoms (N=32, 45.7%) and symptom worsening (N=21, 30.0%) was the predominant cause to visit rheumatologist. The duration between first symptom and rheumatic disease diagnosis is significantly longer for patients aged < 50 years compared to that of those with ≥ 50 years of age. Results show that 36.4% of patients aged ≥ 50 years had delayed diagnosis due to late appointment compared with 5.7% of patients aged < 50 years. In addition, patients with longer duration of symptoms were likely to have more visits to the rheumatologist. Most of the participants of < 50 years significantly agreed that rheumatologists treat autoimmune diseases, only a few approved that they treat muscle problems.
Conclusion: Most participants in our study have lesser knowledge about their symptoms and they did not know where to consult for the treatment of their disease. This caused unnecessary delays and worsening and aggravation of the symptoms. There is an increased need to organize an awareness campaign in the general population regarding autoimmune and rheumatic diseases.
Keywords: rheumatic diseases, delayed diagnosis, misdiagnosis, referrals, consultations, Saudi Arabia
Introduction
Rheumatic diseases (RD) are a group of conditions that have an impact on the muscles, joints, and other connective tissues.1 There are currently over 200 distinct rheumatic diseases, with rheumatoid arthritis, osteoarthritis, lupus, gout, infectious arthritis, and spondyloarthropathies being the most prevalent.2 These diseases are characterized by joint discomfort, swelling, morning stiffness that can last for more than half an hour, inflammation, and limited joint mobility.2,3 They can be difficult to diagnose, therefore understanding the expected clinical appearance is essential.1
Patients with systemic lupus erythematosus may exhibit photosensitive malar rash, hair loss, and unexplained weight loss, which may not suggest a single organ pathology.2,3 Patients with rheumatoid arthritis may exhibit pain, stiffness, and edema in affected joints, skin nodules, joint deformity, and Raynaud’s phenomenon, among other manifestations.4 Rheumatic diseases are caused by multiple factors, including genetics, environment, lifestyle, infections, and metabolic disorders.5,6
In general, there is no specific test to diagnose rheumatic diseases; however, the signs and symptoms lead to tests that confirm the diagnosis.7 Many untrained physicians may misdiagnose a patient with rheumatoid arthritis due to the finding of a positive rheumatoid factor, even though the clinical presentation was not suggestive of this diagnosis, whereas it may be found positive in many other rheumatic and nonrheumatic diseases, such as hypothyroidism.7,8 Patients of rheumatoid arthritis can, however, have a negative rheumatoid factor that may cause a delay in reaching the diagnosis and in initiating the appropriate treatment for them.9 The same is true for antinuclear antibodies, which are not specific for a particular diagnosis and may even be a normal variant in individuals with low antinuclear antibody titers and no supporting clinical manifestation.10 Thus, the field of rheumatology faces difficulties in diagnosing many patients with vague symptoms, and clinics are overwhelmed with unnecessary referrals because asymptomatic patients are referred for a positive serology ordered as “screening tests”.
Significant delays are observed between the onset of disease and the initiation of treatment, resulting in increased rates of unnecessary suffering and disability, as well as complications including irreversible deformities, organ damage, lower quality of life, and even death.9
There are different factors that can all contribute to a delayed diagnosis of rheumatic diseases. Among the factors that can contribute to a delayed diagnosis of rheumatic disease are patient-specific factors; some patients may delay seeking medical care for their symptoms.9 This could be due to the belief that their symptoms are not serious as they may be progressing slowly, so initial symptoms may not be severe enough to warrant a visit to the doctor, the preference to first try traditional/herbal remedies to treat their symptoms, the fear of being diagnosed with a chronic illness and committing to immunosuppressive therapies that can reduce immunity and cause side effects, and the lack of access to health-care services.9
In some cases, nonspecialist physicians (who are frequently the first physicians consulted by patients) may fail to recognize the symptoms and signs of rheumatic diseases. This may be due to a lack of training in rheumatology, the belief that the patient’s symptoms are caused by another condition, or the patient’s failure to provide a complete medical history.11 Systemic factors can also contribute to the delayed diagnosis of rheumatic diseases. This may be due to lengthy wait times for appointments, a lack of access to specialists, high health care costs, and a lack of medical insurance coverage.9,11
In Saudi Arabia, it is still unknown if this discrepancy is due to variations in diagnostic criteria, a real differential in susceptibility among certain national populations, or a mix of both of these variables. However, altogether musculoskeletal (MSK) diseases rank as the second most common reason Saudi Arabians attend primary health centres (PHCs) and private clinics for outpatient care.12 In reality, a study of RA patients (who met the 2010 American College of Rheumatology criteria for RA) in Saudi Arabia revealed that it might take up to 30 months from the time symptoms appear to the time a diagnosis is made.13 The authors revealed that RA patients frequently do not consult rheumatologists when their symptoms first appear, and nonrheumatologists frequently neglect to send RA patients to rheumatologists in a timely manner.13 According to a different survey, the majority of Saudi patients with RA (55%) report a decline in their job capacity of more than 50%.14
Musculoskeletal (MSK) examination is the most common way for the diagnosis of RD, however, mostly primary health-care physicians are unaware of it. The use of advance radiological techniques is also growing, though they are not readily available PHCs in Saudi Arabia. A group of researchers proposed a set of guidelines known as the New Early Arthritis Referral Criteria that are meant to enhance the identification of early RD by MSK examination.15 MSK ultrasonography is accessible in most of rheumatology clinics in Saudi Arabia, which is helpful in the diagnosis of RD. In Saudi Arabia, the detection of rheumatic diseases in clinical practice relies both on local and international experiences, as well as the utilization of various assisting tools such as the guidelines provided by the American College of Rheumatology (ACR) for diagnosing different rheumatic diseases,16 and the European Alliance of Associations for Rheumatology (EULAR).17,18 The Saudi Society of Rheumatology in Saudi Arabia (SSRSA) has organized various awareness campaigns, conferences, workshops, and webinars throughout Saudi Arabia.19,20 These initiatives aim to educate nonrheumatologist doctors and susceptible individuals about the symptoms and signs of rheumatologic diseases. In addition, the SSRSA has published numerous resources dedicated to educating the public about the major types of rheumatic diseases. These resources can be accessed through their patients’ portal.21
The current study aimed to ascertain the duration between the onset of the disease and the first clinical consultation and diagnosis, as well as the factors contributing to delayed diagnosis in Saudi Arabia. We aimed to learn more about the causes of delayed diagnosis in rheumatic disease patients. By comprehending the causes, we can assist patients in avoiding them in the future, resulting in fewer complications and a successful course of treatment with better outcomes.
Materials and Methods
Study Design and Study Area
The study utilized a cross-sectional online survey design. Data was collected through an online questionnaire which was distributed through social media platforms to the residents of Saudi Arabia in different regions. A total of 808 participants completed the questionnaire.
Study Time Period
The study was conducted after the ethical approval was taken. The data collection was started on September 9, 2022 and completed on October 11, 2022.
Target Population
The study included participants that were at the time of residing in Saudi Arabia; male and female both were included, and those who were ≥18 years of age. All others who were not willing to participate, did not give consent or <18 years of age were excluded.
Patient Consent
Informed consent was the part of online questionnaire and only participants who were voluntarily willing to participate completed the questionnaire.
Sample Size and Sampling Technique
As this electronic survey had covered all regions of Saudi Arabia, a cluster sampling technique was used to collect the data from 808 participants. The minimum required sample size of 800 was calculated using the level of precision formula by placing the following values N=Z2xpxq/d2xDE, where (z=1.96, P=0.50, q=0.50, d=0.05, design effect=2).
Instrument of Data Collection
A self-prepared questionnaire was used to collect data from the participants. The questionnaire had three sections. Section one contained questions about the demographic data, section two contained questions targeting patients who had been diagnosed with a rheumatic disease, with details of their diagnosis and the time it took for the diagnosis to be confirmed from the onset of symptoms and the symptoms that got them to seek medical attention and the specialties they had visited prior to visiting a rheumatologist, and section three contained questions about the general knowledge of all participants on the role of rheumatologists and the type of symptoms that should prompt a rheumatology consultation.
Data Analysis
The data were entered and analyzed using SPSS 26.0 (v.26.0, IBM Corporation, New York, USA) (RRID:SCR_002865).
Mean and standard deviation were given for quantitative variables. Frequencies and percentages were given for qualitative variables. Knowledge scores were calculated by counting the correct answers, which were then converted to percentage to see whether the participants had poor, good or excellent knowledge. Pearson, chi-squared, Fisher's exact tests were applied to observe associations between qualitative variables.
Results
Sociodemographic Characteristics of the Study Participants
In the present study, 808 patients participated. Mean age of the participants was 34.22 ± 12.77 years. A total of 415 (51.4%) males participated in this study. Majority of the study participants were from Saudi Arabia (N=770, 95.3%). A large number of participants were from Riyadh (N=255, 31.6%), followed by Makkah (N=154, 19.1%), and Al-Qassim (N=74, 9.2%) region. Nearly half of the participants were single (N=387, 47.9%) or married (N=400, 49.5%). Most of the study participants had either diploma or university degree (N=576, 71.3%). With reference to number of children, over half of them had no children (N=412, 51.0%), while nearly one-quarter had more than three children (N=199, 24.6%). Table 1 presents the sociodemographic characteristics of the study participants.
 |
Table 1 Sociodemographic Factors of the Study Participants (N=808) |
Diagnosis and Symptoms Duration of Rheumatic Diseases
Overall, 70 (8.7%) patients had diagnosis of rheumatic disease. Rheumatoid arthritis 40.0% (N=28), followed by osteoarthritis 31.4% (N=22) and gout/pseudogout 11.4% (N=8) were the most common diagnoses. The duration of symptoms before diagnosis were mostly between 1 and 3 months (N=21, 30.1%), followed by <1 month (N=12, 17.1%) and >2 years (N=11, 15.7%). Table 2 represents the overall number and frequency of diagnosis of each rheumatic disease.
 |
Table 2 Descriptive Statistics Regarding Diagnosis and Symptoms Duration of Rheumatic Diseases (N=808) |
Patient Pathway and Diagnostic Journey in Rheumatology Care
Table 3 shows the descriptive statistics for patient pathway and diagnostic journey in rheumatology care. The decision to visit rheumatologist was found to be predominantly based on symptom persistence (N=32, 45.7%) and symptom worsening (N=21, 30.0%). Orthopedic (N=25, 35.7%) was the most frequent clinic specialty that patients visited first based on their symptom dynamics. Visits to nonrheumatologists (N=27, 44.3%) were mostly 1–2 visits. Internet (N=24, 34.3%) and family/friends (N=23, 32.9%) were found to be the main drivers to see a rheumatologist. There was at least one visit (N=27, 38.6%) to a rheumatologist before a firm diagnosis could be made. In most of the patients, duration between symptoms and first diagnosis were <1 month (N=18, 25.7%) or >12 months (N=18, 25.7%). Most of the patients believed that it took longer than expected (N=34, 4.2%) to diagnose their conditions.
 |
Table 3 Patient Pathway and Diagnostic Journey in Rheumatology Care (N=70) |
The study questionnaire also investigated the choice of physician by patients based on their symptoms (Table S1). Majority of the participants responded rheumatologist for joint pain/swelling (N=358, 44.3%), dermatologist for photosensitive rash (N=557, 68.9%), rheumatologist for painful discoloration of finger after cold (N=240, 29.7%), dermatologist for oral and genital ulcers (N=228, 28.2%), and orthopedic for back pain (N=511, 63.2%).
Association Between Demographic and Clinical Factors and Diverse Aspects of Rheumatic Disease
For statements regarding visit to rheumatologist, (Table 4a) shows that the duration between first symptom and rheumatic disease diagnosis is significantly longer for patients aged <50 years compared to that of those with ≥50 years of age (P=0.046). Patients with longer duration of symptoms were likely to have more visits to rheumatologist (P=0.018) (Table 4b). Regarding the factor associated with reasons of delayed diagnosis in patients with rheumatic disease, results show that 36.4% of patients aged ≥50 years had delayed diagnosis due to late appointment compared with 5.7% of patients aged <50 years (Table 4c). For the role of rheumatologist, 31.3% of the participants <50 years of age agreed that rheumatologist treat autoimmune diseases compared to 12.7% in ≥50 years age cohort (P<0.0001) (Table 4d). On the other hand, 28.8% of the ≥50 years age participants responded Yes to statement that rheumatologist treat muscle problems in contrast to 12.5% in <50 years age cohort (P<0.0001) (Table 4e). For the statement that rheumatologists treat elderly knee pain, more participants in group that had no rheumatic disease agreed (43.8% versus 24.3%, P=0.002) compared to their counterparts (Table 4f). Conversely, a large number of patients diagnosed with rheumatic disease responded affirmatively to the statement that rheumatologist treat autoimmune disease (45.7% vs 27.0%, P=0.001) (Table 4g).
 |
Table 4 Association Between Demographic and Clinical Factors and Diverse Aspects of Rheumatic Disease |
Patients’ Statement Regarding First Symptoms, Delayed Diagnosis, Rheumatologists’ Role, and Age Group Affected by Rheumatic Disease
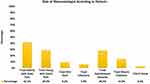
Regarding first symptoms of rheumatic disease (Figure 1), majority of the patients responded Yes to joint pain (N=53, 75.7%), joint swelling (N=33, 47.1%), and morning stiffness (N=23, 32.9%). Waiting for symptoms to appear (N=15, 32.6%) and late referral (N=14, 30.4%) were the main reasons for delayed diagnosis according to patients (Figure 2). The majority of the patients believed that the role of rheumatologist (Figure 3) is to treat knee pain of elderly patients (N=340, 42.1%), followed by young patients with joint pain (N=234, 29.0%) and autoimmune diseases (N=230, 28.5%). Regarding age brackets affected by rheumatic disease (Figure S1), a large number of participants were of the opinion that there is no specific age (N=280, 34.7%), followed by elderly population above 50 years (N=269, 33.3%) and people aged between 35 and 50 years (N=216, 26.7%).
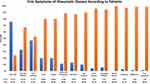 |
Figure 1 First Symptoms in Patients Diagnosed with Rheumatic Disease (N=70). |
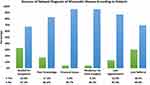 |
Figure 2 Reasons for Delayed Diagnosis of Rheumatic Disease (N=46). |
Discussion
A large population-based study was conducted in Saudi Arabia to evaluate the knowledge of common symptoms of rheumatic diseases and causes of delayed diagnosis. The overall prevalence of rheumatic disease in our cohort was 8.7%, where rheumatoid arthritis, osteoarthritis, and gout/pseudogout were the most common diagnoses. Persistence of symptoms was the predominant cause to visit rheumatologist. The duration between first symptom and rheumatic disease diagnosis is significantly longer for patients aged <50 years compared to that of those with ≥50 years of age. Patients with longer duration of symptoms were likely to have more visits to rheumatologist. Most of the participants of <50 years significantly agreed that rheumatologists treat autoimmune diseases, only a few thought that they treat muscle problems.
We found that the patient sought medical advice when their symptoms worsened. Similarly, a study conducted in Poland, they reported that 89% of patients sought medical care when their symptoms worsened, 86% when they were unable to perform daily activities or work, 70% had limited access to specialists, and more than half of the patients believed their symptoms would resolve on their own.22 The study authors concluded that diagnostic delays are caused by a lack of patient awareness (ignorance of early symptoms) and a dysfunctional health-care system, resulting in delayed consultations with rheumatologists and higher rates of referrals to nonrheumatologists.22
According to our study results, patients with RD usually present with joint pain as their first symptom, followed by joint swelling, morning symptoms and various other symptoms. This is consistent with another recent single center study where half of the patient came with joint pain alone.23 Similarly, a study reported that most of the female patients (84.8%) presented with joint swelling in the onset of RD in Saudi Arabia.13
In our study, most participants have 1–3 months duration of symptoms before they have a diagnosis of rheumatic disease. In Germany, SLE patients were subjected to an additional cross-sectional examination using self-reported questionnaires. Their goal was to establish a connection between this delay and the progression of the disease. According to their findings, the average duration between the onset of symptoms and the diagnosis of SLE was 47 months. The longer the time to diagnosis, the greater the disease activity, disease-related damage, and fatigue, and the lower the health-related quality of life. Unfortunately, a longer diagnostic delay was associated with a worse prognosis.24 Similarly, 822 patients with RA or unclassified arthritis in the UK participated in a questionnaire-based survey. Patients with newly diagnosed rheumatoid arthritis (RA) and unclassified arthritis were investigated for delays between symptom onset and rheumatology evaluation. Only 20% of patients were seen within three months of the onset of symptoms. The median delay for primary care physicians was 6.9 days. Before being referred, patients averaged four visits to the doctor. These findings highlight delays at every stage of the rheumatologist consultation process. Nonetheless, waiting periods for primary care were particularly lengthy.11
A retrospective observational study was conducted in Ontario, Canada, to evaluate referrals to rheumatologists, the early care management of patients with rheumatic diseases, and the timeliness of care and treatment. Among 2,430 patients referred to a rheumatologist with various rheumatic diseases, the time between the onset of symptoms and consultation with a rheumatologist varied by diagnosis, with systemic rheumatic diseases having the shortest time and rheumatoid arthritis (RA) having the longest median time at 327 days. The majority of the delay occurred before referral for 36% of RA patients who started disease-modifying antirheumatic drugs (DMARDs) within six months of symptom onset. In addition to substantial delays in rheumatology consultations, they determined that roughly one-third of rheumatologist referrals were for a systemic inflammatory rheumatic disease.25
We also found that diagnosis of rheumatic disease and duration between first symptoms is significantly associated with age of patients. This is consistent with another study where they also reported that among 102 patients, diagnostic and therapeutic delays were correlated with older age, a lower level of education, and delayed rheumatologist consultation. Anti-CCP antibodies were only associated with a diagnostic delay when rheumatoid factor was negative. Diagnostic and therapeutic delays in patients with rheumatoid arthritis led to high disease activity and poor functional outcomes.26
Similar to our study, another study conducted in Saudi Arabia around a decade prior included patients attending outpatient’s clinic who met the 2010 American College of Rheumatology criteria for RA were the subject of a multicenter, retrospective investigation. They reported the average disease duration was 6.6% in studied patients. At the onset of rheumatoid arthritis, majority of patients reported joint pain. Between the onset of symptoms and their final diagnosis, patients consulted an average of four physicians. The average time between the onset of rheumatoid arthritis and the initial physician visit was 6.2 months, while the average time between the initial physician visit and the final RA diagnosis was 30.2 months. Whereas, in our study the time duration was a maximum of three months. In addition, only 3.2% of patients initially consulted a rheumatologist, compared to 67.2%, 23.6%, and 6.0%, respectively, who consulted orthopedic surgeons, general practitioners, or nonrheumatologists. However, in our study the majority of the participants consulted an orthopedic clinic. In addition, they discovered that rural patients were diagnosed with RA later than urban patients due to geographic distribution and the rarity of rheumatologists in rural areas.13
There are some limitations of the study along with major strength that the study was conducted among the general population of Saudi Arabia to evaluate their knowledge. Although a prior study analyzed the delay of consultation, but they were mostly conducted either in elderly diagnosed patients or in patients who were visiting clinics, which is subject to response bias.
Conclusion
In conclusion, most participants in our study have less knowledge about their symptoms and they did not know where to consult for the treatment of their disease. This caused unnecessary delay and worsening and aggravation of the symptoms. Young patients mostly consulted later compared to elderly patients. There is an increased need to organize an awareness campaign in the general population regarding autoimmune and rheumatic diseases. Likewise, training of general practitioners will also play an important role to optimize access and direct referral to a rheumatologist that will eventually help in early diagnosis and prevention of complications.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Majmaah University for research committee (MUREC) (HA-01-R-088) (with the ethical number MUREC-Aug.30/COM-2022/12-1) for studies involving humans.
Patient Consent for Publication
Informed consent was obtained from all subjects involved in the study for the participation and publication of the study.
Acknowledgments
Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2024R354), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Alsiri N, Alhadhoud M, Alkatefi PTT, Palmer S. The Concomitant Diagnosis of Fibromyalgia and Connective Tissue Disorders: A Systematic Review. Elsevier; 2022.
2. Rome K, Stewart S. 9 - Rheumatic Diseases. In: Burrow JG, Rome K, Padhiar N, editors. Neale’s Disorders of the Foot and Ankle. Oxford: Elsevier; 2020:222–260.
3. Orange DE, Blachere NE, DiCarlo EF, et al. Rheumatoid arthritis morning stiffness is associated with synovial fibrin and neutrophils. Arthr Rheumatol. 2020;72(4):557–564.
4. Sankineni P, Meghana BV. Skin in rheumatoid arthritis and seronegative arthritis. Clin Dermatol Rev. 2019;3(1). doi:10.4103/CDR.CDR_47_18
5. Altorok N, Nada S, Nagaraja V, Kahaleh B. Chapter 17 - Epigenetics in Bone and Joint Disorders. In: Tollefsbol TO, editor. Medical Epigenetics. Boston: Academic Press; 2016:295–314.
6. Deane KD, Demoruelle MK, Kelmenson LB, Kuhn KA, Norris JM, Holers VM. Genetic and environmental risk factors for rheumatoid arthritis. Best Pract Res. 2017;31(1):3–18. doi:10.1016/j.berh.2017.08.003
7. Leu Agelii M, Hafström I, Svensson B, et al. Misdiagnosis of rheumatoid arthritis in a long-term cohort of early arthritis based on the ACR-1987 classification criteria. Open Access Rheumatol. 2022;14:187–194. doi:10.2147/OARRR.S372724
8. Tiwari V, Jandu JS, Bergman MJ. Rheumatoid factor. In: StatPearls. StatPearls Publishing; 2022.
9. Saad SA, Alhaj NK. Delay in referral of rheumatoid arthritis patients to rheumatology clinic. Egypt Rheumatol Rehabil. 2020;47(1):12. doi:10.1186/s43166-020-00012-7
10. Grygiel-Górniak B, Rogacka N, Puszczewicz M. Antinuclear antibodies in healthy people and non-rheumatic diseases - diagnostic and clinical implications. Reumatologia. 2018;56(4):243–248. doi:10.5114/reum.2018.77976
11. Rebecca Jayne S, Peter N, Clare J, et al. Delays between the onset of symptoms and first rheumatology consultation in patients with rheumatoid arthritis in the UK: an observational study. BMJ Open. 2019;9:3.
12. Magliah R, Hafiz W, Alahmadi ZA, et al. Early diagnosis of inflammatory arthritis by primary care physicians following training by a rheumatologist. Open Access Rheumatol. 2019;11:315–321. doi:10.2147/OARRR.S222630
13. Hussain W, Noorwali A, Janoudi N, et al. From symptoms to diagnosis: an observational study of the journey of rheumatoid arthritis patients in Saudi Arabia. Oman Med J. 2016;31:29–34. doi:10.5001/omj.2016.06
14. Janoudi N, Almoallim H, Husien W, Noorwali A, Ibrahim A. Work ability and work disability evaluation in Saudi patients with rheumatoid arthritis. Spec Emph Work Abilit Among Housew Saudi Med J. 2013;34(11):1167–1172.
15. Almoallim H, Janoudi N, Attar SM, et al. Determining early referral criteria for patients with suspected inflammatory arthritis presenting to primary care physicians: a cross-sectional study. Open Access Rheumatol. 2017;9:81–90. doi:10.2147/OARRR.S134780
16. Clinical practice guidelines. Available from: https://rheumatology.org/clinical-practice-guidelines.
17. Aringer M, Brinks R, Dörner T, et al. European League against Rheumatism (EULAR)/American College of Rheumatology (ACR) SLE classification criteria item performance. Ann Rheumatic Dis. 2021;80(6):775–781. doi:10.1136/annrheumdis-2020-219373
18. Medha B, Stephane Z, Ray N, et al. 2023 ACR/EULAR antiphospholipid syndrome classification criteria. Ann Rheumatic Dis. 2023;82(10):1258. doi:10.1136/ard-2023-224609
19. Omair MA, Omair MA, Halabi H. Survey on management strategies of rheumatoid arthritis in Saudi Arabia: a Saudi Society for Rheumatology Initiative. Internat J Rheum Dis. 2017;20(9):1185–1192. doi:10.1111/1756-185X.12735
20. Zaini R, Alrehaily A, Alhazmi A, Halabi H, Mohamed H, Almoallim H. Future directions of rheumatology training according to Saudi vision 2030: recommendations from a Saudi experts meeting. Open Access Rheumatol. 2020;347–355. doi:10.2147/OARRR.S286285
21. Rheumatology SSf. Patient portal 2023. Available from: https://www.ssrsa.org/patients_portal.
22. Raciborski F, Kłak A, Kwiatkowska B, et al. Diagnostic delays in rheumatic diseases with associated arthritis. Rheumatology. 2017;55(4):169–176. doi:10.5114/reum.2017.69777
23. Almoallim H, Hassan R, Cheikh M, et al. Rheumatoid arthritis Saudi database (RASD): disease characteristics and remission rates in a tertiary care center. Open Access Rheumatol;2020. 139–145. doi:10.2147/OARRR.S260426
24. Kernder A, Richter JG, Fischer-Betz R, et al. Delayed diagnosis adversely affects outcome in systemic lupus erythematosus: cross sectional analysis of the LuLa cohort. Lupus. 2021;30(3):431–438. doi:10.1177/0961203320983445
25. Widdifield J, Tu K, Carter Thorne J, et al. Patterns of care among patients referred to rheumatologists in Ontario, Canada. Arthrit Car Res. 2017;69(1):104–114. doi:10.1002/acr.22910
26. Ochola B, Nankabirwa J, Buwembo W, Kaddumukasa M, Mayanja-Kizza H. The clinical presentation and factors associated with disease severity of rheumatoid arthritis in Uganda: a cross-sectional study. Open Access Rheumatol. 2022;14:75–86. doi:10.2147/OARRR.S361454
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.