Back to Journals » Infection and Drug Resistance » Volume 14
Gastrointestinal Tract Colonization Rate of Extended-Spectrum Beta-Lactamase-Producing Gram-Negative Bacteria and Associated Factors Among Orthopaedic Patients in a Tertiary Hospital in Tanzania: Implications for Infection Prevention
Authors Seni J , Akaro IL, Mkinze B, Kashinje Z, Benard M, Mboowa G , Aruhomukama D , Sserwadda I, Joloba ML, Mshana SE , Kidenya BR
Received 26 January 2021
Accepted for publication 25 March 2021
Published 11 May 2021 Volume 2021:14 Pages 1733—1745
DOI https://doi.org/10.2147/IDR.S303860
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Jeremiah Seni,1 Inyasi Lawrence Akaro,2,3 Baraka Mkinze,2,3 Zengo Kashinje,1 Modest Benard,1 Gerald Mboowa,4 Dickson Aruhomukama,4 Ivan Sserwadda,4 Moses L Joloba,4 Stephen E Mshana,1 Benson R Kidenya5
1Department of Microbiology and Immunology, Weill Bugando School of Medicine, Catholic University of Health and Allied Sciences, Mwanza, Tanzania; 2Department of Surgery, Weill Bugando School of Medicine, Catholic University of Health and Allied Sciences, Mwanza, Tanzania; 3Department of Orthopaedic Surgery, Bugando Medical Centre, Mwanza, Tanzania; 4Department of Immunology and Molecular Biology, Makerere University College of Health Sciences, Kampala, Uganda; 5Department of Biochemistry and Molecular Biology, Weill Bugando School of Medicine, Catholic University of Health and Allied Sciences, Mwanza, Tanzania
Correspondence: Jeremiah Seni
Department of Microbiology and Immunology, Weill Bugando School of Medicine, Catholic University of Health and Allied Sciences, P.O. Box 1464, Bugando, Mwanza, Tanzania
Tel: +255 784 593000
Email [email protected]
Background: The dual burden of road traffic accidents and antimicrobial resistance in orthopaedic infections is challenging already strained health-care systems. Limited information exists in Tanzania on antimicrobial resistance surveillance to delineate the potential sources of multi-drug-resistant bacteria for specific mitigation strategies among orthopaedic patients.
Methods: A longitudinal study was conducted at Bugando Medical Centre in Mwanza city between January and May 2020. It involved the collection of rectal swabs/stools, hand swabs, and environmental sampling to identify extended-spectrum beta-lactamase (ESBL)-producing gram-negative bacteria. Participants’ data were collected using a structured questionnaire and analysed to determine factors associated with ESBL colonization among index orthopaedic patients and correlates with other ESBL sources using OR (95% CI) and a cut-off p-value of ≤ 0.05.
Results: We found that 47.2% (125/265) of index patients, 77.8% (14/18) of neighbouring patients, 8.3% (2/24) of health-care workers, 72.2% (13/18) of non-medical caregivers, and 31.4% (27/86) of samples taken from the hospital environment had ESBL producers. Escherichia coli and Klebsiella spp. predominated among participants and Acinetobacter spp. predominated in the environmental samples. Patients with open fractures had increased odds of being colonized with ESBL producers [OR (95% CI): 2.08 (1.16– 3.75); p=0.015]. The floor below patients’ beds was commonly contaminated; however, the odds of environmental contamination decreased on the third round of sampling [OR (95% CI: 0.16 (0.04– 0.67); p=0.012], apparently as a result of parallel infection prevention and control responsive measures against coronavirus disease 2019 (COVID-19).
Conclusion: We found a high occurrence of ESBL colonization among participants and in the environmentat this tertiary hospital. The importance of routine ESBL surveillance among orthopaedic patients with open fractures on admission and strengthened decontamination of health-care premises is reiterated.
Keywords: ESBL colonization, orthopaedic patients, Mwanza, Tanzania
Background
Infections of open fractures are caused by patients’ endogenous normal microbiota and environmental multi-drug-resistant (MDR) bacteria.1,2 These infections are difficult to treat and prone to complications, and therefore, their prevention is pivotal to ensuring favourable patient outcomes.3–5 Preventive and control measures of these infections require a carefully designed infection surveillance system to identify the potential sources of MDR bacteria for specific mitigation strategies.6–8 Owing to limited sanitation and hygiene measures in low- and middle-income countries (LMIC), speculated potential niches are gastrointestinal colonization among patients and environmental contamination. However, the dual burden of road traffic accidents and antimicrobial resistance (AMR) is challenging the already strained health-care systems in LMIC, making prompt responsive action difficult.9–11
In Tanzania, as in many other African countries, over three-quarters of orthopaedic patients’ injuries are due to road traffic accidents. The injuries are mostly open fractures affecting predominantly males in the productive age group between 21 and 30 years.12–14 The proportion of surgical site infections among orthopaedic patients in Tanzania was previously shown to be 6.0%.15 The occurrence and transmission of MDR bacteria [notably methicillin-resistant Staphylococcus aureus (MRSA) and extended-spectrum beta-lactamase (ESBL)-producing bacteria] among patients, health-care workers, and the health-care environment are well documented in general surgery patients.16–18 For example, one study at Bugando Medical Centre (BMC) showed a higher occurrence of ESBL colonization among general surgery patients on discharge compared to admission (36.4% versus 23.7%), and there was a preponderance of exogenous infections.17 Another study showed that approximately one-third of samples taken from the hospital environment were contaminated with Gram-negative bacteria, 20% of which were ESBL producers.18 However, limited information exists among orthopaedic patients, who are thought to be at increased risk owing to the setting where they acquired the injury (ie, mostly in road traffic accidents), which, in turn, challenges specific mitigation strategies. To address these gaps, the current study aimed to evaluate the occurrence of ESBL colonization among orthopaedic patients on admission and also to evaluate other potential sources of ESBL-producing bacteria in the orthopaedic wards (ie, among previously admitted patients on the same wards, non-medical caregivers, health-care workers, and the hospital environment).
Materials and Methods
Study Design, Settings, and Duration
This was a longitudinal study conducted for 4 months from 3rd January to 30th May 2020 at BMC tertiary hospital in Mwanza city, Tanzania. The BMC has a capacity of over 900 beds and serves as a tertiary referral hospital for eight regions in the north-western part of Tanzania, which altogether constitutes a catchment population of over 16 million people.19
Patient Enrolment, Data Collection, and Laboratory Procedures
Purposive sampling was used to recruit appropriate index patients in the orthopaedic wards at BMC (ward J5 for women and children, and ward E8 for males). We included index orthopaedic patients set for admission in the orthopaedic wards whose data and stool/rectal samples had been collected within 24 hours of admission. We excluded patients who had been admitted to the orthopaedic wards but discharged within 24 hours.
To evaluate the occurrence and potential dynamics of transmission of ESBL-producing bacteria, the study also enrolled neighbouring patients (to the index patients) who were already present on the ward at the start of the project and those who were not sampled within 24 hours of admission, the immediate non-medical caregivers of the index patients, and the immediate health workers in the admitting wards, and also examined the patients’ environment in the two wards.
Using the Kish–Leslie equation,20 and a proportion of 23.7% of ESBL Enterobacteriaceae colonization among surgical patients on admission, from another study conducted at the same hospital,17 the minimum sample size for index patients was projected to be 277. A total of 295 eligible patients were enrolled during the study period. However, 12 patients were excluded owing to incomplete information on their questionnaires or because they were discharged within 24 hours. Therefore, a total of 283 patients were enrolled, of whom 265 (93.6%) were index patients and 18 (6.4%) were neighbouring patients.
If an index patient tested positive for ESBL stool/rectal colonization, stool/rectal samples were obtained from the two neighbouring patients flanking the index patient in the same ward and one non-medical caregiver, as well as hand swabs from immediate health-care givers. Index patients who were negative for ESBL colonization on admission were rescreened between 24 and 48 hours (second sampling) and between 72 and 96 hours (third sampling). The environmental sampling in the admitting wards was also carried out three times at intervals of approximately of 2 months: on 16th January 2020 (n=29), 28th March 2020 (n=28), and 28th May 2020 (n=29). Specific environmental areas sampled included walking crutches, wheelchairs, bathroom sinks and door knobs, the floor below patients’ beds, and patients’ bed rails. Based on this sampling strategy, we enrolled 18 non-medical caregivers, 24 health-care workers, and 88 environmental samples from the wards.
Research assistants, nurses, and doctors in each ward instructed index patients, neighbouring patients, and non-medical caregivers to collect stool/rectal samples using sterile swabs. Hand swabs were collected from health workers by gently rolling the swab on the palm and between the fingers of both hands. Environmental sampling was conducted by swabbing the site using a sterile swab. All swabs collected were labelled immediately, placed in Amies transport medium (Amies Swabs PS + Viscose; DeltaLab, Barcelona, Spain) and submitted to the Catholic University of Health and Allied Sciences (CUHAS) Multipurpose Laboratory within 2 hours for subsequent processing.
In the laboratory, samples were inoculated on MacConkey agar, a selective and differential culture medium (Oxoid, Basingstoke, UK), supplemented with 2 μg/mL cefotaxime (a third generation cephalosporin), and incubated in ambient air at 35–37°C for 18–24 hours for screening of presumptive ESBL-producing Gram-negative bacteria.21 Following incubation, any growth was presumptively regarded as cephalosporin-resistant Gram-negative bacteria. Then, pure colonies were initially identified phenotypically based on Gram staining reactions and lactose fermentation, followed by confirmation of bacterial genera and/or species using five biochemical identification tests, namely oxidase, urease, Simmons citrate, sulphur-indole-motility, and triple sugar iron tests (Oxoid, Basingstoke, UK), as previously described and validated in house.21,22 Finally, antimicrobial susceptibility testing (AST) was performed using the conventional Kirby–Bauer disc diffusion method as per Clinical and Laboratory Standards Institute (CLSI) guidelines.23 The standardized inoculum was made by emulsifying one or two pure bacterial colonies in normal saline and adjusting the turbidity of the resulting suspension to a 0.5 McFarland standard. Using a sterile cotton swab, the suspension was uniformly spread into two Mueller–Hinton agar plates (Oxoid, Basingstoke, UK). Then, 11 antibiotic discs (Oxoid, Basingstoke, UK) were placed in the plates, incubated in ambient air at 35–37°C for 18–24 hours, and subsequently interpreted as sensitive, intermediate, or resistant, as per CLSI guidelines.23 The non-beta-lactam antibiotic discs set were tetracycline (10 µg), trimethoprim–sulfamethoxazole (1.25/23.75 µg), chloramphenicol (10 µg), gentamicin (10 µg), ciprofloxacin (5 µg), and amikacin (30 µg). In addition, four antibiotic discs were set up for special purposes as described below: cefoxitin (30 µg) for presumptive screening of AmpC production, a fourth generation cephalosporin cefepime (30 µg), the broad-spectrum beta-lactam/beta-lactamase inhibitor piperacillin–tazobactam (TZP) (100/10 µg), and the last line beta-lactam antibiotic meropenem (10 µg).23 ESBL production was confirmed by the combined disc method, as previously described for Enterobacteriaceae and with slight modification for non-Enterobacteriaceae Gram-negative bacteria.23
Quality Control
Information in the questionnaires was reviewed by two research scientists (ZK and MB) for completeness at the end of each day. The investigators reviewed the data in the questionnaires on a weekly basis. All laboratory procedures were carried out by laboratory scientists under the supervision of medical microbiologists. Sterility testing was performed by incubating uninoculated MacConkey agar plates for each batch of freshly prepared media, and when no growth of bacteria was observed after overnight incubation, the batch was regarded as good for use in subsequent laboratory procedures. Two standard control strains (Klebsiella pneumoniae ATCC 700603 and Escherichia coli ATCC 25922) were used to assess the performance of MacConkey agar media supplemented with 2 μg/mL cefotaxime by showing typical growth of lactose-fermenting colonies and no bacterial growth, respectively. These two strains were also used as controls to assess the biochemical identification tests, for AST procedures, and for confirmation of ESBL strains.
Data Management and Statistical Analysis
Socio-demographic, clinical, and laboratory data from study participants and environmental samples were entered into Microsoft Excel for storage and consistency checks, and exported to STATA version 13.0 for analysis. Continuous variables such as age and frequency of antibiotic use were described using measures of central tendency, ie, mean ± standard deviation and median (interquartile range) for symmetrically and asymmetrically distributed data, respectively. All other categorical variables were described by frequencies and their respective percentages/proportions and compared using the Pearson chi-squared or Fisher’s exact test, or the two-sample test of proportions. The strength of the association between the dependent variable (ESBL colonization by Gram-negative bacteria) and independent variables (eg, age, sex, residence, ward of admission, and history of antibiotic use) was determined using a logistic regression model. All variables with a p-value of ≤0.2 in univariate analysis were subjected to multivariate analysis to determine the independent predictors of ESBL positivity at a p-value of ≤0.05 with a 95% confidence interval (CI).
Results
Socio-Demographic and Clinical Characteristics of Index Orthopaedic Patients
Of the 265 index patients enrolled, approximately two-thirds were males, and the overall median (IQR) age was 28 (12–41) years (Table 1). The majority of patients were admitted from other hospitals/clinics (66.8%) and had closed fractures (69.4%). Of 167 patients for whom information was available, only 48 (28.7%) had attended a hospital within 24 hours. A total of 101 (38.1%) were on antibiotic treatment at the time of enrolment. Of these, 72 (71.3%) were on beta-lactam antibiotics, with ceftriaxone alone being prescribed in 60 patients, 15 (14.8%) were on non-beta-lactam antibiotics, and 14 (13.9%) were on both beta-lactam and non-beta-lactam antibiotics. A total of 131 (49.4%) reported self-treatment with antibiotics in the past year. The median (IQR) frequency of self-treatment was 4 (2–5). The minimum and maximum frequencies of self-treatment were 1 and 20, respectively (Table 1).
 |
Table 1 Socio-Demographic and Clinical Characteristics of Index Orthopaedic Patients |
ESBL-Producing Gram-Negative Bacteria Among Index and Neighbouring Orthopaedic Patients
The prevalence of ESBL-producing Gram-negative bacterial colonization among all orthopaedic patients was 49.1% (139/283) (95% CI: 45.0–56.7%). ESBL colonization was significantly higher among neighbours [77.8% (14/18)] than index patients [47.2% (125/265)], p=0.011 (one-sided Fisher’s exact test). ESBL colonization rates among tested index patients on admission, second sampling, and third sampling, were 47.2%, 16.7%, and 0.0%, respectively.
A total of 158 ESBL-producing Gram-negative bacteria were recovered (142 from index orthopaedic patients and 16 from neighbouring patients), with a predominance of E. coli (53.8%), which accounted for 52.1% of isolates from index patients and 68.8% of isolates from neighbours (Figure 1).
Antimicrobial Susceptibility Patterns of ESBL-Producing Gram-Negative Bacteria Isolates
The highest sensitivity patterns of ESBL-producing E. coli were noted in isolates from both index and neighbouring patients in chloramphenicol (85.1% versus 81.8%), piperacillin–tazobactam (73.0% versus 63.6%), amikacin (97.3% versus 100.0%), and meropenem (97.2% versus 100.0%), respectively. Similarly, there were also high sensitivities of these antibiotics to other Gram-negative bacteria (Table 2).
 |
Table 2 Antimicrobial Susceptibility Patterns of ESBL-Producing Gram-Negative Bacteria Isolates |
Factors Associated with Gastrointestinal Tract ESBL Colonization Among Index Orthopaedic Patients
The multivariate logistic regression analysis showed that index patients with open fractures had increased odds of being of colonized with ESBL-producing Gram-negative bacteria [OR (95% CI): 2.08 (1.16–3.75); p=0.015] (Table 3).
 |
Table 3 Factors Associated with Gastrointestinal Tract ESBL Colonization Among Index Orthopaedic Patients |
ESBL Colonization Among Patients’ Caregivers and Health-Care Workers in Orthopaedic Wards
A total of 18 patients’ caregivers were enrolled in this study, 16 (88.9%) of whom were female. Their mean ± SD age was 33.6±10.4 years. All caregivers had a previous history of antibiotic use and half of them had previously self-treated with antibiotics. The prevalence of ESBL rectal colonization was 72.2% (13/18). The implicated ESBL isolates were E. coli (n=6), K. pneumoniae (n=6), and unidentified Gram-negative bacteria (n=1).
A total of 24 health-care workers were enrolled during the study period, half of whom were female. Three-quarters worked on the E8 male ward. Their mean ± SD age was 33.2±9.4 years, and their duration of working in their respective wards/units ranged from 1 month to 10 years. The majority were nurses (58.4%), whereas doctors and medical attendants accounted for 20.8% each. Three health-care workers (12.5%) had a history of using antibiotics in the past 3 months (one each had used ampiclox, amoxicillin–clavulanate, and ceftriaxone). The prevalence of ESBL hand colonization was 8.3% (2/24). One health-care worker (a doctor with a history of using amoxicillin–clavulanate, in ward E8) had dual carriage of K. pneumoniae and E. coli. The former isolate was resistant to trimethoprim–sulfamethoxazole, chloramphenicol, and ciprofloxacin; showed intermediate resistance to gentamicin and piperacillin–tazobactam; and was sensitive to tetracycline, amikacin, and meropenem. The latter isolate was resistant to tetracycline, trimethoprim–sulfamethoxazole, chloramphenicol, ciprofloxacin, and piperacillin–tazobactam; showed intermediate resistance to gentamicin; and was sensitive to amikacin and meropenem. The second health-care worker (a nurse with no history of antibiotic use, in ward E8) had K. pneumoniae only. This isolate was resistant to trimethoprim–sulfamethoxazole, chloramphenicol, and gentamicin; showed intermediate resistance to ciprofloxacin; and was sensitive to tetracycline, piperacillin–tazobactam, amikacin, and meropenem
There were 11 pairs of index patient–neighbour, and five pairs had ESBL-producing bacteria of the same species but different strains (Supplementary Table S1). There were 13 pairs of index patients and caregivers, but only 11 pairs were involved in the comparison. (One pair was dropped because the neighbour was sampled instead of the index patient and the second was dropped because a caregiver was linked to an index patient with no ESBL colonization.) Of the 11 pairs, three pairs had ESBL-producing bacteria of the same species but different strains (Supplementary Table S2).
Distribution of ESBL-Producing Bacterial Isolates in the Environment of the Wards
The proportion of ESBL-producing bacteria isolated from the environment of the wards was 31.4% (27/86), which altogether resulted into 35 bacterial isolates. The most predominant bacteria were Acinetobacter spp. (50.0%), followed by K. pneumoniae (n=6), Enterobacter spp. (n=5), E. coli (n=4), unidentified Gram-negative bacteria (n=2), and Citrobacter spp. (n=1). The odds of occurrence of ESBL-producing Gram-negative bacteria was significantly higher from the floor samples [OR (95% CI): 10.0 (1.09–92.0); p=0.042] compared to other environmental samples. However, the odds of occurrence of ESBL-producing Gram-negative bacteria significantly decreased on the third round of sampling [OR (95% CI): 0.16 (0.04–0.67); p=0.012] (Table 4).
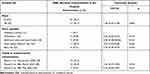 |
Table 4 Factors Associated with Occurrence of ESBL Bacteria in the Hospital Environment |
Discussion
Existence of ESBL-Producing Bacteria Among Study Participants and the Hospital Environment
Prevention of MDR bacterial attributable infections is a pivotal measure to avert the burden of AMR across the world and is one of the strategic objectives in the Global Action Plan on AMR and the Tanzanian National Action Plan on AMR.24,25 We found a significantly lower proportion of ESBL stool/rectal colonization among index orthopaedic patients (47.2%) on admission compared to neighbouring orthopaedic patients who had previously been admitted in the orthopaedic wards (77.8%). The former proportion is higher than 23.7% in the same hospital among general surgical patients on admission and 16.5% in the general population in communities around Mwanza city.17,26 This higher proportion could be related to the fact that nearly two-thirds of patients had been referred from other hospitals/clinics, and therefore could represent the trend in the hospital settings, as shown among neighbouring patients who had spent longer on the wards (77.8%). The occurrence of ESBL-producing bacteria in the hospital environment in this study (31.4%) was similar to that in a previous study among patients on discharge (36.4%).17 In contrast to our findings, which showed colonization of 16% 48 hours after admission, a low prevalence of ESBL rectal colonization on admission and at 48 hours post-admission (6.0% and 9.0%, respectively) was previously reported from Denmark.27 Stringent infection prevention and control (IPC) measures may account for the lower colonization rates 48 hours post-admission in both countries, and this is especially important in Tanzania as the current study was conducted in the midst of the coronavirus disease 2019 (COVID-19) pandemic, where IPC was largely strengthened. ESBL hand contamination among health-care workers in the orthopaedic wards was lower (8.3%), and similar to 10.7% among health-care workers in a cardiac intensive care unit in Kampala, Uganda.28
The predominance of ESBL-producing E. coli and Klebsiella spp. among orthopaedic patients, non-medical caregivers, and health-care workers in this study is in agreement with two systematic reviews and meta-analyses among patients with various infections in East African hospitals, animals, and non-hospital environments,6,11 and another study among general and orthopaedic patients in Denmark.27 On the other hand, the predominance of Acinetobacter spp. in the hospital environment underscores its natural existence on inanimate surfaces in the hospital. The presence of these three MDR pathogens calls for the establishment of targeted AMR surveillance systems, focused IPC mitigation strategies, and the introduction of cost-effective molecular tools for their routine screening in hospital settings. Hand in hand with these responsive measures, the exploration of non-antibiotic remedies such as essential oils would be of interest in these settings, where the burden of MDR-attributable infection is rapidly escalating.29
Antimicrobial Susceptibility Profiles of ESBL-Producing Bacteria
Over three-quarters of ESBL-producing bacterial isolates were sensitive to the WHO watch and reserve group of antibiotics, including chloramphenicol, piperacillin–tazobactam, amikacin, and meropenem. This may be due to the fact that these antibiotics are very expensive and not accessible in most of the drug outlets/pharmacies, and therefore less likely to be misused, as previously shown in six referral hospitals across Tanzania.30,31 Therefore, rational use of these agents guided by AST is emphasized to ensure their longevity in saving patients’ lives.
Factors Associated with Occurrence of ESBL-Producing Bacteria Among Participants and the Hospital Environment
Previous studies have shown a strong association between previous antibiotic use and previous hospital admission with subsequent ESBL colonization and/or infections, both in Tanzania and in other countries.14,26,27,32 However, this was not the case in the current study.
Index patients with open fractures had approximately two times increased odds of being of colonized with ESBL-producing Gram-negative bacteria compared to their counterparts. This may be due to the fact that patients with open fractures are at increased risk of infections and complications, and therefore, are likely to be given antibiotic prophylaxis and to stay longer in the hospital, all of which will increase their risk of being colonized and sometimes infected with MDR bacteria, including ESBL-producing Gram-negative bacteria.5
Of the 11 pairs of index patient–neighbour and 11 pairs of index patient–caregiver, five and three pairs, respectively, had ESBL-producing bacteria of the same species but different strains. None of these strains had exactly identical antibiogram profiles, making the transfer of AMR genes by clonal expansion less likely, and leaving open the possibility of horizontal transfer of AMR genes within and among bacterial species.33 The latter will be further dissected in the next phase of the project using the whole genome sequencing approach. At this juncture, it suffices to point out that the occurrence of ESBL-producing bacteria among orthopaedic patients, non-medical caregivers, health-care workers, and the hospital environment should alert the hospital to be more vigilant in IPC and prevent subsequent infections in vulnerable orthopaedic patients.
The odds of occurrence of ESBL-producing Gram-negative bacteria was higher from shared locations and items in the hospital environment (eg, floor samples, wheelchairs, sinks, doors knobs, and bed rails), ranging from 27.3% to 50.0%, compared to personal items (eg, walking crutches: 9.1%). Hospital environmental contamination has previously been widely documented to provide potential niches for MDR bacteria,18,34 underscoring a need to frequently decontaminate these premises. Our study was conducted in the midst of the COVID-19 pandemic, and a trend towards a decrease in ESBL-producing bacteria contaminating the hospital environment was noted (ie, there was a 16-fold decrease by the third round of sampling). The decrease could be associated with the parallel hospital-wide vigilant strengthening of IPC measures against severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) and COVID-19, which indirectly also decreased these MDR bacteria in the hospital environment.
Limitations of the Study
This project commenced when the world (including Tanzania) was in the midst of the COVID-19 pandemic. This negatively impacted our project as there only limited routine elective orthopaedic surgery was carried out and non-medical caregivers were limited to those attending clinically unstable patients. So, we ended up enrolling only a few caregivers and neighbouring patients. The duration of hospital stay among index orthopaedic patients was also reduced for those who were clinically stable, and as a result, the follow-up component was also negatively affected. However, despite all these limitations, the study objectives were largely achieved.
Conclusions
Significant proportions of orthopaedic patients, healthy individuals on the orthopaedic wards, and locations in the hospital environment had ESBL-producing Gram-negative bacteria. There was a predominance of E. coli and Klebsiella spp. among participants, and Acinetobacter spp. in the environmental samples. Patients with open fractures had increased odds of being colonized with ESBL producers, emphasizing a need to prioritize this group in the AMR routine surveillance programmes. The most commonly contaminated environmental location was the floor below patients’ beds. However, there was an appreciable trend towards a decrease in environmental contamination, notably in the third round of sampling, which could be linked to parallel responsive IPC measures against COVID-19. This reinforces the need to strengthen the routine decontamination of the health-care environment.
Extending AMR surveillance to the lower tier hospitals where two-thirds of orthopaedic patients came from, and evaluating the impact of ESBL colonization on the incident orthopaedic patients’ infections, should be areas of focus in future studies.
Disclaimer
The contents are the responsibility of the authors and do not necessarily reflect the views of the funders.
Abbreviations
AMR, antimicrobial resistance; AST, antimicrobial susceptibility testing; ATCC, American Type Culture Collection; BMC, Bugando Medical Centre; CLSI, Clinical and Laboratory Standards Institute; CUHAS, Catholic University of Health and Allied Sciences; ESBL, extended-spectrum beta-lactamase; IPC, infection prevention and control; IQR, interquartile range; LMIC, low- and middle-income countries; MDR, multi-drug resistance; SD, standard deviation.s
Data Sharing Statement
The data supporting the findings of this study are available from the corresponding author upon reasonable request. Additional data from this study will be published by the co-authors.
Ethics Approval and Informed Consent
This study was conducted in accordance with the Declaration of Helsinki. It was approved by the Joint CUHAS/BMC Research and Ethics Committee (CREC/409/2019) and the National Health Research Ethics Review Committee of the National Institute for Medical Research (NIMR/HQ/R.8a/Vol. IX/3322) in Tanzania; and the Makerere University College of Health Sciences – School of Biomedical Sciences Higher Degrees Research and Ethics Committee (SBS-HDREC-650) and the Uganda National Council for Science and Technology (HS411) in Uganda. Permission to conduct this study was sought from the BMC Director General, Head of the Department of Orthopaedics, and the ward supervisors/in-charge nurses prior to sample and data collection. Written informed consent for adults (or assent for children) was obtained from all study participants. Patients received all necessary urgent management prior to being enrolled into the study. All information obtained from all study participants was kept confidential using codes. In the event that a patient developed surgical site infection, appropriate samples were taken for culture and antimicrobial susceptibility testing to guide attending doctors on the specific antimicrobial therapies.
Acknowledgments
We are thankful to the study participants for their involvement in this study, and to the BMC and CUHAS management for their support during execution of this study. We are grateful to the research assistants (Scholastica S. Bupaha, Frank Rwihula, Janeth S. Danga, Pendo E. Haraka, Emmanuel S. Elikana, and Geoffrey Luena) for their excellent technical assistance. We are also thankful to all doctors, nurses, and medical attendants in the orthopaedic wards for managing the patients and their general involvement in the study.
Author Contributions
JS, GM, DA, IS, MJ, SEM, and BRK made substantial contributions to the conception, designing, coordination and execution of the study; JS, ILA, BM, ZK, and MB made substantial contributions to the acquisition of data and clinical samples, and played critical roles in the patients’ management; JS, ILA, BM, ZK, MB, SEM, and BRK made substantial contributions to the analyses of data and clinical samples, and performed extensive literature searches and interpretation of data; JS wrote the initial draft of the manuscript, which was critically revised by all authors. All authors contributed to data analysis, drafting, or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This study was part of the research project titled “Understanding transmission dynamics and acquisition of antimicrobial resistance at referral hospitals and community settings in East Africa”, supported through the Grand Challenges Africa programme (grant numbers GCA/AMR/rnd2/058/002 and GCA/AMR/rnd2/058-01). Grand Challenges Africa is a programme of the African Academy of Sciences (AAS) implemented through the Alliance for Accelerating Excellence in Science in Africa (AESA) platform, an initiative of the AAS and the African Union Development Agency (AUDA-NEPAD). GC Africa is supported by the Bill and Melinda Gates Foundation (BMGF) and the African Academy of Sciences and partners. It was executed collaboratively between Makerere University College of Health Sciences, Kampala, Uganda, and the Catholic University of Health and Allied Sciences, Mwanza, Tanzania. The funders had no roles in the design, execution, data management, manuscript writing, or manuscript submission.
Disclosure
The authors reported no conflicts of interest for this work.
References
1. Seekamp A, Köntopp H, Schandelmaier P, Krettek C, Tscherne H. Bacterial cultures and bacterial infection in open fractures. Eur J Trauma. 2000;26(3):131–138. doi:10.1007/s000680050011
2. Penn-Barwell JG, Bennett PM, Mortiboy DE, Fries CA, Groom AF, Sargeant ID. Factors influencing infection in 10 years of battlefield open tibia fractures. Strategies Trauma Limb Reconstr. 2016;11(1):13–18. doi:10.1007/s11751-016-0250-x
3. Court-Brown CM, Bugler KE, Clement ND, Duckworth AD, McQueen MM. The epidemiology of open fractures in adults. A 15-year review. Injury. 2012;43(6):891–897. doi:10.1016/j.injury.2011.12.007
4. Elniel AR, Giannoudis PV. Open fractures of the lower extremity. EFORT Open Rev. 2018;3(5):316–325. doi:10.1302/2058-5241.3.170072
5. Hannigan GD, Pulos N, Grice EA, Mehta S. Current concepts and ongoing research in the prevention and treatment of open fracture infections. Adv Wound Care. 2015;4(1):59–74. doi:10.1089/wound.2014.0531
6. Seni J, Moremi N, Matee M, et al. Preliminary insights into the occurrence of similar clones of extended-spectrum beta-lactamase-producing bacteria in humans, animals and the environment in Tanzania: a systematic review and meta-analysis between 2005 and 2016. Zoonoses Public Health. 2018;65(1):1–10. doi:10.1111/zph.12387
7. World Health Organization. Antimicrobial resistance: global report on surveillance. June 2014 ed. Geneva, Switzerland: World Heath Organization; 2014.
8. Metsemakers WJ, Onsea J, Neutjens E, et al. Prevention of fracture-related infection: a multidisciplinary care package. Int Orthop. 2017;41(12):2457–2469. doi:10.1007/s00264-017-3607-y
9. O’Neill J Review on antimicrobial resistance. antimicrobial resistance: tackling a crisis for the health and wealth of nations; December 2014.
10. Bonnet E, Lechat L, Ridde V. What interventions are required to reduce road traffic injuries in Africa? A scoping review of the literature. PLoS One. 2018;13(11):e0208195. doi:10.1371/journal.pone.0208195
11. Sonda T, Kumburu H, van Zwetselaar M, et al. Meta-analysis of proportion estimates of extended-spectrum-beta-lactamase-producing Enterobacteriaceae in East Africa hospitals. Antimicrob Resist Infect Control. 2016;5(1):18. doi:10.1186/s13756-016-0117-4
12. Clelland SJ, Chauhan P, Mandari FN. The epidemiology and management of tibia and fibula fractures at Kilimanjaro Christian Medical Centre (KCMC) in Northern Tanzania. Pan Afr Med J. 2016;25:51. doi:10.11604/pamj.2016.25.51.10612
13. Haonga BT, Areu MMM, Challa ST, et al. Early treatment of open diaphyseal tibia fracture with intramedullary nail versus external fixator in Tanzania: cost effectiveness analysis using preliminary data from Muhimbili Orthopaedic Institute. Sicot-J. 2019;5:20. doi:10.1051/sicotj/2019022
14. Idowu OJ, Onipede AO, Orimolade AE, Akinyoola LA, Babalola GO. Extended-spectrum beta-lactamase orthopedic wound infections in Nigeria. J Glob Infect Dis. 2011;3(3):211–215. doi:10.4103/0974-777X.83524
15. Nobert N, Moremi N, Seni J, et al. The effect of early versus delayed surgical debridement on the outcome of open long bone fractures at Bugando Medical Centre, Mwanza, Tanzania. J Trauma Manag Outcomes. 2016;10(1):6. doi:10.1186/s13032-016-0036-7
16. Moremi N, Claus H, Vogel U, Mshana SE. The role of patients and healthcare workers Staphylococcus aureus nasal colonization in occurrence of surgical site infection among patients admitted in two centers in Tanzania. Antimicrob Resist Infect Control. 2019;8(1):102. doi:10.1186/s13756-019-0554-y
17. Moremi N, Claus H, Rutta L, Frosch M, Vogel U, Mshana SE. High carriage rate of extended-spectrum beta-lactamase-producing Enterobacteriaceae among patients admitted for surgery in Tanzanian hospitals with low rate of endogenous surgical site infections. J Hosp Infect. 2018;100(1):47–53. doi:10.1016/j.jhin.2018.05.017
18. Moremi N, Claus H, Silago V, et al. Hospital surface contamination with antimicrobial-resistant Gram-negative organisms in Tanzanian regional and tertiary hospitals: the need to improve environmental cleaning. J Hosp Infect. 2019;102(1):98–100. doi:10.1016/j.jhin.2018.09.001
19. URT. The 2012 population and housing census. Gender dimension monograph. Vol. IV. The United Republic of Tanzania (URT); 2015. Available from: https://www.nbs.go.tz/index.php/en/census-surveys/population-and-housing-census/177-2012-phc-gender-dimension-monograph .
20. Kish L. Sampling organizations and groups of unequal sizes. Am Sociol Rev. 1965;30(4):564–572. doi:10.2307/2091346
21. Nelson E, Kayega J, Seni J, et al. Evaluation of existence and transmission of extended spectrum beta lactamase producing bacteria from post-delivery women to neonates at Bugando Medical Center, Mwanza-Tanzania. BMC Res Notes. 2014;7(1):279. doi:10.1186/1756-0500-7-279
22. Koneman EW, Allen SD, Janda WM, Schreckenberger PC, Winn WC. Color Atlas and Textbook of Diagnostic Microbiology.
23. CLSI. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing.
24. World Health Organization. Global action plan on antimicrobial resistance. The World Health Organization, Geneva, Switzerland; 2015. Available from: http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_20-en.pdf?ua=1.
25. URT. The National Action Plan on Antimicrobial Resistance (2017–2022). The Ministry of Health Community Development Gender Elderly and Children (MHCDGEC), Ministry of Agriculture, Livestock and Fisheries (MALF). The United Republic of Tanzania (URT); 2017.
26. Mshana SE, Falgenhauer L, Mirambo MM, et al. Predictors of blaCTX-M-15 in varieties of Escherichia coli genotypes from humans in community settings in Mwanza, Tanzania. BMC Infect Dis. 2016;16(1):187. doi:10.1186/s12879-016-1527-x
27. Jakobsen L, Kuhn KG, Hansen F, et al. Fecal carriage of extended-spectrum and AmpC beta-lactamase-producing Enterobacteriaceae in surgical patients before and after antibiotic prophylaxis. Diagn Microbiol Infect Dis. 2016;86(3):316–321. doi:10.1016/j.diagmicrobio.2016.07.028
28. Ssemogerere L, Sendagire C, Mbabazi C, et al. Hand colonization with gram-negative organisms of healthcare workers accessing the cardiac intensive care unit: a cross-sectional study at the uganda heart institute. Crit Care Res Pract. 2019;2019:6081954. doi:10.1155/2019/6081954
29. Donadu MG, Trong Le N, Viet D, et al. Phytochemical compositions and biological activities of essential oils from the leaves, rhizomes and whole plant of hornstedtia bella skornick. Antibiotics (Basel). 2020;9(6).
30. Seni J, Mapunjo SG, Wittenauer R, et al. Antimicrobial use across six referral hospitals in Tanzania: a point prevalence survey. BMJ Open. 2020;10(12):e042819. doi:10.1136/bmjopen-2020-042819
31. World Health Organization. The 2019 WHO AWaRe classification of antibiotics for evaluation and monitoring of use. World Health Organization; 2019. Available from: https://apps.who.int/iris/handle/10665/327957.
32. Marando R, Seni J, Mirambo MM, et al. Predictors of the extended-spectrum-beta lactamases producing Enterobacteriaceae neonatal sepsis at a tertiary hospital, Tanzania. Int J Med Microbiol. 2018;308(7):803–811. doi:10.1016/j.ijmm.2018.06.012
33. Andersson DI, Hughes D. Antibiotic resistance and its cost: is it possible to reverse resistance? Nat Rev Microbiol. 2010;8(4):260–271. doi:10.1038/nrmicro2319
34. Mitchell BG, Dancer SJ, Anderson M, Dehn E. Risk of organism acquisition from prior room occupants: a systematic review and meta-analysis. J Hosp Infect. 2015;91(3):211–217. doi:10.1016/j.jhin.2015.08.005
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

