Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
Fried Frailty Phenotype in Elderly Patients with Chronic Coronary Syndrome: Prevalence, Associated Factors, and Impact on Hospitalization
Authors Nguyen HT , Do HT, Nguyen HVB, Nguyen TV
Received 29 November 2023
Accepted for publication 14 March 2024
Published 20 March 2024 Volume 2024:17 Pages 1265—1274
DOI https://doi.org/10.2147/JMDH.S452462
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Huan Thanh Nguyen,1,2 Huong Thanh Do,2 Hai Van Be Nguyen,2 Tan Van Nguyen1,3
1Department of Geriatrics and Gerontology, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam; 2Department of Cardiology, Thong Nhat Hospital, Ho Chi Minh City, Vietnam; 3Department of Interventional Cardiology, Thong Nhat Hospital, Ho Chi Minh City, Vietnam
Correspondence: Huan Thanh Nguyen, Department of Geriatrics and Gerontology University of Medicine and Pharmacy at Ho Chi Minh City, 17 Hong Bang Street, Ward 11, District 5, Ho Chi Minh City, Vietnam, Tel +84-909097849, Email [email protected]
Purpose: To investigate the prevalence and factors associated with frailty and impact of frailty on hospitalization due to any cause in elderly patients with chronic coronary syndrome (CCS).
Patients and Methods: We conducted a study wherein we assessed frailty using Fried frailty phenotype for outpatients aged ≥ 60 years with CCS. Logistic regression analysis was performed to assess the factors associated with frailty. Frailty was adjusted for demographic and geriatric variables and comorbidities to assess its impact on hospitalization.
Results: Overall, 420 patients (median age 70 years [interquartile range, 65– 77]; men, 74.5%) who completed the 3-month follow-up period were analyzed. Coronary revascularization for > 1 year was the most common clinical scenario for CCS (59.8%; n = 251). The prevalence of non-frail, pre-frail, and frail patients were 22.4% (n = 94), 49.7% (n = 209), and 27.9% (n = 117), respectively. In the adjusted model, three factors associated with frailty were age ≥ 75 years (odds ratio [OR] 2.29, 95% confidence interval [CI] 1.39– 3.75, P = 0.001), limitations in instrumental activity of daily living (OR 3.89, 95% CI 2.33– 6.48, P < 0.001), and heart failure (OR 2.30, 95% CI 1.32– 4.02, P = 0.003). The overall 3-month hospitalization rate was higher in frail patients than in non-frail patients (23.9% vs 13.5%, P = 0.012). Frailty was associated with hospitalization (OR 1.85, 95% CI 1.04– 3.30, P = 0.037) but in a weak strength of association (r = 0.126).
Conclusion: The prevalence of frailty was 27.9% in the elderly patients with CCS. Age ≥ 75 years, limitations in functional status, and heart failure were associated with increased odds of frailty. Frailty was a predictor of 3-month all-cause hospitalization in these patients.
Keywords: frailty, chronic coronary syndrome, elderly
Introduction
Coronary artery disease (CAD) has increased prevalence and incidence with age.1 Although it remains one of the most medical life-threatening condition for the elderly, especially in acute atherothrombotic events called acute coronary syndromes (ACS),2 most patients have stable periods presenting various clinical scenarios called chronic coronary syndromes (CCS).3 Fortunately, CAD can in fact be prevented and controlled by lifestyle changes, pharmacologic therapy, and revascularization procedures to stabilize and regress the process of coronary atherosclerotic plaque.3 However, the challenge is that the elderly with CAD may concurrently have geriatric issues, such as polypharmacy, multimorbidity, declines in physical and mental health, and frailty, which may influence prognosis and management of CAD.4
Frailty is considered a clinical condition of increased and disproportionate vulnerability resulting from a decreased ability to recover homeostasis following stressor events due to age-related multisystem failure and pathological decline in reserves.5 About one quarter of the elderly worldwide are frail,6 and they have a higher risk of disability, hospitalization, and death. In the adverse events, the elderly who hospitalized due to frailty place a considerable pressure on health care systems, their relative caregivers, and themselves.7 Among several frailty screening and assessment tools,8 the Fried frailty phenotype can categorize elderly into non-frail, pre-frail, or frail, and has association with cardiovascular outcomes.9,10
Given that both CAD and frailty are linked to the aging process and share some common pathophysiological pathways, frailty may thoroughly influence CAD expression, whereas CAD may accelerate the development of frailty.11 However, although many studies have evaluated the impact of frailty on adverse health outcomes in elderly patients with ACS,12 little clinical information is available to understand the burden and prognostic value of frailty in elderly patients with CCS.13 Therefore, the primary aim of this study was to investigate the prevalence of frailty assessed by the Fried frailty phenotype in elderly outpatients with CCS. The two secondary aims of this study were to identify the factors associated with frailty and evaluate the impact of frailty on hospitalization in these patients.
Material and Methods
Study Design, Participants, and Data Collection
Between May 2023 and October 2023, this prospective observational study was conducted in patients aged ≥ 60 years with a diagnosis of chronic coronary syndromes (CCS) visiting the Cardiology clinics at Thong Nhat hospital, Ho Chi Minh city, Vietnam. The investigators collected sociodemographic characteristics, medical histories, and CCS scenarios from electronic medical records and face-to-face interviews. After 3 months, we made telephone calls to the patients or their family members. Hospitalization was established as a binary variable if the patient had been hospitalized for any cause at least once during the 3-month follow-up period. Hospital electronic medical records were used to confirm hospitalization. The exclusion criteria include active malignancy, serious mental condition, no response to follow-up calls, and unconfirmed hospitalization events. Written informed consent was obtained from all the patients. This study complied with the ethical principles of the Declaration of Helsinki. This study was approved by the Ethics Committee of Thong Nhat hospital (reference number: 34/BVTN-ĐHYD).
Assessment of Frailty
Patients were diagnosed as one of the three categories using the Fried frailty phenotype: non-frail (0 criteria present), pre-frail (1–2 criteria present), or frail (≥ 3 criteria present).9 The five components of the Fried frailty phenotype included: (1) Weight loss: Unintentional weight loss of ≥4.5 kg in the last year. (2) Weakness: Grip strength of the dominant hand was measured using a Jamar 5030-J1 Hydraulic Hand Dynamometer (JLW Instruments, Chicago, IL 60607, United States). Weakness was defined as the lowest quartile of grip strength, stratified by sex and body mass index (BMI). The BMI cut-off points were ≤17.0, ≤17.3, ≤18.0, and ≤21.0 kg for BMI ≤23.0; 23.1–26.0; ≤26.1–29.0, and >29.0, respectively, in women and ≤29.0, ≤30.0, and ≤32.0 kg for BMI ≤24.0, 24.1–28.0, and >28.0, respectively, in men. (3) Slowness: The walking time of the patients over a 4.57-m distance was adjusted for sex and height. The cut-off points for slow walking speed were established as height ≤173 cm and time ≥7 s or height >1.73 cm and time ≥6 s for men, and height ≤1.59 cm and time ≥7 s (0.65 m/s) or height >1.59 cm and time ≥6 s (0.76 m/s) for women. (4) Exhaustion: Two statements from the Center for Epidemiologic Studies Depression Scale were used: “I felt that everything I did was an effort last week” and “I could not get going last week”.9 Participants answering “frequently” or “always” to at least one of these two statements were categorized as having met the criterion for exhaustion. (5) Low physical activity: The short version of the Minnesota Leisure Time Activity questionnaire was used with 18 activities: walking, chores, mowing the lawn, raking, gardening, hiking, jogging, biking, exercise cycling, dancing, aerobics, bowling, golf, singles tennis, doubles tennis, racquetball, calisthenics, and swimming.9 The total weekly kilocalories of physical activity expenditure were calculated using a standardized algorithm. Low activity levels were defined as <270 and <383 kcal in women and men, respectively.
Independent Variables
Age was classified into two groups: 60–74 years and age ≥75 years. Sex was categorized as men or women. Educational level was classified as pre-senior high school (below tenth grade), senior high school (from tenth to twelfth grade), or tertiary education (college, university, or postgraduate education). The patients resided in both urban and rural areas. Marital status included married and single/widowed/divorced. Alcohol intake and smoking status during the past 12 months were self-reported. BMI was classified as underweight (<18.5 kg/m2), normal weight (18.5–22.9 kg/m2), overweight (23.0–24.9 kg/m2), and obese (≥25 kg/m2).14 Limitations in functional status were evaluated using the Katz activities of daily living (ADLs) and the Lawton instrumental activities of daily living (IADLs) indices. Patients were coded as having limitations in ADLs or IADLs if they self-reported being unable to complete one or more tasks in each index.15,16
Clinical scenarios of CCS included (1) patients with suspected CAD and stable anginal symptoms and/or dyspnea; (2) patients with new-onset heart failure or left ventricular dysfunction and suspected CAD; (3) patients <1 year after ACS or recent coronary revascularization; (4) patients >1 year after initial diagnosis or coronary revascularization; (5) patients with angina and suspected vasospastic or microvascular disease; and (6) asymptomatic patients in whom CAD was detected at screening.3
Sample Size Calculation
Sample size was calculated for the primary aim using a single population proportion formula: n=Z21- α/2*[p*(1-p)/d2], with n = the required minimum sample size, Z1- α/2 = 1.96 (with α = 0.05 and 95% confidence interval) and d = precision (assumed as 0.045). Because the prevalence of frailty diagnosed using the Fried phenotype in patients with CCS is unknown, we set p as 0.5 to obtain the maximum possible value of p*(1 − p) as 0.25. Therefore, this study required a minimum of 418 participants, with an allowable margin of error of 5%.
Statistical Analyses
The Shapiro–Wilk test was used to assess the distribution of continuous variables. Continuous variables were described using median and interquartile range (IQR) (25–75th percentile) for non-normal distribution and means and standard deviations for normal distribution. Categorical variables were described as frequencies and percentages (%). Comparisons between categorical variables were conducted using the chi-square test or Fisher’s exact test. Comparisons between continuous variables were conducted using the one-way ANOVA or Kruskal–Wallis tests. To determine the factors associated with frailty and the impact of frailty on hospitalization, the non-frail and pre-frail groups were pooled together in a non-frail group. Variables with P values <0.2 in the univariate analysis were selected for multivariate logistic regression. All variables were examined for their interaction and multicollinearity. The effect size for each significant variable was determined using the Pearson’s correlation coefficient (r). All tests were two-sided, and the significance level was set at P <0.05. Data were analyzed using IBM SPSS Statistics for Windows version 25 (IBM Corp.).
Results
Prevalence of Frailty and Baseline Characteristics of Participants
Among the 437 elderly patients with CCS who underwent screening at our clinics during the study period, nine were excluded due to active malignancy (five patients), serious mental conditions (two patients), or decline to participate (two patients). After 3-month of follow-up, 8 patients were excluded because they did not respond to follow-up calls (5 patients) or because of unconfirmed hospitalization events (3 patients). The 420 patients enrolled in this study had a median age of 70 years (IQR: 65–77; range, 60–93) and male predominance (74.5%). Supplementary Figure S1 shows the flow diagram of the study participants. The prevalence of non-frail, pre-frail, and frail patients diagnosed with the Fried frailty phenotype was 22.4% (n = 94), 49.7% (n = 209), and 27.9% (n = 117), respectively.
Table 1 shows the baseline characteristics of participants according to the Fried frailty phenotype. Between the three Fried frailty phenotype groups, there were trends for increasing age with the median age of non-frail, pre-frail, and frail patients being 66, 70, and 75 years, respectively (P < 0.001). In addition, there were significant differences between the three groups in terms of marital status, BMI groups, functional status limitations, heart failure, and type 2 diabetes mellitus. Coronary revascularization for > 1 year was the most frequently reported clinical scenario in CCS (Table 2). Among the five Fried frailty phenotype components, the proportion of patients with slow walking speeds was the highest (64.0%). This criterion was most common in the frail and pre-frail patients (95.7% and 75.1%, respectively) (Table 3).
 |
Table 1 Baseline Characteristics of the Participants by Fried Frailty Phenotype |
 |
Table 2 Clinical Scenarios of Chronic Coronary Syndrome in the Participants by Fried Frailty Phenotype |
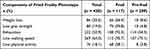 |
Table 3 Distribution of the Five Fried Frailty Components Among the Participants |
Factors Associated with Frailty
Univariate logistic regression analysis was performed to identify potential factors associated with frailty (Table 4). In the adjusted model, the three factors associated with frailty were age ≥ 75 years, limitations in ADLs, and heart failure. While limitations in ADLs had a moderate strength of association with frailty (r = 0.318), the remaining two factors had a weak strength of association. In our study, a history of coronary revascularization was not associated with frailty in elderly patients with CCS.
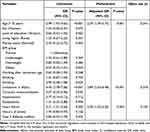 |
Table 4 Factors Associated with Frailty (n = 420) |
Impact of Frailty on 3-Month All-Cause Hospitalization
The overall 3-month hospitalization rate was higher in the frail group than in the non-frail group (23.9% vs 13.5%, P = 0.012). After adjusting for confounding variables, frailty was found to be a predictor of hospitalization in the study population, but with a weak association (r = 0.126) (Table 5).
 |
Table 5 Factors Associated with 3-Month All-Cause Hospitalization (n = 420) |
Discussion
To the best of our knowledge, this is the first study to show the burden and short-term prognostic value of frailty assessed using the Fried frailty phenotype in elderly patients with CCS. We found that about one-fourth of these patients are frail and aged ≥ 75 years, have limitations in functional status, and heart failure. In addition, our study demonstrated that frailty had an impact on the 3-month hospitalization from any cause in elderly patients. Based on these findings, we propose three points for discussion.
Prevalence of Frailty in Elderly Patients with CCS
The aging process predisposes the elderly to a higher risk of having concurrently geriatric syndromes and coronary syndromes.17 The elderly patients with coronary syndromes can be underdiagnosed, undermanaged, and have more adverse clinical events attributable to frailty.3 According to previous guidelines, assessment of frailty in elderly patients with coronary syndromes can improve clinical decision-making by informing the prediction of the benefits of revascularization or the risk of adverse reactions.3,18,19 While there are many scales used to screen and diagnose frailty, the Fried frailty phenotype is widely considered as the standard tool for assessment of frailty.20 Since the guidelines of European Society of Cardiology for the diagnosis and management of CCS published in 2019,3 there have been no studies evaluating frailty using the Fried phenotype in elderly outpatients with CCS. In 2021, there was a study of Lyu et al that assessed frailty among inpatients with CCS;13 however, this study had limited number of patients, assessed frailty by FRAIL scale, and did not group patients based on clinical scenarios of CCS.
Our study found that the prevalence of frailty in elderly outpatients with CCS was 27.9%, and approximately two-thirds of the frail patients experienced coronary revascularization in the third and fourth CCS scenarios. Since only significant stenosis of the coronary arteries requires revascularization, our findings suggest a link between the severity of coronary artery disease and frailty. However, further studies are required to confirm this pathophysiological association. Notably, the prevalence of frailty in our study was slightly lower than that in the study by Lyu et al (30.3%).13 The differences in frailty assessment tools and participant characteristics can influence the prevalence of frailty. While our patients were assessed for frailty using the Fried phenotype at clinics, a study by Lyu et al assessed frailty using the FRAIL scale in hospitalized patients.13 In addition the type of coronary syndrome (chronic or acute) can also impact the burden of frailty. For instance, the study of Nguyen et al showed that 48.1% of elderly patients with ACS are frail as defined by the Edmonton Frail Scale.21 Our finding together with others suggest that frailty can present in elderly patients under various circumstances of CAD and should be assessed in the clinical practice.
We found that slowness and exhaustion were the two most prevalent Fried frailty phenotype components in both pre-frail and frail groups. Meanwhile, low grip strength and slowness were the two criteria with the highest rates in the Vietnamese elderly population,22 The high rate of exhaustion in our study population may be due to an imbalance between myocardial oxygen supply and demand in CAD. Previous studies have shown that patients with CAD have symptoms of ischemia related to impaired coronary flow, leading to an inadequate response to physical activity.23
Factors Associated with Older Patients with CCS
Frailty is a geriatric condition that can be prevented and slowed with early detection and appropriate intervention of associated factors.24 Among elderly patients with CCS, our study found that advanced age, limitations in IADLs, and heart failure were factors associated with frailty. In cases of CCS, coronary revascularization is the clearest evidence of CAD. However, our study did not find an association between revascularization and frailty. This may require additional studies with more details, such as types of revascularization (coronary artery bypass grafting [CABG] or percutaneous coronary intervention [PCI]) and circumstances of revascularization (immediate or selective invasive strategy) to provide clearer evidence of the link between revascularization and frailty.
The association between frailty and advanced age has been clearly demonstrated in previous epidemiological and pathogenesis studies.24–26 As people age, multiple physiological dysregulation in mitochondrial function, intercellular communication, and cellular senescence result in individual metabolic and stress-response system decline, which is the basis for the manifestation of a clinical frailty phenotype.26 Previous studies have found individuals aged ≥75 years having a higher risk of CAD and cardiovascular adverse events after coronary revascularization.27,28 In the present study, our analysis revealed that age ≥75 years was associated with increased odds of frailty in patients with CCS. Since frailty has been considered a clinical characteristic determining strategy in myocardial revascularization between PCI and CABG,29 assessment of this geriatric condition should be routinely performed in patients with CCS, especially in those with advanced age.
Frailty and limitations in functional status have a reciprocal relationship. Frailty can restrict the elderly from living independently and performing instrumental activities, whereas functional status decline can be a determinant of frailty.30 In our study, multivariate analysis showed limitations in IADLs as a predictor of frailty in elderly patients with CCS. Due to the limited number of study participants with limitations in ADLs, we did not analyze geriatric conditions as a potential factor associated with frailty. Although more studies with larger sample sizes are required, our findings may preliminarily indicate the need for frailty assessment in elderly patients with CCS and functional disabilities.
There are a number of cardiovascular diseases (CVD) associated with frailty, which are independently associated with worse clinical outcomes in elderly patients with CVD.4,31–33 As for heart failure, this syndrome represents the final stage of CVD and shares some pathophysiological pathways with frailty, such as systemic inflammation, sarcopenia, comorbidities, and older age.34 In addition, the clinical relationship between heart failure and frailty is bidirectional. While heart failure can contribute to decreased functional capacity and physical activity in frail individuals, frailty can increase limited physical functional status and low quality of life in elderly patients with heart failure.34,35 Given the co-occurrence of heart failure, coronary syndromes, and frailty in elderly individuals, future studies are needed to determine the clinical and prognostic associations between the three medical conditions.
Impact of Frailty on Hospitalization in Elderly Patients with CCS
Although frailty was clearly demonstrated as an independent predictor of mortality, the evidence of impact of frailty on hospitalization risk was still conflicting.7,36 The inconsistence in the previous studies may be assumed that hospitalization risk in the frail elderly are affected by many factors, such as differences in comorbidities, healthcare access, tools of frailty assessment, and duration of follow-up. Our study is the first to reveal that frailty assessed using the Fried model is associated with short-term hospitalization risk from any cause in elderly patients with CCS. However, the weak association between frailty and hospitalization in our study reflects the need for long-term follow-up data to confirm the prognostic value of frailty for hospitalization risk.
Limitations
This study had several limitations. First, the study was conducted at a single center; therefore, the patients did not fully represent the general population. Second, the association between other comorbidities and frailty was not fully evaluated because of the low rates of some diseases. Third, except for the group of patients undergoing coronary revascularization, the remaining patients with CCS may have been inappropriately diagnosed, and the rate was incomplete. Fourth, the exhaustion assessment based on self-reported questionnaires is a subjective criterion in the Fried model. Fifth, owing to the nature of the study design, we could not conclude a causal relationship between frailty and its associated factors. Sixth, the short-term follow-up duration may not have been sufficient to determine the impact of frailty on hospitalization. Further longitudinal studies with larger sample sizes are required to confirm our findings.
Conclusions
This is the first study to determine the burden and short-term prognostic value of frailty using the Fried model in elderly patients with CCS. We found a substantial prevalence of frailty and that advanced age, functional status limitations, and heart failure are associated with frailty. We also demonstrated that frailty was a predictor of 3-month all-cause hospitalization. Our findings suggest an important role for frailty assessment in elderly patients with CCS.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available by the corresponding author, without undue reservation.
Acknowledgments
We thank the patients for their participation in our study.
Funding
The authors received no specific funding for this work.
Disclosure
The authors report no conflicts of interest in this work. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Safiri S, Karamzad N, Singh K., et al. Burden of ischemic heart disease and its attributable risk factors in 204 countries and territories, 1990-2019. Eur J Prev Cardiol. 2022;29(2):420–431. doi:10.1093/eurjpc/zwab213
2. Byrne RA, Rossello X, Coughlan JJ, et al. ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023;44(38):3720–3826. doi:10.1093/eurheartj/ehad191
3. Knuuti J, Wijns W, Saraste A, et al. ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–477. doi:10.1093/eurheartj/ehz425
4. Damluji AA, Cohen MG. The influence of frailty on cardiovascular disease: the time for a “frailty academic research consortium” is now! Circ Cardiovasc Interv. 2022;15(1):e011669. doi:10.1161/CIRCINTERVENTIONS.121.011669
5. Hoogendijk EO, Afilalo J, Ensrud KE, et al. Frailty: implications for clinical practice and public health. Lancet. 2019;394(10206):1365–1375. doi:10.1016/S0140-6736(19)31786-6
6. O’Caoimh R, Sezgin D, O’Donovan MR, et al. Prevalence of frailty in 62 countries across the world: a systematic review and meta-analysis of population-level studies. Age Ageing. 2020;50(1):96–104. doi:10.1093/ageing/afaa219
7. Chang SF, Lin HC, Cheng CL. The relationship of frailty and hospitalization among older people: evidence from a meta-analysis. J Nurs Scholarsh. 2018;50(4):383–391. doi:10.1111/jnu.12397
8. Howlett SE, Rutenberg AD, Rockwood K. The degree of frailty as a translational measure of health in aging. Nat Aging. 2021;1(8):651–665. doi:10.1038/s43587-021-00099-3
9. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol a Biol Sci Med Sci. 2001;56(3):M146–M156. doi:10.1093/gerona/56.3.m146
10. Damluji AA, Chung SE, Xue QL, et al. Frailty and cardiovascular outcomes in the national health and aging trends study. Eur Heart J. 2021;42(37):3856–3865. doi:10.1093/eurheartj/ehab468
11. Liperoti R, Vetrano DL, Palmer K, et al. Association between frailty and ischemic heart disease: a systematic review and meta-analysis. BMC Geriatr. 2021;21(1):357. doi:10.1186/s12877-021-02304-9
12. Dou Q, Wang W, Wang H, et al. Prognostic value of frailty in elderly patients with acute coronary syndrome: a systematic review and meta-analysis. BMC Geriatr. 2019;19(1):222. doi:10.1186/s12877-019-1242-8
13. Lyu H, Wang C, Jiang H, et al. Prevalence and determinants of frailty in older adult patients with chronic coronary syndrome: a cross-sectional study. BMC Geriatr. 2021;21(1):519. doi:10.1186/s12877-021-02426-0
14. WHOWP R. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. World Health Organization; 2000.
15. Shelkey M, Wallace M. Katz index of independence in activities of daily living. J Gerontol Nurs. 1999;25(3):8–9. doi:10.3928/0098-9134-19990301-05
16. Graf C. The Lawton instrumental activities of daily living scale. Am J Nurs. 2008;108(4):
17. Ilie AC, Taranu SM, Stefaniu R, et al. Chronic coronary syndrome in frail old population. Life. 2022;12(8):1133. doi:10.3390/life12081133
18. Virani SS, Newby LK, Arnold SV, et al. AHA/ACC/ACCP/ASPC/NLA/PCNA guideline for the management of patients with chronic coronary disease: a report of the American heart association/American college of cardiology joint committee on clinical practice guidelines. Circulation. 2023;148(9):e9–e119. doi:10.1161/CIR.0000000000001168
19. Lawton JS, Tamis-Holland JE, Bangalore S, et al. ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation. 2022;145(3):e18–e114. doi:10.1161/CIR.0000000000001038
20. Dent E, Martin FC, Bergman H, et al. Management of frailty: opportunities, challenges, and future directions. Lancet. 2019;394(10206):1376–1386. doi:10.1016/S0140-6736(19)31785-4
21. Nguyen TV, Le D, Tran KD, et al. Frailty in older patients with acute coronary syndrome in Vietnam. Clin Interv Aging. 2019;14:2213–2222. doi:10.2147/CIA.S234597
22. Nguyen HT, Nguyen AH, Nguyen GTX. Prevalence and associated factors of frailty in patients attending rural and urban geriatric clinics. Australas J Ageing. 2022;41(2):e122–e130. doi:10.1111/ajag.13016
23. Li H, Wei M, Zhang L, et al. Factors contributing to exercise tolerance in patients with coronary artery disease undergoing percutaneous coronary intervention. BMC Sports Sci Med Rehabil. 2023;15(1):35. doi:10.1186/s13102-023-00640-4
24. Feng Z, Lugtenberg M, Franse C, et al. Risk factors and protective factors associated with incident or increase of frailty among community-dwelling older adults: a systematic review of longitudinal studies. PLoS One. 2017;12(6):e0178383. doi:10.1371/journal.pone.0178383
25. Fedarko NS. The biology of aging and frailty. Clin Geriatr Med. 2011;27(1):27–37. doi:10.1016/j.cger.2010.08.006
26. Fried LP, Cohen AA, Xue QL, et al. The physical frailty syndrome as a transition from homeostatic symphony to cacophony. Nat Aging. 2021;1(1):36–46. doi:10.1038/s43587-020-00017-z
27. Malkin CJ, Prakash R, Chew DP. The impact of increased age on outcome from a strategy of early invasive management and revascularisation in patients with acute coronary syndromes: retrospective analysis study from the ACACIA registry. BMJ Open. 2012;2(1):e000540. doi:10.1136/bmjopen-2011-000540
28. Chen PF, Wang DN, Chen K, et al. Outcomes of percutaneous coronary intervention in patients >/= 75 years: one-center study in a Chinese patient group. J Geriatr Cardiol. 2015;12(6):626–633. doi:10.11909/j.issn.1671-5411.2015.06.004
29. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165. doi:10.1093/eurheartj/ehy394
30. Costenoble A, Knoop V, Vermeiren S, et al. A comprehensive overview of activities of daily living in existing frailty instruments: a systematic literature search. Gerontologist. 2019;61(3):e12–e22. doi:10.1093/geront/gnz147
31. Polidoro A, Stefanelli F, Ciacciarelli M, et al. Frailty in patients affected by atrial fibrillation. Arch Gerontol Geriatr. 2013;57(3):325–327. doi:10.1016/j.archger.2013.04.014
32. McNallan SM, Singh M, Chamberlain AM, et al. Frailty and healthcare utilization among patients with heart failure in the community. JACC Heart Fail. 2013;1(2):135–141. doi:10.1016/j.jchf.2013.01.002
33. Singh M, Stewart R, White H. Importance of frailty in patients with cardiovascular disease. Eur Heart J. 2014;35(26):1726–1731. doi:10.1093/eurheartj/ehu197
34. Pandey A, Kitzman D, Reeves G. Frailty Is Intertwined With Heart Failure: mechanisms, Prevalence, Prognosis, Assessment, and Management. JACC Heart Fail. 2019;7(12):1001–1011. doi:10.1016/j.jchf.2019.10.005
35. Denfeld QE, Winters-Stone K, Mudd JO, et al. The prevalence of frailty in heart failure: a systematic review and meta-analysis. Int J Cardiol. 2017;236:283–289. doi:10.1016/j.ijcard.2017.01.153
36. EL B, JM G, PM R, et al. Prevalence and outcomes of frailty in unplanned hospital admissions: a systematic review and meta-analysis of hospital-wide and general (internal) medicine cohorts. EClinicalMedicine. 2023;59:101947. doi:10.1016/j.eclinm.2023.101947
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
