Back to Journals » Research Reports in Clinical Cardiology » Volume 7
Frequency of coronary artery stenosis in patients with asymptomatic familial hypercholesterolemia and its association with carotid intimal thickness and cardio-ankle vascular index
Authors Suzuki M, Takahashi M , Iizuka T, Terada H, Noike H, Shirai K
Received 4 December 2015
Accepted for publication 29 February 2016
Published 28 June 2016 Volume 2016:7 Pages 83—90
DOI https://doi.org/10.2147/RRCC.S101805
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Richard Kones
Masayo Suzuki,1 Mao Takahashi,1 Takuo Iizuka,1 Hitoshi Terada,2 Hirohumi Noike,1 Kohji Shirai3
1Cardiovascular Center, Internal Medicine, 2Department of Radiology, 3Department of Vascular Function, Sakura Hospital, Medical Center, Toho University, Sakura City, Chiba Prefecture, Japan
Background: Familial hypercholesterolemia (FH) is associated with premature coronary arterial disease. We aimed to determine the incidence of coronary artery stenosis (CAS) in asymptomatic FH patients using coronary computed tomography angiography (CCTA). To investigate the association between CAS and atherosclerosis of carotid arteries, we performed ultrasonography to measure the mean intima-media thickness (IMT), maximum IMT, and plaque score. We also aimed to examine the significance of the cardio-ankle vascular index (CAVI) and its association with the incidence of CAS in asymptomatic FH patients.
Patients and methods: We enrolled consecutively, 31 FH patients without symptoms of coronary artery disease. Based on the CCTA findings, we divided the patients into two groups, those with and without CAS, and compared various parameters and risk factors of the two groups.
Results: Of 31 FH patients, seven patients (22.6%) had CAS. The proportion of male patients and mean low-density lipoprotein-cholesterol level were higher in patients with CAS than in those without CAS (P<0.05). All carotid ultrasonography parameters (ie, mean IMT, maximum IMT, and plaque score) were significantly higher in patients with CAS than in those without CAS (P<0.01), whereas no significant difference was found in CAVI between the two groups.
Conclusion: CAS was identified in >22.6% of the asymptomatic FH patients. Patients with CAS tended to have enhanced levels of carotid plaque markers, but no increase was noted in CAVI. FH patients should be continuously monitored using CCTA and ultrasonography.
Keywords: CAVI, coronary artery stenosis, heterozygous familial hypercholesterolemia, CCTA, ultrasound evaluation of the carotid artery
Corrigendum for this paper has been published
Introduction
Familial hypercholesterolemia (FH) is characterized by markedly elevated low-density lipoprotein (LDL)-cholesterol levels and premature coronary artery disease.1–3 The known hereditary mutant alleles are LDL-receptor, apolipoprotein B-100, and PCSK9 genes.4 The prevalence of heterozygous FH is reported to be one in 500 in the general population.5 Although coronary angiographical studies are recommended in FH patients to monitor premature coronary arterial disease,6,7 in clinical practice, it is often difficult to perform such invasive studies in asymptomatic FH patients. The recent advancement in multislice computed tomography (MSCT) imaging technology that demonstrates coronary artery imaging using a 64-slice MSCT scanner allows a less-invasive means of assessment.8,9 In the present study, we performed coronary computed tomography angiography (CCTA) with a 64-slice scanner to determine the frequency of coronary artery stenosis (CAS) in asymptomatic FH patients (ie, who had no coronary symptoms and no known coronary artery disease).
Because atherosclerosis is a systemic arterial disease,10 coronary atherosclerosis is associated with arteriosclerosis of the carotid artery as well as that of the aorta and femoral and tibial arteries.11,12 Therefore, in the present study, we also aimed to investigate the association between CAS and carotid atherosclerosis in asymptomatic FH patients. We performed B-mode (two dimensional) arterial ultrasonography, a noninvasive method to evaluate the extent of atherosclerosis in carotid arteries13–15 and to measure the mean intima-media thickness (IMT), maximum IMT, and plaque score (PS), which are known markers of carotid atherosclerosis.16
Furthermore, we measured the cardio-ankle vascular index (CAVI) to evaluate arterial stiffness in asymptomatic FH patients, as it is another marker of atherosclerosis. As a noninvasive method to assess arterial stiffness, pulse wave velocity (PWV) has long been used as an established marker.17–20 In particular, carotid-femoral PWV is a useful predictor of coronary artery diseases in arteriosclerotic patients.21,22 However, PWV has been found to be altered by blood pressure (BP) at the time of measurement.23 Against this background, CAVI was developed as a more reliable marker of atherosclerosis.24 CAVI, which represents the stiffness of the artery from the origin of the aorta to the ankle, is derived from the stiffness parameter beta theory of Hayashi et al.25 CAVI has been shown to be independent of BP at the time of measurement.25,26 Several clinical studies have shown that CAVI is increased in patients with CAS,27–30 chronic kidney disease,31 severe diabetes mellitus, and hypertension; those on hemodialysis; and smokers.32 CAVI is considered to be an excellent surrogate marker of general atherosclerosis. Nevertheless, the predictive ability of CAVI for coronary artery disease in FH patients has not yet been fully investigated. Although it is reported that CAVI is not elevated in FH patients,33 hypercholesterolemia is associated with CAVI.34 Therefore, in the present study, we aimed to determine whether CAVI could be a predictor of coronary atherosclerosis in asymptomatic FH patients.
Patients and methods
Patients
We used data from 31 consecutive FH patients without symptoms of angina who were diagnosed as having FH at our department during the period between September 2007 and September 2011, according to the criteria proposed by the research group on primary hyperlipoproteinemia in the Ministry of Welfare and Labour of Japan.35 The patients were admitted with suspected coronary artery disease because FH is known to have severe coronary atherosclerosis. Briefly, the criteria are total cholesterol level >230 mg/dL, Achilles tendon thickness >9 mm, and a familial history of hypercholesterolemia.
Based on the findings of CCTA, we identified patients with CAS (CAS group) and compared them with those without CAS (non-CAS group) to determine risk factors for the incidence of CAS in asymptomatic FH patients.
This study was designed and monitored in accordance with the ethics and principles of Good Clinical Practice and the Declaration of Helsinki. This study was approved by the institutional review board of Toho University Sakura Medical Center. Before participation, the purpose of this study was explained to each patient, and all participants gave written informed consent.
Computed coronary tomographic angiography
Multislice CCTA was performed using Aquilion 64-slice scanner (Toshiba Co., Tokyo, Japan). The CCTA data were analyzed on a three-dimensional workstation (ZIO M900 QUADRA; Amin Co., Ltd., Tokyo, Japan). Metoprolol 20–60 mg was administered as the premedication to decrease the pulse rate to 50–70 pulses/min. Each patient’s heart was controlled under sinus rhythm. Scan protocol was performed according to prospective gating methods with 120 kV×200 mA. The angiographic agent, iopamidol-370 (body weight ×0.05 mL/sec), was administered through the brachial medial vein. Scans were analyzed by consensus of two observers unaware of the clinical data. Luminal narrowing of ≥50% on CCTA at the worst view position indicated CAS.36 The 15-segment American Heart Association model of the coronary tree was used.7 Each lesion identified was examined using maximum intensity and multiplanar reconstruction techniques along multiple longitudinal axes and also transversely. Plaque with calcification was defined as >130 Hounsfield unit (HU) with 3 mm length, and noncalcified plaque was defined as <120 HU.
Ultrasound evaluation of the carotid artery
Ultrasound evaluation of the common carotid artery was performed with high-resolution ultrasonography (Toshiba Co.) using a 7.5 MHz probe equipped with a Doppler system. After the patient had rested in the supine position, the neck was slightly hyperextended and optimal bilateral visualization of the carotid arteries was performed according to the method of Terminology and Diagnostic Criteria Committee, Japan Society of Ultrasonics in Medicine.16 Based on multiple visualizations, plaque formation was identified as the presence of wall thickness >1.1 mm and wall thickening at least 50% greater than the thickness of the surrounding wall. The IMT was measured as the distance from the leading edge of the first echogenic line to the leading edge of the second echogenic line. In order to obtain the mean IMT values, the IMT values at sites 1 cm and 2 cm proximal to the bulb from the anterior, lateral, and posterior approaches were averaged. No measurements were carried out at the level of discrete plaques. The maximum IMT represents the greatest carotid IMT in the observable areas of the common carotid artery, carotid bulb, and the internal carotid artery. The PS was determined as the sum of plaque thicknesses of three segments >1.1 mm of the carotid artery (ie, common carotid artery, carotid bulb, and internal carotid artery) on both the right and left sides.16,37
Cardio-ankle vascular index
CAVI was measured using VaSera1500 (Fukuda Denshi Co. Ltd., Tokyo, Japan). Examinations were performed after resting for 10 minutes. The measurement method was described previously.24 Briefly, CAVI is calculated by applying BP and PWV to the following formula: CAVI = a{(2ρ/ΔP) × ln(Ps/Pd)PWV2} + b, where Ps is systolic BP, Pd is diastolic BP, PWV is pulse wave velocity, ΔP is Ps−Pd, ρ is blood density, and a and b are constants. The brachial and ankle pulse waves were determined using inflatable cuffs with the pressure maintained between 30 mmHg and 50 mmHg to ensure that the cuff pressure had a minimal effect on the systemic hemodynamics. BP and pulse pressure were determined simultaneously.
Blood sample collection
Blood samples were collected from the antecubital vein in the morning after 12 hours of fasting. To measure hemoglobin A1c (HbA1c), blood was collected in tubes containing ethylenediaminetetraacetic acid. The stable and unstable fractions of HbA1c were measured by high-pressure liquid chromatography (Hi-Auto A1c analyzer system; Kyoto Daiichi Kagaku, Kyoto, Japan). Stable form data were used in the present analysis. HbA1c was expressed as the value determined by the National Glycohemoglobin Standardization Program.
Plasma total cholesterol and triglyceride levels were measured enzymatically using kits from Nippon Shoji Co., Ltd. (Osaka, Japan) and a 7150 analyzer (Hitachi Ltd., Tokyo, Japan). Serum high-density lipoprotein cholesterol was measured using a selective inhibition assay (Daiichi Pure Chemicals Co., Ltd., Tokyo, Japan). Serum LDL cholesterol levels were calculated using the Friedewald formula.38
Definition of risk factors
Diabetes mellitus was defined according to the World Health Organization criteria and/or as having received treatment for diabetes mellitus. Dyslipidemia was defined as a total cholesterol concentration ≥220 mg/dL, a triglyceride concentration ≥150 mg/dL, and/or having received treatment for dyslipidemia. Hypertension was defined as systolic BP ≥140 mmHg, diastolic BP ≥90 mmHg, and/or having received treatment for hypertension.
Statistical analysis
Statistical analysis was performed using SPSS Version 16.0 for Windows (SPSS Inc., Chicago, IL, USA). Quantitative data were expressed as mean value ± 1 SD. Qualitative variables were presented by calculating the frequency and percentage. The comparison between CAS and non-CAS groups was performed using the Mann–Whitney U test. Qualitative variables were presented by the exact model. These risk factors were scored as explanatory factors, and the subordinate variables were CAS =1 and non-CAS =0. The receiver operating characteristic (ROC) curve analysis was performed to determine the sensitivity and specificity of potential parameters used for diagnosis of CAS. A two-tailed P-value of <0.05 was considered statistically significant.
Results
Patient characteristics
Table 1 shows the characteristics of patients, including serum profiles and medical treatment. The majority of patients were women. Approximately one-third of the patients had diabetes mellitus and more than one-third had hypertension. The mean total cholesterol was 237.4 mg/dL, and most patients were receiving treatment for hypercholesterolemia.
Findings from CCTA, ultrasonography, and CAVI
Table 2 shows the findings from CCTA, ultrasonography, and CAVI in 31 patients. The CCTA revealed that seven patients (22.6%) had CAS, two patients had one affected vessel, and five patients had two affected vessels. Coronary calcified plaque was found in 19 (61.3%) patients.
Comparisons of risk factors between the CAS group and non-CAS group
Risk factors
There was no significant difference in the mean age between the CAS group and non-CAS group. There were more male patients in the CAS group than in the non-CAS group. HbA1c was slightly higher in the CAS group than in the non-CAS group, but the difference was not significant. In both groups, most patients had received treatment with lipid-lowering agents; statins were most commonly taken in both groups, followed by ezetimibe and probucol. Although all patients in the CAS group were under lipid-lowering treatment, LDL-cholesterol level was higher in the CAS group than in the non-CAS group (Table 3).
Carotid arteriosclerotic findings
Mean IMT, maximum IMT, and PS were significantly higher in the CAS group than in the non-CAS group (Table 3).
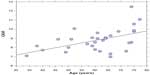
CAVI
There was a significant correlation between age and CAVI (Figure 1). However, CAVI was not significantly higher in the CAS group compared with the non-CAS group (Table 3).
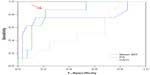
ROC curve analysis in patients with CAS
The ROC curve analysis was performed to determine cutoff values of various parameters (mean IMT, PS, and CAVI) based on the proportion of true-positive results (sensitivity) and false-positive results (1− specificity) to determine the probability of CAS in FH patients (Figure 2). The cutoff values of mean IMT and PS that gave the maximum sensitivity and specificity for CAS were 0.82 mm and 5.1 mm, respectively. At the cutoff level, the sensitivities of mean IMT and PS for CAS were 75%, and 87.5%, respectively, and the specificities were 85.7% and 78.6%, respectively.
Multiple regression analysis of various parameters for CAS
To investigate the impact of carotid arterial findings (mean IMT, max IMT, and PS), we performed multiple regression analysis, including CAVI, age, sex, and duration of statin therapy. Mean IMT and PS were selected as independent risk factors for CAS (Table 4).
Discussion
In the present study enrolling 31 asymptomatic FH patients, CAS was observed in 22.6% of patients; noncalcified plaque was observed in 29.0% of patients and calcified plaque was observed in 61.3% of patients. The incidence of CAS was similar to that of a previous report.39 Since FH is known to be associated with coronary events even in younger patients,6,7 the high incidence of CAS in FH patients should not be overlooked. We consider that FH patients should be monitored for CAS via less-invasive methods such as CCTA, even when they have no symptoms.
In patients with CAS, the proportions of male patients and mean LDL-cholesterol level were higher than in non-CAS patients, suggesting that these factors may be associated with the incidence of CAS in FH patients. The proportions of patients who had concomitant diabetes mellitus (57.1%) and hypertension (57.1%) were higher in the CAS group than in non-CAS patients (29.2% and 20.8%, respectively). The difference was not significant. But, controlling these risk factors may be important in FH patients.
We also compared the findings from ultrasonography of the carotid artery and CAVI in terms of predictive ability of CAS in FH patients. As shown in Table 3, the carotid parameters measured by ultrasonography (ie, mean IMT, maximum IMT, and PS) were significantly higher in CAS patients than in non-CAS patients, suggesting that the presence of carotid plaque may be a predictor of coronary arteriosclerosis in asymptomatic FH patients. Since the PS showed the most marked difference among the carotid parameters measured in the present study (Table 4), it may be a useful index for the prediction of CAS in asymptomatic FH patients.
CAVI was not significantly different between patients with and without CAS. This was consistent with the findings from the previous by Soska et al. They compared CAVI in FH patients and in healthy controls.33 There was no significant difference in HDL-cholesterol levels between FH patients and the controls.33 In our study, there was also no significant difference in HDL-cholesterol levels between patients with and without CAS, although LDL-cholesterol level was higher in patients with CAS. On the other hand, another study showed that a significant increase in CAVI was observed in patients with combined hyperlipidemia who had a low (<40 mg/dL) HDL-cholesterol level but not in patients with hypercholesterolemia alone.40 These findings suggested that CAVI may increase when both increased LDL-cholesterol level and decreased HDL-cholesterol level were observed.
Another possible explanation as to why no increase in CAVI was observed in CAS patients may be attributed to the developmental process of atherosclerosis in FH patients. We consider that FH patients may have a different developmental process of wall thickening from those with atherosclerosis, caused by hypertension, obesity, and diabetes. Atherosclerosis develops through several processes of fatty streak, fibrous plaque, atheroma formation, and complicated lesion.41 When the fatty streak was formed cholesterol ester deposed. Afterward calcification and/or inflammation occur at the fibrous plaque to complicated lesion stages. In a study that measured aortic PWV in rabbits, aortic stiffness was not enhanced in hypercholesterolemia.42 Therefore, in FH patients, an increase in CAVI may not be prominent at the fatty streak stage when calcification and inflammatory processes have not been established. However, CAVI may be increasing when calcification and inflammatory processes have started. In fact, increased CAVI was observed in FH patients who had developed severe coronary stenosis, and underwent angioplasty (data not shown). Therefore, in clinical practice, even when CAVI shows normal in FH patients, coronary artery disease cannot be denied. We consider that FH patients should be continuously monitored with CCTA and ultrasonography.
Limitations
Although FH is not a common disease, the sample size of the present study was small. Nevertheless, a statistical significance was obtained for some parameters for the prediction of CAS in asymptomatic FH patients. We consider the findings are important and useful in clinical practice.
Conclusion
Although the sample size limits the ability to draw conclusions, in this study of asymptomatic FH patients, CAS was identified in 22.6% of patients by CCTA. An increase in CAVI was not observed in patients with CAS; however, the possibility of coronary artery disease cannot be ruled out, and FH patients should be continuously monitored with CCTA and ultrasonography.
Acknowledgments
We wish to thank the members of the Clinical Physiology Unit for the measurement of CAVI and also the members of the Radiological Department for examination of MSCT. The Department of Vascular Function was funded by Fukuda Denshi CO., Ltd.
Disclosure
The authors report no conflicts of interest in this work.
References
Nemati MH, Astaneh B. Optimal management of familial hypercholesterolemia:treatment and management strategies. Vasc Health Risk Manag. 2010;6:1079–1088. | |
Raal FJ, Santos RD. Homozygous familial hypercholesterolemia:current perceptions on diagnosis and treatment. Atherosclerosis. 2012;223(2):262–268. | |
Maiorana A, Nobili V, Calandra S, et al. Preemptive liver transplantation in a child with familial hypercholesterolemia. Pediatr Transplant. 2011;15(2):E25–E29. | |
Soutar AK, Naoumova RP. Mechanisms of disease:genetic causes of familial hypercholesterolemia. Nat Clin Pract Cardiovasc Med. 2007;4(4):214–225. | |
Bujo H, Takahashi K, Saito Y, et al; Research Committeon Primary Hyperlipidemia of the Ministry of Health, Labour, and Welfare of Japan. Clinical features of familial hypercholesterolemia in Japan in a database from 1996 to 1998 by the research committee of the ministry of health, labour and welfare of Japan. J Atheroscler Thromb. 2004;11(3):146–151. | |
Hirobe K, Matsuzawa Y, Ishikawa K, et al. Coronary artery disease in heterozygous familial hypercholesterolemia. Atherosclerosis. 1982;44(2):201–210. | |
Mabuchi H, Koizumi J, Shimizu M, Takeda R. Development of coronary heart disease in familial hypercholesterolemia. Circulation. 1989;79(2):225–232. | |
Meijboom WB, Meijs MF, Schuijf JD, et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography:a prospective, multicenter, multivendor study. J Am Coll Cardiol. 2008; 52(25):2135–2144. | |
Ropers D, Baum U, Pohle K, et al. Detection of coronary artery stenosis with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation. 2003;107(5):664–666. | |
Hata J, Kiyohara Y. Epidemiology of stroke and coronary artery disease in Asia. Circ J. 2013;77(8):1923–1932. | |
Kafetzakis A, Kochiadakis G, Laliotis A, et al. Association of subclinical wall changes of carotid, femoral, and popliteal arteries with obstructive coronary artery disease in patients undergoing coronary angiography. Chest. 2005;128(4):2538–2543. | |
Boaz M, Chernin G, Schwartz I, et al. C-reactive protein and carotid and femoral intima media thickness:predicting inflammation. Clin Nephrol. 2013;80(6):449–455. | |
Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of the arterial wall:a direct measurement with ultrasound imaging. Circulation. 1986;74(6):1399–1406. | |
Fell G, Phillips DJ, Chikos PM, Harley JD, Thiele BL, Strandness DE Jr. Ultrasonic duplex scanning for disease of the carotid artery. Circulation. 1981;64(6):1191–1195. | |
Craven TE, Ryu JE, Espeland MA, et al. Evaluation of the associations between carotid artery atherosclerosis and coronary artery stenosis. A case-control study. Circulation. 1990;82(4):1230–1242. | |
Terminology and Diagnostic Criteria Committee, Japan Society of Ultrasonics in Medicine; Subcommittee for Preparing Guidelines for Ultrasound Diagnosis of Carotid Artery. Standard method for ultrasound evaluation of carotid artery lesions. Jpn J Med Ultrason. 2009;36:501–518. | |
Blacher J, Asmar R, Djane S, London GM, Safar ME. Aortic pulse wave velocity as a marker of cardiovascular risk in hypertensive patients. Hypertension. 1999;33(5):1111–1117. | |
Amar J, Ruidavets JB, Chamontin B, Drouet L, Ferrières J. Arterial stiffness and cardiovascular risk factors in a population-based study. J Hypertens. 2001;19(3):381–387. | |
Sutton-Tyrrell K, Najjar SS, Boudreau RM, et al. Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation. 2005;111(25):3384–3390. | |
Rocha E. [Pulse wave velocity:a marker of arterial stiffness and its applicability in clinical practice.] Rev Port Cardiol. 2011;30(9):699–702. Portuguese. | |
Mitchell GF, Vita JA, Larson MG, et al. Cross-sectional relations of peripheral microvascular function, cardiovascular disease risk factors, and aortic stiffness:the Framingham Heart Study. Circulation. 2005; 112(24):3722–3728. | |
Podolec P, Kopeć G, Podolec J, et al. Aortic pulse wave velocity and carotid-femoral pulse wave velocity:similarities and discrepancies. Hypertens Res. 2007;30(12):1151–1158. | |
Nye ER. The effect of blood pressure alteration on the pulse wave velocity. Br Heart J. 1964;266:261–265. | |
Shirai K, Utino J, Otsuka K, Takata M. A novel blood pressure-independent arterial wall stiffness parameter; cardio-ankle vascular index (CAVI). J Atheroscler Thromb. 2006;13(2):101–107. | |
Hayashi K, Handa H, Nagasawa S, Okumura A, Moritake K. Stiffness and elastic behavior of human intracranial and extracranial arteries. J Biomech. 1980;13(2):175–184. | |
Shirai K, Song M, Suzuki J, et al. Contradictory effects of β1- and α1- aderenergic receptor blockers on cardio-ankle vascular stiffness index (CAVI) – the independency of CAVI from blood pressure. J Atheroscler Thromb. 2011;18(1):49–55. | |
Nakamura K, Tomaru T, Yamamura S, Miyashita Y, Shirai K, Noike H. Cardio-ankle vascular index is a candidate predictor of coronary atherosclerosis. Circ J. 2008;72(4):598–604. | |
Horinaka S, Yabe A, Yagi H, et al. Cardio-ankle vascular index could reflect plaque burden in the coronary artery. Angiology. 2011; 62(5):401–408. | |
Park JB, Park HE, Choi SY, Kim MK, Oh BH. Relation between cardio-ankle vascular index and coronary artery calcification or stenosis in asymptomatic subjects. J Atheroscler Thromb. 2013;20(6):557–567. | |
Miyoshi T, Doi M, Hirohata S, et al. Cardio-ankle vascular index is independently associated with the severity of coronary atherosclerosis and left ventricular function in patients with ischemic heart disease. J Atheroscler Thromb. 2010;17(3):249–258. | |
Takenaka T, Hoshi H, Kato N, et al. Cardio-ankle vascular index to screen cardiovascular diseases in patients with end-stage renal diseases. J Atheroscler Thromb. 2008;15(6):339–344. | |
Shirai K, Hiruta N, Song M, et al. Cardio-ankle vascular index (CAVI) as a novel indicator of arterial stiffness:theory, evidence and perspectives. J Atheroscler Thromb. 2011;18(11):924–938. | |
Soska V, Dobsak P, Dusek L, et al. Cardio-ankle vascular index in heterozygous familial hypercholesterolemia. J Atheroscler Thromb. 2012;19(5):453–461. | |
Park HE, Choi SY, Kim MK, Oh BH. Cardio-ankle vascular index reflects coronary atherosclerosis in patients with abnormal glucose metabolism:assessment with 256 slice multi-detector computed tomography. J Cardiol. 2012;60(5):372–376. | |
Japan Atherosclerosis Society, editor. [Japan Atherosclerosis Society Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases.] 2007 ed. Tokyo:Kyorinsha; 2007. Japanese. | |
Fujihara K, Suzuki H, Sato A, et al. Comparison of the Framingham Risk Score, UK Prospective Diabetes Study (UKPDS) Risk Engine, Japanese Atherosclerosis Longitudinal Study-Existing Cohorts Combine (JALS-ECC) and maximum carotid intima-media thickness for predicting coronary artery stenosis in patients with asymptomatic type 2 diabetes. J Atheroscler Thromb. 2014;21(8):799–815. | |
Katakami N, Kaneto H, Osonoi T, et al. Usefulness of lipoprotein ratios in assessing carotid atherosclerosis in Japanese type 2 diabetic patients. Atherosclerosis. 2010;214(2):442–447. | |
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. | |
Sugisawa T, Okamura T, Makino H, et al. Defining patients at extremely high risk for coronary artery disease in heterozygous familial hypercholesterolemia. J Atheroscler Thromb. 2012;19(4):369–375. | |
Dobsak P, Soska V, Sochor O, et al. Increased cardio-ankle vascular index in hyperlipidemic patients without diabetes or hypertension. J Atheroscler Thromb. 2015;22(3):272–283. | |
Strong JP, Malcom GT, Newman WP 3rd, Oalmann MC. Early lesions of atherosclerosis in childhood and youth:natural history and risk factors. J Am Coll Nutr. 1992;11(suppl):51S–54S. | |
Hayashi S, Obara S, Murakawa M, Hazama A, Kusanagi M, Katsuda S. To what extent does aortic pulse wave velocity estimate early atherosclerosis in Kurosawa and Kusanagi-hypercholesterolemic rabbits? Hypertens Res. 2011;34(5):559–564. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.