Back to Journals » Clinical Ophthalmology » Volume 13
Familial Background Factors And Their Association With Non-Organic Visual Loss
Authors Takahashi M, Kunikata H, Kato K, Kawakami A, Nakazawa T
Received 15 April 2019
Accepted for publication 3 October 2019
Published 21 October 2019 Volume 2019:13 Pages 2059—2061
DOI https://doi.org/10.2147/OPTH.S212365
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Misuzu Takahashi,1 Hiroshi Kunikata,2,3 Keiichi Kato,1 Ayako Kawakami,1 Toru Nakazawa2–5
1Kato Eye Clinic, Taiwa-cho, Japan; 2Department of Ophthalmology, Tohoku University Graduate School of Medicine, Sendai, Japan; 3Department of Retinal Disease Control, Tohoku University Graduate School of Medicine, Sendai, Japan; 4Department of Advanced Ophthalmic Medicine, Tohoku University Graduate School of Medicine, Sendai, Japan; 5Department of Ophthalmic Imaging and Information Analytics, Tohoku University Graduate School of Medicine, Sendai, Japan
Correspondence: Keiichi Kato Kato Eye Clinic 2-8-10, Yoshioka-Higashi, Taiwa-cho, Kurokawa-gun, Miyagi 981-3627, Japan
Tel +81 22 347 1682
Fax +81 22 347 1683
Email [email protected]
Purpose: To identify new types of clinical findings that could be used to diagnose and treat non-organic visual loss (NOVL).
Methods: This study retrospectively examined the records of 191 patients diagnosed with NOVL at the Kato Eye Clinic. Clinical characteristics, including uncorrected visual acuity (UCVA) and complaints of vision loss, were compared in 125 of 191 patients with NOVL and control subjects with organic refractive errors, identified during annual school health checks. If available, familial background data for the NOVL patients were compared with data from a mass population study. Familial background data included the presence of siblings, and whether the mother worked outside the home.
Results: Patients with NOVL were more likely to be younger and female (P=0.02, and P<0.001, respectively). UCVA was statistically similar in the better eyes of the NOVL and control subjects (P=0.60), even though the NOVL patients were much more likely to be emmetropic (P<0.001). Complaints of vision loss were significantly more common in the patients with NOVL than in the control subjects (P=0.001). There was no significant difference in the presence of siblings between the subjects in the mass population study and the patients with NOVL (P=0.38), but the NOVL patients were significantly more likely to have a mother who did not work outside the home (P=0.01).
Conclusion: Patients with NOVL tended to be younger, female and to complain more often of vision loss, compared to control subjects with organic refractive errors. Familial background factors, including the presence of siblings or a mother working outside the home, seemed not to be associated with the pathogenesis of NOVL, compared to subjects in a mass population study.
Keywords: psychogenic visual disturbance, hysterical visual loss, functional visual loss, visual acuity, mother
Background
Non-organic visual loss (NOVL), previously also known as hysterical, functional, or psychogenic visual loss, is diagnosed when visual acuity (VA) or the visual field is decreased without any identifiable organic cause.1 NOVL occurs mainly in pre-pubescent and pubescent children from about 8 to 14 years old, and more often in female patients than male patients.2,3 The diagnosis of NOVL is generally made based on positive findings of visual recovery after tests using a neutralizing or fogging lens, or findings of a spiral visual field or tubular tunnel vision, which are considered characteristic of NOVL. Since symptoms eventually completely resolve in almost all children diagnosed with NOVL,3,4 differentiation of NOVL from organic vision loss is important. Pattern onset visual-evoked potential testing may be a promising tool to identify NOVL,5,6 but it is not commonly used clinically. Though the pathogenesis of NOVL remains unclear, psychogenic factors, including familial background and school life, are thought to explain many cases of NOVL. To identify new types of clinical findings that could be used to diagnose and treat NOVL, we measured the incidence of complaints of visual loss and investigated familial background factors in more than 100 cases of NOVL.2,3,5–7 We then examined familial background factors in more than 28,000 subjects included in a Japanese mass population study.
Methods
This study retrospectively examined the records of 191 patients diagnosed with NOVL between 2009 and 2013 at the Kato Eye Clinic. Subjects were excluded if visual loss had been found outside of school or if there was any history of intraocular surgery, optic nerve disease or other vitreoretinal disease. NOVL was diagnosed based on positive findings by an ophthalmological specialist (K.K.). The 191 subjects with NOVL included 102 subjects with a spiral visual field (53%), 6 subjects with tubular tunnel vision (3%), 70 subjects with a normal visual field (37%), and 13 subjects with no data for the visual field. Clinical characteristics, including uncorrected visual acuity (UCVA) and complaints of vision loss, were compared in 125 of 191 patients with NOVL, identified during annual school health checks, and control subjects who underwent the same school heath checks and were judged as having a VA grade of C, with the presence of organic refractive errors (REs) being confirmed later at the Kato Eye Clinic. VA grade C is defined in Japanese schools as decimal UCVA more than 0.2 and less than 0.7 in the worse eye. Furthermore, to investigate familial background factors and their association with NOVL, the patients with NOVL were compared with subjects from a mass population study (the Seventh Longitudinal Survey of Newborns in the 21st Century, Japan Ministry of Health, Labor and Welfare). Familial background factors included the presence of siblings, and whether the mother worked outside the home.
Results
Table 1 summarizes clinical data and findings in the NOVL and VA grade C groups on UCVA and how often subjects complained of vision loss. Patients with NOVL were more likely to be younger and female (P=0.02, and P<0.001, respectively). UCVA was statistically similar in the better eyes of the NOVL and control subjects (P=0.70), even though the NOVL patients were much more likely to be emmetropic (P<0.001). Complaints of vision loss were significantly more common in the patients with NOVL than in the control subjects (P=0.001). Table 2 summarizes familial background factors in patients with NOVL at the Kato Eye Clinic and compares these factors with subjects from a mass population study. There was no significant difference in the presence of siblings between the subjects in the mass population study and the patients with NOVL (P=0.38), but the NOVL patients were significantly more likely to have a mother who did not work outside the home (P=0.01).
 |
Table 1 Clinical Characteristics, Visual Acuity and Complaints of Vision Loss |
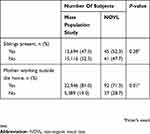 |
Table 2 Familial Background Factors and Their Association with NOVL |
Discussion
Children with NOVL are generally thought to be more likely to complain of vision loss, although the precise rate of such complaints remains unclear. A past report analyzing 30 patients with NOVL showed that about 90% of patients complained of reduced or blurred vision.3 The current study, which analyzed 125 patients with NOVL, also found a higher rate of complaints of vision loss in NOVL patients (about 70%) than in patients with organic REs, i.e., school-judged VA grade C (40%), suggesting that patients with NOVL might want more attention from physicians than patients with organic REs. This may be explained by the psychogenic nature of NOVL. Approximately 30% of NOVL patients have previously been given a psychiatric diagnosis, such as anxiety or depression, and about a quarter of NOVL patients express a desire to obtain eyeglasses.7 It has also been reported that about 40–60% of NOVL patients have difficulties in their family lives and in school.2,3 Though the presence of siblings is generally thought to be associated with NOVL, the current study showed no such association. However, interestingly, this study showed that patients with NOVL were more likely to have a stay-at-home mother. Thus, even though loneliness associated with a working mother might be expected to contribute to NOVL, in fact, a mother working outside the home seemed not to be associated with the pathogenesis of NOVL. These results suggest that familial background factors such as siblings or a mother working outside the home, commonly associated with psychological development, do not contribute to the development of NOVL in children.
Limitations of this study included its retrospective nature, and the comparison of data from a private clinic with data from a mass population study. We did not record familial background factors in the students without suspected NOVL, so we could not compare familial background factors in the NOVL and VA grade C subjects. Future investigations should collect familial background factors from a control group of students without suspected NOVL for comparison.
Ethics
This study followed the tenets of the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of the Kato Eye Clinic. Patient consent was not required by the ethics committee since data were obtained retrospectively from patients’ records and no patient was individually identified in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lessell S. Nonorganic visual loss: what’s in a name? Am J Ophthalmol. 2011;151:569–571. doi:10.1016/j.ajo.2010.11.015
2. Catalono RA, Simon JW, Krohel GB, Rosenberg PN. Functional visual loss in children. Ophthalmology. 1986;93:385–390. doi:10.1016/s0161-6420(86)33730-8
3. Bain KE, Beatty S, Lloyd C. Non-organic visual loss in children. Eye (Lond). 2000;14(Pt 5):770–772.
4. Toldo I, Pinello L, Suppiej A, et al. Nonorganic (Psychogenic) visual loss in children: a retrospective series. J Neuroophthalmol. 2010;30:26–30. doi:10.1097/WNO.0b013e3181c252b9
5. McBain VA, Robson AG, Hogg CR, Holder GE. Assessment of patients with suspected non-organic visual loss using pattern appearance visual evoked potentials. Graefes Arch Clin Exp Ophthalmol. 2007;245:502–510. doi:10.1007/s00417-006-0431-2
6. Somers A, Casteels K, Van Roie E, Spileers W, Casteels I. Non-organic visual loss in children: prospective and retrospective analysis of associated psychosocial problems and stress factors. Acta Ophthalmol. 2016;94:e312–6. doi:10.1111/aos.12848
7. Taich A, Crowe S, Kosmorsky GS, Traboulsi EI. Prevalence of psychosocial disturbances in children with nonorganic visual loss. J AAPOS. 2004;8:457–461. doi:10.1016/S1091853104001260
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
