Back to Journals » Risk Management and Healthcare Policy » Volume 13
Familial and Environmental Risk Predisposition in Tonsillectomy: A Case–Control Study
Authors Bani-Ata M, Aleshawi A, Alali M , Kanaan Y , Al-Momani W , Kanaan N, Abdalla K , Alhowary A
Received 18 April 2020
Accepted for publication 25 June 2020
Published 21 July 2020 Volume 2020:13 Pages 847—853
DOI https://doi.org/10.2147/RMHP.S258748
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Majid Bani-Ata,1 Abdelwahab Aleshawi,2 Maulla Alali,1 Yazan Kanaan,1 Wala Al-Momani,1 Nadia Kanaan,2 Khalid Abdalla,3 Ala’’a Alhowary4
1Otolaryngology Department, Faculty of Medicine, Jordan University of Science and Technology, Irbid 22110, Jordan; 2Intern, King Abdullah University Hospital, Jordan University of Science and Technology, Irbid 22110, Jordan; 3Radiology Department, Faculty of Medicine, Jordan University of Science and Technology, Irbid 22110, Jordan; 4Anesthesia Department, Faculty of Medicine, Jordan University of Science and Technology, Irbid 22110, Jordan
Correspondence: Majid Bani-Ata
Department of Special Surgery, Jordan University of Science and Technology, P.O. Box: 3030, Irbid 22110, Jordan
Email [email protected]
Background: Tonsillectomy is one of the most commonly performed procedures among children and it is the gold standard management to reduce episodes of tonsillitis and obstructive symptoms. Many studies showed a significantly higher incidence of previous tonsillectomy in the parents and siblings. This study investigated the influence of familial and environmental trends in tonsillectomy.
Methods: Retrospectively, we identified those patients who underwent tonsillectomy (the case group). Also, a control group of participants attending the hospital as visitors who had not undergone tonsillectomy was collected. Both groups are compared using the proper statistical tests.
Results: This study included 1,232 participants; 615 underwent tonsillectomy (cases) and 617 did not (controls). It was found that paternal and maternal history of tonsillectomy, childhood asthma, and daycare attendance are independent factors influencing tonsillectomy in the offspring. Of about 85.4% of fathers who underwent tonsillectomy their children will also have tonsillectomy. Also, regarding the maternal history, 72.5% of offspring will have tonsillectomy if the mothers underwent the procedure.
Conclusion: This study reveals that genetic predisposition factors may have a role for tonsillectomy and its underlying causative indications. Also, it highlights the importance of asthma control in children. Moreover, the role of ethnicity may be minimal due to the similar trend of this study with other studies. Further studies and prospective research are recommended.
Keywords: tonsillectomy, tonsillitis, family history, asthma
Introduction
The tonsils are the lymphatic tissue against pathogens entering through the oral and nasal cavity. This is achieved by their specialized crypt.1 Subsequent immune responses may result in tonsillitis and tonsil enlargement of varying severity, ranging from temporary narrowing of the oropharynx with accompanying tenderness to dysphagia, dyspnea, and sleeping breath disorder. Tonsillectomy is gold standard management to reduce the episodes of tonsillitis and obstructive symptoms.2–5
In addition, tonsillectomy is one of the most commonly performed procedures among children, according to the National Health Stat Report, published in 2017, 289,000 tonsillectomies were performed in children less than 15 years of age.6 Also, in Denmark, it is estimated that 6%–9% of persons under the age of 20 years underwent tonsillectomy.7 The most commonly known two causes for tonsillectomy are infection (recurrent tonsillitis, peritonsillar abscess, tonsillolithiasis, and pharyngotonsillitis), and sleep disordered breathing (primary snoring, obstructive sleep apnea syndrome (OSA)).8,9
Many previous studies showed a significantly higher incidence of previous tonsillectomy and/or adenoidectomy in the parents and siblings of children undergoing tonsillectomy than in a control group.3,10–12 Other authors have suggested that atopy is associated with a higher than normal incidence of upper respiratory tract infection, including tonsillitis.11,12
This study uses a large case–control approach to investigate the influence of familial and environmental trends in tonsillectomy, and to understand the sex distribution for this procedure among Jordanian children. Our study also discusses the relation between childhood asthma and tonsillectomy.
Patients and Methods
This study was conducted at King Abdullah University Hospital, a tertiary care center that is affiliated with the Jordan University of Science and Technology, located in northern Jordan. After obtaining the Institutional Review Board approval, we retrospectively identified those patients who underwent tonsillectomy between January 2015 and October 2018 (the case group) (This period of time represents the period where the documentation was done properly). The following information were obtained: demographics (age, sex), causes and indications for tonsillectomy, presence of asthma, maternal and paternal history of tonsillectomy, number of siblings with tonsillectomy, previous attendance to the daycares and the co-existence smoking in the family. In addition, a control group of participants attending the hospital as visitors who did not undergo tonsillectomy was collected and assessed for the same information.
The included case group comprised patients who underwent tonsillectomy as a single procedure or in combination with another procedure such as adenoidectomy and were in the age group from 1 to 14 years at the operation. Any case of malignancy was excluded. A control group of participants whose parents were attending the hospital as visitors and did not undergo tonsillectomy was collected and assessed for the same previously described information. We included the last child in the family alphabetically for randomization. The indications for tonsillectomy were classified into infectious causes (that include recurrent tonsillitis and peritonsillar abscess), sleeping breathing disorder (includes primary snoring and OSA) and other causes (such as febrile convulsion and dysphagia). Many patients had more than one indication. The medical status was assessed mainly for childhood asthma. Detailed family history was recorded from each patient along with the history of attending daycares within the period of tonsillectomy.
 |
Table 1 Demographic Distribution and Clinical Characteristics |
 |
Table 2 Analysis of Factors Associated with Tonsillectomy |
The age group for the controls is within the period of two standard deviations from the mean age of the case group until the age of 14 (10–14 years). This was performed in order to reduce the possibility of young participants (below ten years) to undergoing tonsillectomy in the future. The same information was collected from the control participants.
Setting
The decision to perform tonsillectomy along with the operation was made by consultant otorhinolaryngologists (ENT surgeons) who follow the same guidelines for the indication of tonsillectomy according to the American Academy of Otolaryngology–Head and Neck Surgery (AAO–HNS) Guidelines for tonsillectomy in children and adolescents.13 Information from case and control was collected blindly by senior otorhinolaryngologists residents from the patients themselves or from their parents. The asthma diagnosis was made by consultant pomologists in our institution.
Statistical Analysis
Data were entered into a spreadsheet. Statistical analyses were performed using IBM SPSS Statistics Software (v.21), 2012. Data were presented as frequency distributions for categorical variables and mean ± standard error of the mean for continuous variables (age). Data was tested at a significance level of 0.05%. Pearson χ2 test was used to investigate the significance of association between categorical variables, while Student’s t-test was applied to examine the significance level for continuous normally distributed variables. The normality of the distribution of data was tested using the Kolmogorov–Smirnov test. If a significant (P<0.05) relationship was found, then a post hoc residual analysis for categorical variables was applied to determine the exact significance between groups for each variable. Binary logistic regression analysis was utilized to study the multiple effect of different variables. The sample size was calculated at the following assumptions: power of analysis of 90%, alpha value of 0.05 and beta value of 0.1, the anticipated incidence for family history was assumed as 15% and 5% for the case and control, respectively. The minimal size was 187 for each group.
Results
Demographics and Patients’ Characteristics (Table 1)
Out of 1,232 participants in this study, 615 underwent tonsillectomy (cases) and 617 did not (controls). Overall. 712 males (57.8%) and 520 (42.2%) females were included. The mean age for the total participants was 6.2 years, and 66 suffered from asthma. Smoking was present in 61.6% of families of participants. About 80% of participants attended daycares. Among patients with tonsillectomies, sleeping breath disorders constituted the most common indication of tonsillectomy as 412 (67%) patients suffered from primary snoring (37.6%) and OSA (29.4%). Recurrent tonsillitis and abscess were presented in 410 patients (66.7%). Other indications such as febrile convulsion was present among 31 patients. Table 1 summarizes the general characteristics of the studied sample.
Family History and Other Factors Affecting the Outcome
It was found that the presence of paternal history of tonsillectomy is significantly associated with the case group. Family history of paternal tonsillectomy was found in 13.5% of the cases but in only 2.1% of the control group (P=0.000). This is similar to the family history of maternal tonsillectomy where 11.9% of cases had a family history of maternal tonsillectomy but only 4.9% of the control group had the maternal history (P=0.000). Similarly, siblings with a history of tonsillectomy significantly affected the chance of tonsillectomy (61% of patients with tonsillectomy did not have sibling history in contrast to 92.5% of the control group). In addition, it was noticed that the presence of childhood asthmas is significantly associated with the case group. Asthma was present in 46 of the case group but only in 20 of the control group (P=0.000). Moreover, attending daycare houses was significantly related in the case group. Furthermore, interestingly, males underwent tonsillectomy significantly more than females (61.3% of patients with tonsillectomy were males). However, smoking did not exhibit any significant association, probably due to the high prevalence of smoking in both groups. In general, the presence of first-degree family history was associated significantly with tonsillectomy in the case group (48.5% of the case group vs 12.6% in the control group). Table 2 summarizes the comparative factors between the cases and controls.
For more detailed analyses, parents' history of tonsillectomy was divided into paternal history, maternal history and combined maternal and paternal history Figure 1. It was revealed that 100% (7 out of 7) of patients had tonsillectomy when both the father and mother had undergone tonsillectomy. Regarding the paternal history, 85.4% of fathers who underwent tonsillectomy; their children will have tonsillectomy. Also, regarding the maternal history, 72.5% of offspring will have tonsillectomy if the mother underwent the procedure. After performing multiple regression analysis, it was found that history of asthma, maternal history of tonsillectomy, paternal history of tonsillectomy and attending daycare are independent factors affecting the case group. The presence of paternal and maternal history of tonsillectomy increase the like-hood of tonsillectomy by 5- and 2.5-fold, respectively. More importantly, the asthmatic history increases the chance of tonsillectomy by 24.5-fold. In addition, attending daycare increases the chance by 5-fold.
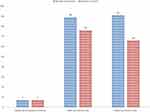 |
Figure 1 Parents history was divided into paternal, maternal history or both. |
When analyzing the indications for tonsillectomy with the related factors, it was revealed that males had more recurrent tonsillitis and females underwent tonsillectomy due to OSA more than males. In addition, no relation was found between family history and the indications except for OSA which is more commonly present with patients with a sibling history of tonsillectomy.
Discussion
In this study, several factors have been reported to influence the frequency of tonsillectomy between children, including the history of childhood asthma, parental history of tonsillectomy, daycare attendance and gender. On the other hand, parental smoking and sibling’s history showed a low significance.
The most significant factor associated with tonsillectomy in this study was having asthma. Frequency of tonsillectomy in children with asthma was 24 times more than those without asthma. Studies about the influence of medical and social history in the incidence of tonsillectomy reported that family history of atopy increased the incidence of tonsillitis.11,12,14 Another study showed that many patients underwent tonsillectomy in order to relieve the signs and symptoms of asthma; however, its effect was temporary or even increased the severity of asthma.15
In our study, parental tonsillectomy history has been reported to significantly increase the chance of tonsillectomy. Children with paternal tonsillectomy history were 5 times more likely to undergo tonsillectomy surgery than those without paternal history, while maternal history increased the risk by 3 times. Similar results were obtained in another study which showed that the incidence of tonsillectomy was increased when there was a parental history with a threefold difference when one parent is concerned and a fourfold when both parents underwent the operation.16 This result was explained previously by the similarities of the lifestyle and the environmental factors of parents and their children. Also, attitudinal factors of parents may also play a role, because parents who the benefitted from tonsillectomy, preferred their children to undergo this procedure earlier.14
Regarding genetic role, Bager et al3 recently highlighted the role of genetic factors in tonsillectomy. They reported that genetic factors predispose to severe tonsillitis underlying tonsillectomy, regardless of age and sex. Immune responses to infections may be attributed to a degree of genetic control as demonstrated by the role of the CCR5 gene in controlling the acquired immunodeficiency syndrome and the role of the mannose-binding lectin gene in controlling effective responses to infant infections.3,17,18 Regarding tonsillitis infection, two studies indicate a considerable genetic component underlying recurrent tonsillitis and tonsillectomy.3,19,20 Another study conducted a genome-wide association study (GWAS) of tonsillectomy (~3,000 cases) and identified and replicated an association between a genetic variant in the gene HORMAD2 and tonsillectomy.21
The results of this study showed that the prevalence of tonsillectomy among males was higher than those of females. These results contrast with a study which took place in Denmark from 1980 to 2001, and reported that cumulative risk of tonsillectomy during the first 20 years of life for females is higher than those of males.7 Studying a wider age group may show different incidence among different age groups.
Participants who attend daycare are reported to be at higher risk of tonsillectomy, this may be attributed to the fact that children in the daycare are more prone to contagious infections which leads to recurrent tonsillitis. This result is in agreement with results in a study from the city São Paulo which suggested that nursery schools may represent a risk factor for colonization of oropharynx by Streptococcus pyogenes.22
This study revealed that parental smoking was insignificantly related to tonsillectomy. This may be attributed to the high prevalence of smoking in approximately every house in Jordan.23 Studying passive smoking in the home environment may give more accurate results. A study of parental cigarette smoking and tonsillectomy in children reported that encouraging parents to stop smoking in the home environment will lead to a decrease in the incidence of tonsillitis and tonsillectomy.24
One study stated that the indications for tonsillectomy were sleep apnea, 22.2%, followed by peritonsillar abscess, 14.8%, and sleep disordered breathing, 14.8%.25 The cause of tonsillar disease was associated with the age of the patient in that tonsillar hyperplasia was the most frequent cause in children younger than 10 years, while in teenagers the cause of tonsillar disease was most frequently related to abscesses and acute infections, and chronic tonsillitis was the most frequent in individuals older than 20 years.26 In this study, the most clinical indications were recurrent tonsillitis and sleeping problems.
This study may have a similar trend to previous studies. However, its relatively large sample size is a strong point. Also, it is the first study to report such a significant relationship in this region within our race. On the other hand, several limitations points are reported. First, it is a retrospective study that lacks the accuracy of the prospective studies. Second, tonsillectomies often follow trends through the decades, being performed very often at certain time points, and then more seldom in others. This cyclic nature may influence the results.
Conclusion
Our results support the previous data about genetic predisposition factors for tonsillectomy and its underlying causative indications. Also, it highlights the importance of asthma control in children. Moreover, maintaining the infectious control practice in daycare units is crucial to reduce the transmission of infections. Moreover, the similarity of this study that was conducted in Jordan to other studies may indicate no role for ethnicity. Further studies and prospective research are recommended to understand how genes regulate the tonsils’ immune response to infections and to understand the complex environmental, genetic and attitudinal factors influencing this common procedure.
Ethical Approval
Institutional approval was obtained from the Institutional Review Board at Jordan University of Science and Technology. This study was conducted in accordance with the Declaration of Helsinki. There was no need for written consents due to the retrospective nature of the study. We confirm that the privacy of the participants was preserved, and the data was anonymized and maintained with confidentiality. The patient data accessed complied with relevant data protection and privacy regulations.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Perry ME. The specialised structure of crypt epithelium in the human palatine tonsil and its functional significance. J Anat. 1994;185(Pt 1):111–127.
2. Burton MJ, Glasziou PP, Chong LY, Venekamp RP. Tonsillectomy or adenotonsillectomy versus non-surgical treatment for chronic/recurrent acute tonsillitis. Cochrane Database Syst Rev. 2014;11:CD001802.
3. Bager P, Corn G, Wohlfahrt J, Boyd HA, Feenstra B, Melbye M. Familial aggregation of tonsillectomy in early childhood and adolescence. Clin Epidemiol. 2018;10:97–105. doi:10.2147/CLEP.S148575
4. Mitka M. Guideline cites appropriateness criteria for performing tonsillectomy in children. JAMA. 2011;305(7):661–662. doi:10.1001/jama.2011.118
5. Georgalas CC, Tolley NS, Narula PA. Tonsillitis. BMJ Clin Evid. 2014;2014:0503.
6. Erickson BK, Larson DR, St Sauver JL, Meverden RA, Orvidas LJ. Changes in incidence and indications of tonsillectomy and adenotonsillectomy, 1970-2005. Otolaryngol Head Neck Surg. 2009;140(6):894–901. doi:10.1016/j.otohns.2009.01.044
7. Vestergaard H, Wohlfahrt J, Westergaard T, Pipper C, Rasmussen N, Melbye M. Incidence of tonsillectomy in Denmark, 1980 to 2001. Pediatr Infect Dis J. 2007;26(12):1117–1121. doi:10.1097/INF.0b013e31814536ba
8. Darrow DH, Siemens C. Indications for tonsillectomy and adenoidectomy. Laryngoscope. 2002;112(8pt 2 suppl 100):6–10. doi:10.1002/lary.5541121404
9. Discolo CM, Darrow DH, Koltai PJ. Infectious indications for tonsillectomy. Pediatr Clin North Am. 2003;50(2):445–58.1. doi:10.1016/S0031-3955(03)00030-0
10. Domenighetti G, Bisig BE. Tonsillectomy: a family-transmissible surgical procedure. Lancet. 1995;346(8986):1376. doi:10.1016/S0140-6736(95)92395-0
11. Clein NW. Influence of tonsillectomy and adenoidectomy on children with specific reference to the allergic implications on respiratory symptoms. Ann Allergy. 1952;5:568–573.
12. Stool SE. Diseases of the tonsils and adenoids in relation to rhinitis and sinusitis. Workshop on tonsillectomy and adenoidectomy. Ann Otol Rhinol Laryngol. 1975;84(Suppl. 19):73–74. doi:10.1177/0003489475084S1916
13. Randel A. AAO-HNS guidelines for tonsillectomy in children and adolescents. Am Fam Physician. 2011;84(5):566–573.
14. Capper R, Canter RJ. Is the incidence of tonsillectomy influenced by the family medical or social history? Clin Otolaryngol Allied Sci. 2001;26(6):484–487. doi:10.1046/j.1365-2273.2001.00508.x
15. Peshkin MM. Asthma in children: III. The incidence and significance of various diseases and infections, and of tonsillectomy and adenoidectomy. Am J Dis Child. 1927;33(6):880–894. doi:10.1001/archpedi.1927.04130180015002
16. Katznelson D, Gross S. Familial clustering of tonsillectomies and adenoidectomies. Clin Pediatr (Phila). 1980;19(4):276–283. doi:10.1177/000992288001900409
17. Stephenson J. Studies probe new anti-HIV strategy, long-term success of prevention methods. JAMA. 2011;305(14):1397–1399. doi:10.1001/jama.2011.433
18. Koch A, Melbye M, Sorensen P, et al. Acute respiratory tract infections and mannose-binding lectin insufficiency during early childhood. JAMA. 2001;285(10):1316–1321. doi:10.1001/jama.285.10.1316
19. Kvestad E, Kvaerner KJ, Roysamb E, Tambs K, Harris JR, Magnus P. Heritability of recurrent tonsillitis. Archiv Otolaryngol Head Neck Surg. 2005;131(5):383–387. doi:10.1001/archotol.131.5.383
20. Martin NG, Kehren U, Battistutta D, Mathews JD. Iatrogenic influences on the heritability of childhood tonsillectomy: cohort differences in twin concordance. Acta Genet Med Gemellol (Roma). 1991;40(2):165–172. doi:10.1017/S0001566000002609
21. Feenstra B, Bager P, Liu X, et al. Genome-wide association study identifies variants in HORMAD2 associated with tonsillectomy. J Med Genet. 2017;54(5):358–364. doi:10.1136/jmedgenet-2016-104304
22. Vieira FM, Figueiredo CR, Soares MC, et al. Prevalence of Streptococcus pyogenes as an oropharynx colonizer in children attending daycare: a comparative study of different regions in Brazil. Braz J Otorhinolaryngol. 2006;72(5):587–591. doi:10.1016/S1808-8694(15)31013-2
23. Abughosh S, Wu IH, Hawari F, et al. Cigarette smoking among Jordanian adults. J Ethn Subst Abuse. 2012;11(2):101–112. doi:10.1080/15332640.2012.674888
24. Hinton AE, Herdman RC, Martin-Hirsch D, Saeed SR. Parental cigarette smoking and tonsillectomy in children. Clin Otolaryngol Allied Sci. 1993;18(3):178–180. doi:10.1111/j.1365-2273.1993.tb00824.x
25. Šumilo D, Nichols L, Ryan R, Marshall T. Incidence of indications for tonsillectomy and frequency of evidence-based surgery: a 12-year retrospective cohort study of primary care electronic records. Br J Gen Pract. 2019;69(678):e33–e41. doi:10.3399/bjgp18X699833
26. Mattila PS, Tahkokallio O, Tarkkanen J, Pitkäniemi J, Karvonen M, Tuomilehto J. Causes of tonsillar disease and frequency of tonsillectomy operations. Arch Otolaryngol Head Neck Surg. 2001;127(1):37–44. doi:10.1001/archotol.127.1.37
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
