Back to Journals » Clinical Ophthalmology » Volume 11
Evaluating intraocular pressure-lowering solutions for the treatment of open-angle glaucoma: comparison between bimatoprost 0.03% and bimatoprost 0.01% – an observational switch study
Authors Deshpande SS, Sonty S, Ahmad A
Received 20 March 2017
Accepted for publication 3 June 2017
Published 27 July 2017 Volume 2017:11 Pages 1371—1376
DOI https://doi.org/10.2147/OPTH.S137537
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sarita S Deshpande,1 Sriram Sonty,1,2 Afzal Ahmad1
1Glaucoma Section, Midwest Eye Center, Calumet City, 2Glaucoma Section, Department of Ophthalmology, University of Illinois at Chicago, Chicago, IL, USA
Purpose: The purpose of this study is to evaluate the intraocular pressure (IOP)-lowering efficacy of bimatoprost 0.01% solution in patients with primary open-angle glaucoma (POAG), who were switched from bimatoprost 0.03% solution, compared to patients with POAG who continued on bimatoprost 0.03% solution.
Methods: A retrospective review evaluated 35 patients (35 right eyes [OD], 34 left eyes [OS]) who remained on bimatoprost 0.03% and 30 patients (27 OD, 30 OS) who were switched to bimatoprost 0.01% during the period January 8, 2010 to December 26, 2012. Mean IOP was measured 6 and 3 months before the switch, at switch, and 3, 6, and 12 months after the switch. Hyperemia scores were recorded before and after the switch and were compared to a picture scale.
Results: Mean IOP in the group that switched was 16.96±5.03 mmHg in OD and 17.67±5.33 mmHg in OS at baseline. Mean IOP postswitch to bimatoprost 0.01% solution was 17.60±4.34 mmHg in OD and 17.00±3.37 mmHg in OS. IOP was not significantly reduced in either OD or OS postswitch to bimatoprost 0.01% (P1=0.5 OD, P2=0.2 OS). The hyperemia scores improved remarkably when bimatoprost 0.03% solution was switched to bimatoprost 0.01% solution (P<0.001).
Conclusion: To our knowledge, this is the first switch study evaluating the hypotensive efficacy and tolerability of bimatoprost in a group of patients with open-angle glaucoma. In this study comparing bimatoprost 0.03% and 0.01% solution, we found improved tolerability postswitch to 0.01% from 0.03% bimatoprost, similar efficacy between the two concentrations before and after switch in the same patient population, and similar IOPs comparable to nonswitch bimatoprost 0.03% solution.
Keywords: bimatoprost, open-angle glaucoma, hyperemia, intraocular pressure
Introduction
More than 80 million people worldwide will be affected by glaucoma by 2020.1 Pharmacologic treatment options to lower intraocular pressure (IOP) are the current first-line therapy for the most common of the glaucoma subcategories, including primary open-angle glaucoma (POAG). Among the potential pharmacologic treatments, the prostaglandin class of drugs has become the preferred option.
Most prostaglandin mimetics appear to affect a hypotensive response by remodeling the extracellular matrix of the ciliary body, thereby enhancing uveoscleral outflow.2,3 Bimatoprost is a unique prostaglandin in that it also interacts with the trabecular meshwork to increase outflow facility.4 Thus, bimatoprost has a dual mechanism of action whereby it lowers IOP by acting on both the pressure-sensitive and pressure-insensitive outflow pathways.5 Short-term comparative studies of the IOP-lowering effect of prostaglandins latanoprost, travoprost, and bimatoprost have shown statistical similarity and, in some cases, a superior effect with bimatoprost.6–9
However, it is often the case in clinical practice that a single agent is unable to provide adequate IOP lowering over the long-term. If/when that occurs, clinicians typically add an adjunctive IOP-lowering agent that belongs to another class or switch the patient to one or more agents from the same class.10 While some short-term studies have shown improved IOP lowering when patients who had a poor initial IOP-lowering response to latanoprost were switched to bimatoprost,11–13 long-term data are scarce. Bimatoprost 0.03% is well accepted as an effective agent, but it has a high rate of hyperemia.14–19 Katz et al14 have shown that bimatoprost 0.01% was equally potent in lowering IOP in a parallel comparative study, while decreasing the rate of hyperemia. Clinical trials comparing bimatoprost 0.01% to bimatoprost 0.03% and other ocular hypotensive agents have found uniform acceptance by patients.17,20–27 However, to date, there is no published study evaluating the hypotensive efficacy in the same group of patients with glaucoma who have been switched from bimatoprost 0.03% to bimatoprost 0.01% and compared to those who remained on bimatoprost 0.03%. In this study, we evaluated for the first time the long-term IOP-lowering efficacy in patients switched from 0.03% to 0.01% and compared it to that of nonswitch patients.
Methods
This is a retrospective study comparing the hypotensive efficacy of two concentrations (0.03% and 0.01%) of bimatoprost in patients with POAG. We identified retrospectively, from electronic medical records, 30 patients with POAG who were switched from bimatoprost 0.03% to 0.01% and 35 patients who were maintained on bimatoprost 0.03% care from January 8, 2010 to December 26, 2012 at our institution. Group 1 consisted of patients with mild glaucoma who were switched from bimatoprost 0.03% to 0.01% (n=30). Group 2 consisted of patients who had moderate to severe glaucoma, and continued to be maintained on bimatoprost 0.03% (n=35). The severity of glaucoma was determined using our own classification system, based on Humphrey visual field status: mild =+1 to −5 dB, moderate =−6 to −15 dB, and severe =−16 dB and worse. The main outcome measures were mean IOP measured with applanation tonometry 6 and 3 months before switch, at switch, and 3, 6, and 12 months after the switch to 0.01%. The type of applanation tonometry used was that of Goldman attached to Haag-Streit slit lamp. The hyperemia scores were graded as: no hyperemia = Grade 0, mild hyperemia = Grade 1, moderate hyperemia = Grade 2, and severe hyperemia = Grade 3, compared to a picture scale. Safety outcomes included discontinuation of bimatoprost and reasons for discontinuation.
All patients included in this study signed an “Authorization and Consent to Disclose Medical Information” form. In our practice, we routinely obtain written informed consent from our patients to use information from their medical records for clinical research in accordance with the regulations of the Health Insurance Portability and Accountability Act. Thus, no separate investigational review board approval was deemed necessary for this study.
Inclusion criteria
Patients with POAG who switched from bimatoprost 0.03% solution to bimatoprost 0.01% solution with follow-up records of at least 6 months were included in this study. IOP measurements were collected at 6 and 3 months before the switch, at switch, and 3, 6, and 12 months after the switch to bimatoprost 0.01%.
Exclusion criteria
Patients were excluded from the analysis if they did not have follow-up records of 6 and 3 months before switching and 3, 6, and 12 months after switching from bimatoprost 0.03% to bimatoprost 0.01%.
Statistical analyses
Data were analyzed using Microsoft Office Excel 2010 Software (Microsoft Corp., Edmond, WA, USA) and GraphPad Prism (GraphPad Software Inc., La Jolla, CA, USA). Distribution of variables is given as mean, standard deviation, and ranges. For accurate statistical analyses, OD and OS were analyzed separately in order to avoid between-eye correlations. Data are presented as the mean IOP ± standard deviation. Statistical significance was determined using a paired t-test to study the difference in the mean values of IOP between pre- and postswitch. Statistical significance between groups 1 and 2 was determined using unpaired t-test. Statistical significance was set at P<0.05.
Results
The study sample consisted of 65 patients (30 patients who switched from bimatoprost 0.03% to bimatoprost 0.01% – Group 1 [27 right eyes {OD}, 30 left eyes {OS}] and 35 patients who were maintained on 0.03% – Group 2 [35 right eyes {OD}, 34 left eyes {OS}]). There were 40 patients in the nonswitch group to start with, but 5 patients were excluded from the study because there was not enough follow-up data. So, the total number of patients in the nonswitch group was 35. The total number of patients in the switch group was 30. These patients fit the study criteria after review, and data were collected from their medical records for analyses.
Both groups had similar characteristics. There were a total of 44 females and 21 males with a mean age of 70 years (range: 48.0–94 years). The mean age in Group 1 was 71 years (range: 48–93 years) and in Group 2 was 69 years (range: 45–94 years). The percentage of males to females was 29% versus 70%, respectively, in Group 1 and 34% versus 66%, respectively, in Group 2. Seventy percent of patients in Group 1 were African Americans versus 77% in Group 2. There were 26% whites in Group 1, compared to 23% in Group 2. Three percent of the patients in Group 1 were Hispanics. There were no Hispanics in Group 2. Baseline characteristics are depicted in Table 1.
  | Table 1 Baseline characteristics of patients |
Approximately 67% of the switched patients (n=18) were on bimatoprost monotherapy. The remainder of the patients were using bimatoprost and at least one adjunctive such as brimonidine, dorzolamide, and timolol. Patients continued concurrent use of adjunctive medications after the switch to bimatoprost 0.01%.
Efficacy
Mean IOP prior to switch from bimatoprost 0.03% to bimatoprost 0.01% (Group 1) was 16.96±5.03 mmHg in OD and 17.67±5.33 mmHg in OS. The mean of nonswitched Group 2 IOP at baseline was 17.40±4.61 mmHg in OD and 17.63±3.97 mmHg in OS. Mean IOP at 12 months after the switch was 17.60±4.34 mmHg in OD and 17.00±3.37 mmHg in OS (Figure 1; Table 2). In the nonswitched group, the mean IOP remained the same. These results provide enough evidence to suggest that there was no significant difference between the lowering efficacy of bimatoprost 0.03% and bimatoprost 0.01% (P1=0.5 OD, P2=0.2 OS). Similarly, mean IOP pre- and postswitch data show noninferiority of bimatoprost 0.01% solution compared to bimatoprost 0.03% solution.
  | Table 2 Mean and range of IOP for switch and nonswitch groups at various time points |
African American patients had preswitch mean IOPs of 16.181±3.79 mmHg OD and 16.71±3.23 mmHg OS, whereas the postswitch mean IOPs were 16.43±3.93 mmHg OD and 15.92±3.38 mmHg OS, and the differences were not statistically significant (P1=0.6 OD, P2=0.2 OS). African American patients in the nonswitch group had average IOPs of 17.17±4.59 mmHg OD and 17.44±5.43 mmHg OS. Caucasian patients had preswitch mean IOPs of 18.41±7.55 mmHg OD and 19.19±7.89 mmHg OS, comparable to postswitch mean IOPs, which were 17.75±6.44 mmHg OD and 18.0±6.06 mmHg OS (P1=0.37 OD, P2=0.29 OS). Caucasian patients in the nonswitch group had mean IOPs of 19.91±3.61 mmHg OD and 18.18±2.62 mmHg OS.
Between the two races, African American patients who switched from bimatoprost 0.03% monotherapy to bimatoprost 0.01% monotherapy had lower IOP readings postswitch, when compared to Caucasian patients who switched from bimatoprost 0.03% to bimatoprost 0.01% monotherapy. These differences were not statistically significant.
Tolerability
Preswitch to 0.01%, there were no patients exhibiting Grade 0 on the hyperemia scale. Four patients exhibited Grade 1, 21 patients showed Grade 2, and 4 patients showed Grade 3 hyperemia. Hyperemia was not recorded for one patient. Postswitch to bimatoprost 0.01% solution, the hyperemia scores showed no patient exhibiting Grade 0, 24 patients with Grade 1, 3 patients with Grade 2, and 2 patients with Grade 3 hyperemia, indicating a shift toward less hyperemia after using bimatoprost 0.01%. There was a significant difference between the hyperemia scores of pre- and postswitch patients (P<0.001). The average preswitch hyperemia score was 2.0, and the average postswitch hyperemia score was 1.24. This shows that 0.01% bimatoprost is more tolerable than 0.03% bimatoprost (Table 3). Patients in the nonswitched Group 2 on bimatoprost 0.03% did not show any change in the hyperemia scores, as expected (P>0.05).
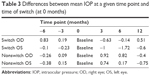  | Table 3 Differences between mean IOP at a given time point and time of switch (at 0 months) |
Discussion
In our study, we found a similar IOP-lowering effect between bimatoprost 0.01% and bimatoprost 0.03% in those patients who were switched. It is generally accepted in clinical practice that medication compliance is better in Caucasians than in African Americans, and theories range from a difference in socioeconomics to intentional nonadherence if hyperemia is considered too obvious. In our study, improved compliance, regression to the mean, or a Hawthorne effect28 may have contributed to the long-term IOP-lowering effect with bimatoprost 0.01% solution compared to bimatoprost 0.03% solution. It is possible that the immediate positive hypotensive response at 3 months could be due to adherence to the medication. However, it is important to note that the goal of this study is to show that 0.01% bimatoprost is as efficacious as 0.03% bimatoprost, with better hyperemic rates. Earlier studies have found a sustained long-term IOP-lowering capability of bimatoprost when used as monotherapy in treatment-naïve glaucoma patients.29 This study suggests that significant sustained long-term IOP lowering also occurs after switching from bimatoprost 0.03% to bimatoprost 0.01% solution, either as monotherapy or as part of an adjunctive therapy mix.
The prostaglandin class agents have a similar adverse effect profile, but the frequency of side effects varies from drug to drug.8,14 For example, Parrish et al9 found latanoprost had a higher ocular tolerability than bimatoprost. However, in our study, there was no discontinuation due to hyperemia or other side effects. In our switch group, we observed an increase in the number of mild ocular hyperemia cases (Grade 1) and a decrease in moderate and severe ocular hyperemia cases (grades 2 and 3) following switch from 0.03% to 0.01% bimatoprost. The results of our study corroborate with those of Katz et al,14 who also reported a reduction in the number of moderate ocular hyperemia cases and an increase in mild ocular hyperemia cases in their study comparing 0.03% with 0.01% bimatoprost, indicating a greater tolerability to the lower concentration (0.01%). Although we did not include a patient survey, anecdotally, our patients liked the switch due to continued efficacy and better tolerability (less hyperemia) of bimatoprost 0.01% solution.
Sonty et al30 previously showed bimatoprost 0.03% to be an effective alternative for patients in whom latanoprost was considered ineffective. While additional long-term prospective studies are called for to confirm the findings of our small retrospective study, our results support switching patients from the higher concentration bimatoprost 0.03% solution to bimatoprost 0.01% solution before switching to a new class agent, or before switching classes or treatment strategies. Our study adds to the literature about similar efficacy and improved tolerability between the two formulations of bimatoprost.14,17,20–27
Conclusion
This first observational retrospective switch study of bimatoprost from 0.03% to 0.01% within the same POAG patient population has shown similar IOP-lowering efficacy and improved tolerability. Patients who were in the bimatoprost 0.01% arm showed similar IOPs after 12 months to patients who were maintained on bimatoprost 0.03%. The patients who switched from bimatoprost 0.03% to bimatoprost 0.01% showed improved hyperemia scores. This switch study indicates that 0.01% may be considered an improved IOP-lowering concentration of bimatoprost in the treatment of POAG.
Acknowledgments
The authors thank Michelle Dalton ELS and Vasantha Reddi PhD for preparing the manuscript and editorial services, which was funded by Allergan. Allergan funded publication of this study.
Disclosure
Sriram Sonty: Alcon (speaker fees, research funds), Allergan (consultant, research funds, speaker fees), Incyte (research funds), Innopharma (research funds). The other authors report no conflicts of interest in this work.
References
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–267. | ||
Lindsey JD, Kashiwagi K, Kashiwagi F, Weinreb RN. Prostaglandins alter extracellular matrix adjacent to human ciliary muscle cells in vitro. Invest Ophthalmol Vis Sci. 1997;38(11):2214–2223. | ||
Weinreb RN, Lindsey JD. Metalloproteinase gene transcription in human ciliary muscle cells with latanoprost. Invest Ophthalmol Vis Sci. 2002;43(3):716–722. | ||
Wan Z, Woodward DF, Cornell CL, et al. Bimatoprost, prostamide activity, and conventional drainage. Invest Ophthalmol Vis Sci. 2007;48(9):4107–4115. | ||
Brubaker RF. Mechanism of action of bimatoprost (Lumigan). Surv Ophthalmol. 2001;45(Suppl 4):S347–S351. | ||
Walters TR, DuBiner HB, Carpenter SP, Khan B, VanDenburgh AM; Bimatoprost Circadian IOP Study Group. 24-Hour IOP control with once-daily bimatoprost, timolol gel-forming solution, or latanoprost: a 1-month, randomized, comparative clinical trial. Surv Ophthalmol. 2004;49(Suppl 1):S26–S35. | ||
Noecker RS, Dirks MS, Choplin NT, Bernstein P, Batoosingh AL, Whitcup SM; Bimatoprost/Latanoprost Study Group. A six-month randomized clinical trial comparing the intraocular pressure-lowering efficacy of bimatoprost and latanoprost in patients with ocular hypertension or glaucoma. Am J Ophthalmol. 2003;135(1):55–63. | ||
Gandolfi S, Simmons ST, Sturm R, Chen K, VanDenburgh AM; Bimatoprost Study Group 3. Three-month comparison of bimatoprost and latanoprost in patients with glaucoma and ocular hypertension. Adv Ther. 2001;18(3):110–121. | ||
Parrish RK, Palmberg P, Sheu WP, Group XLTS. A comparison of latanoprost, bimatoprost, and travoprost in patients with elevated intraocular pressure: a 12-week, randomized, masked-evaluator multicenter study. Am J Ophthalmol. 2003;135(5):688–703. | ||
Martinez A, Sanchez M. Intraocular pressure lowering effect of dorzolamide/timolol fixed combination in patients with glaucoma who were unresponsive to prostaglandin analogs/prostamides. Curr Med Res Opin. 2007;23(3):595–599. | ||
Williams RD. Efficacy of bimatoprost in glaucoma and ocular hypertension unresponsive to latanoprost. Adv Ther. 2002;19(6):275–281. | ||
Gandolfi SA, Cimino L. Effect of bimatoprost on patients with primary open-angle glaucoma or ocular hypertension who are nonresponders to latanoprost. Ophthalmology. 2003;110(3):609–614. | ||
Nakamura T, Yamada M, Teshima M, et al. Electrophysiological characterization of tight junctional pathway of rabbit cornea treated with ophthalmic ingredients. Biol Pharm Bull. 2007;30(12):2360–2364. | ||
Katz LJ, Cohen JS, Batoosingh AL, Felix C, Shu V, Schiffman RM. Twelve-month, randomized, controlled trial of bimatoprost 0.01%, 0.0125%, and 0.03% in patients with glaucoma or ocular hypertension. Am J Ophthalmol. 2010;149(4):661–671.e1. | ||
Campbell JH, Schwartz G, Labounty B, Kowalski J, Patel VD. Comparison of adherence and persistence with bimatoprost 0.01% versus bimatoprost 0.03% topical ophthalmic solutions. Curr Med Res Opin. 2013;29(9):1201–1209. | ||
Figus M, Nardi M, Piaggi P, et al. Bimatoprost 0.01% versus bimatoprost 0.03%: a 12-month prospective trial of clinical and in vivo confocal microscopy in glaucoma patients. Eye (Lond). 2014;28(4):422–429. | ||
Myers JS, Vold S, Zaman F, Williams JM, Hollander DA. Bimatoprost 0.01% or 0.03% in patients with glaucoma or ocular hypertension previously treated with latanoprost: two randomized 12-week trials. Clin Ophthalmol. 2014;8:643–652. | ||
Ogundele AB, Li G, Ellis JJ. Impact of topical bimatoprost 0.01% and bimatoprost 0.03% on conjunctival irritation in rabbits. Clin Ophthalmol. 2010;4:77–80. | ||
Wong WB, Patel VD, Kowalski JW, Schwartz G. An adherence based cost-consequence model comparing bimatoprost 0.01% to bimatoprost 0.03%. Curr Med Res Opin. 2013;29(9):1191–1200. | ||
Kook MS, Simonyi S, Sohn YH, Kim CY, Park KH. Bimatoprost 0.01% for previously treated patients with open-angle glaucoma or ocular hypertension in the Korean clinical setting. Jpn J Ophthalmol. 2015;59(5):325–334. | ||
Park KH, Simonyi S, Kim CY, Sohn YH, Kook MS. Bimatoprost 0.01% in treatment-naive patients with open-angle glaucoma or ocular hypertension: an observational study in the Korean clinical setting. BMC Ophthalmol. 2014;14:160. | ||
DuBiner HB, Hubatsch DA. Late-day intraocular pressure-lowering efficacy and tolerability of travoprost 0.004% versus bimatoprost 0.01% in patients with open-angle glaucoma or ocular hypertension: a randomized trial. BMC Ophthalmol. 2014;14:151. | ||
Crichton AC, Nixon DR, Simonyi S, et al. An observational study of bimatoprost 0.01% in patients on prior intraocular pressure-lowering therapy: the Canadian Lumigan(®) RC Early Analysis Review (CLEAR) trial. Clin Ophthalmol. 2014;8:1031–1038. | ||
Campbell JH, Schwartz GF, LaBounty B, Kowalski JW, Patel VD. Patient adherence and persistence with topical ocular hypotensive therapy in real-world practice: a comparison of bimatoprost 0.01% and travoprost Z 0.004% ophthalmic solutions. Clin Ophthalmol. 2014;8:927–935. | ||
Nixon DR. A randomized, prospective study of bimatoprost 0.01% or travoprost/timolol in patients previously treated with latanoprost and timolol to reduce intraocular pressure. J Ocul Pharmacol Ther. 2013;29(10):876–881. | ||
Nixon DR, Simonyi S, Bhogal M, et al. An observational study of bimatoprost 0.01% in treatment-naive patients with primary open angle glaucoma or ocular hypertension: the CLEAR trial. Clin Ophthalmol. 2012;6:2097–2103. | ||
Pfennigsdorf S, Ramez O, von Kistowski G, et al. Multicenter, prospective, open-label, observational study of bimatoprost 0.01% in patients with primary open-angle glaucoma or ocular hypertension. Clin Ophthalmol. 2012;6:739–746. | ||
McCarney R, Warner J, Iliffe S, van Haselen R, Griffin M, Fisher P. The Hawthorne Effect: a randomised, controlled trial. BMC Med Res Methodol. 2007;7:30. | ||
Gupta V, Srinivasan G, Sharma A, Kapoor KS, Sihota R. Comparative evaluation of bimatoprost monotherapy in primary chronic angle closure and primary open angle glaucoma eyes: a three-year study. J Ocul Pharmacol Ther. 2007;23(4):351–358. | ||
Sonty S, Donthamsetti V, Vangipuram G, Ahmad A. Long-term IOP lowering with bimatoprost in open-angle glaucoma patients poorly responsive to latanoprost. J Ocul Pharmacol Ther. 2008;24(5):517–520. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

