Back to Journals » Patient Preference and Adherence » Volume 10
Ethical considerations in adherence research
Authors Patel NU, Moore BA, Craver RF, Feldman SR
Received 21 July 2016
Accepted for publication 11 October 2016
Published 5 December 2016 Volume 2016:10 Pages 2429—2435
DOI https://doi.org/10.2147/PPA.S117802
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Video abstract presented by Nupur U Patel.
Views: 803
Nupur U Patel,1 Blake A Moore,1 Rebekah F Craver,2 Steven R Feldman1,2
1Department of Dermatology, Center for Dermatology Research, 2Department of Public Health Sciences, Wake Forest University School of Medicine, Winston-Salem, NC, USA
Abstract: Poor adherence to treatment is a common cause of medical treatment failure. Studying adherence is complicated by the potential for the study environment to impact adherence behavior. Studies performed without informing patients about adherence monitoring must balance the risks of deception against the potential benefits of the knowledge to be gained. Ethically monitoring a patient’s adherence to a treatment plan without full disclosure of the monitoring plan requires protecting the patient’s rights and upholding the fiduciary obligations of the investigator. Adherence monitoring can utilize different levels of deception varying from stealth monitoring, debriefing after the study while informing the subject that some information had been withheld in regard to the use of adherence monitoring (withholding), informed consent that discloses some form of adherence monitoring is being used and will be disclosed at the end of the study (authorized deception), and full disclosure. Different approaches offer different benefits and potential pitfalls. The approach used must balance the risk of nondisclosure against the potential for confounding the adherence monitoring data and the potential benefits that adherence monitoring data will have for the research subjects and/or other populations. This commentary aims to define various methods of adherence monitoring and to provide a discussion of the ethical considerations that accompany the use of each method and adherence monitoring in general as it is used in clinical research.
Keywords: compliance, stealth monitoring, deception, adherence monitoring
Introduction
Adherence to a prescribed treatment is important for the success of any therapeutic intervention. Defined by the World Health Organization as “the degree to which the person’s behavior corresponds with the agreed recommendations from a health care provider,” adherence has become the focus of much clinical research.1 In recent years, the term adherence has come to supersede that of compliance in the literature.2 The term compliance was defined in the 1970s as “the extent to which a person’s behavior (in terms of taking medications, following diets, or executing lifestyle changes) coincides with medical or health advice.”3,4 It can also be defined as “the extent to which the patient’s behavior follows the prescribed recommendations.”5 A third term, concordance, is defined by the Royal Pharmaceutical Society of Great Britain as an agreement between patient and health care professional, which takes into account the beliefs and wishes of the patient in determining how their medication is taken.2 Although these terms are similarly defined and oftentimes used interchangeably, they differ in their implied meanings.1 Concordance refers to successful partnership in which the patient is supported in their decisions about their medicine.6 While compliance denotes patient obedience in following orders given by the physician in a position of authority, adherence indicates collaboration between physician and patient that takes into account medical knowledge along with patient preferences to improve patient health.1,7 Adherence suggests that the patients have decided to act of their own free will when they follow through with the suggestions made by their physician.7
Nonadherence involves any deviation of the prescribed regimen, including excessive, insufficient, or inconsistent dosing practices. Nonadherence is associated with poor treatment outcomes and a lower quality of life.8 Nonadherence can lead the unknowing clinician to more risky and costly methods of treatment. As much as two-thirds of hospital admissions related to medications are estimated to result from patient nonadherence.9 Accounting for hospital admissions and unused and unnecessary treatment, the cost of nonadherence is estimated to exceed $100 billion in the US.10 In clinical research, the patient outcomes used to guide future medical interventions are based on the prescribed regimen set forth in the study. If a study drug or treatment being investigated fails, it is important to determine whether this failure is attributable to nonadherence by the research subjects or to the outright failure of the therapy in question.11 In chronic diseases, adherence is increasingly important to help improve long-term therapeutic outcomes.
Adherence monitoring provides insight into patient behavior and facilitates evaluation of the effect of adherence on treatment outcomes. Some of the methods used by researchers for monitoring adherence – including pill counts or medication weight (for topical therapies), medication logs or diaries, and self-reporting – are limited by medication dumping and reporting errors. Measuring blood levels of medication or urinary excretion of the medication or a metabolic by-product is also limited as patients have a tendency to use their medication just before an office visit, a phenomenon termed the white coat effect.12 Electronic monitors that record the date and timing of a medication event by the use of a microprocessor in the medication container avoid many of these limitations and can more accurately record the patient’s adherence to a therapeutic program over an extended period of time.13–15 Adherence research and the development and testing of interventions to improve adherence have tremendous potential for improving treatment outcomes. Such research studies also have ethical implications that must be addressed, particularly if some component of nondisclosure is used to prevent biasing adherence outcomes.
Ethical principles in adherence research
Researchers are responsible for ensuring that their projects meet certain ethical criteria before the investigation begins. Research participants are entitled to information regarding the disclosure of the nature, duration, and exposure involved in the research before accepting and becoming a research participant. Researchers are compelled to minimize the risk and physical injury or emotional suffering.16 The Belmont Report17 outlines the foundational rights of a human research participant: respect for persons with informed consent (autonomy), justice, and beneficence. It serves as a guide to the Institutional Review Board (IRB) for evaluating proposed research projects. Informed consent is defined as the right of the individual to be knowledgeable about the events that shall happen to them as the result of participating in a study. Disclosure required for granting informed consent includes benefits, risks, outcomes, time involved, alternative procedures that may be utilized by the participant, a statement of confidentiality, and contact information for unresolved questions by participants.
The Belmont Report also addresses cases where informed consent could potentially confound investigations. Such exceptions to informed consent are permissible only upon meeting the following criteria: it is necessary to the research goals to withhold information regarding research methods, no undisclosed risks exist except those that are minimally harmful, and a plan for debriefing must follow at the culmination of the research project with plans for distribution of research results.17 Very similar criteria are also outlined in federal regulations that exist (45 CFR 46.116d),18 which allow the IRB to grant a waiver of the informed consent requirements to approve deceptive research that requires the withholding of informed consent.18 In this way, research studies can meet ethical standards while legally allowing the researcher to employ deception or withhold information in the process of conducting the study.
One goal of research investigating adherence is to gather accurate data regarding the nonadherence phenomenon. Therefore, these studies need to mimic clinical scenarios as closely as possible. While adherence data can be collected without deception, the information provided by that study type might not be accurate or useful. If patients are fully aware of adherence monitoring, that knowledge could result in patients modifying their adherence behavior.19 The resulting data may not be informative of the actual adherence behavior of patients, creating the need for study design that involves deception. Thus, the adherence information sought by deception researchers oftentimes cannot be obtained by means other than withholding information from patients.
Withholding information about adherence monitoring from patients raises several ethical concerns. One concern is that withholding information from patients or deceiving them compromises the trusted relationship between doctor and patient, as well as potentially harming the patient emotionally. Inflicted insight is an emotional distress in a participant from the knowledge that they were not honest with the researcher.20 This reaction comes from attempting to mislead the physician or from deviating from prescribed treatment methods during the study. Oftentimes, patients will change their apparent or actual behavior to comply with their physician’s wishes to be considered “good” patients.19 The revelation of previously undisclosed adherence monitoring to the participant might produce emotional distress and subsequent physician mistrust. Critics of deception research hypothesize that physician mistrust following deception studies could contribute to limiting the pool of naive patients in future studies.21 These critics assert that deception involves a violation of trust, with the amount of potential harm increasing as the participants become more reliant upon the investigator.22 In addition, the physician investigator may be emotionally harmed in the use of deception as this runs counter to the traditional role of a physician.22 These ethical concerns must be balanced against potential benefits, including the need to withhold study information to understand patient behavior and improve patients’ treatment outcomes.
Several different forms of nondisclosure can be used in adherence research. Different degrees of nondisclosure are associated with varying risks to the patient and varying benefits to the research subject and society (Table 1).
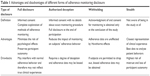  | Table 1 Advantages and disadvantages of different forms of adherence monitoring disclosure |
Full disclosure
Full disclosure is a conservative method that acquires informed consent before the onset of the investigation and provides participants the most comprehensive information regarding the investigation. Any questions the participant may have should be answered prior to obtaining informed consent. Autonomy is upheld. The researcher achieves beneficence such that known risks and benefits are clearly elucidated. With full disclosure, patients in adherence monitoring studies are unlikely to experience emotional distress as the use of deception is disclosed.
This form of disclosure is especially useful in investigations where the risks and therapeutic value of a treatment are not well determined or are unknown. Full disclosure, however, would be problematic in an adherence monitoring study in that true patient behavior could be confounded due to the participant’s knowledge of the adherence monitoring aspect of the investigation.19 Nonadherent subjects might choose to not participate in the study, biasing the outcomes. Moreover, patients may modify their behavior as a result of awareness that investigators are monitoring their adherence. In one study by Rand et al,23 14% of patients being monitored with microprocessing devices discharged their inhalers more than 100 times in the period of 3 hours to demonstrate their compliance with investigator instructions.19 These results strengthen the case against full disclosure, revealing that subjects might act deceptively to falsify their adherence or even genuinely improve their adherence knowing it will be monitored.19 Thus, the use of full disclosure in adherence monitoring studies should be carefully assessed, as it will not provide the most clinically relevant information upon which accurate conclusions regarding actual patient behavior can be drawn.
Partial disclosure
Subjects can be informed they will be monitored, without revealing the complete extent of the monitoring. For example, Carroll et al13 told patients that their use of medication would be monitored and that patients should complete treatment diaries and bring in study medication to be weighed. However, patients were not told that their adherence would be assessed using electronic adherence monitors in the medication caps. By informing patients they would be monitored, some degree of informed consent was obtained, but fully informed consent was not obtained. The conclusions drawn from this study indicated that the medication logs did not ensure adherence, but that electronic monitoring allowed for more accurate measurement of adherence. The partial disclosure approach may have mitigated some of the effects of monitoring on adherence, as the impact of the diary on adherence may have been different from the impact of knowing that adherence was being objectively monitored. The degree of deception used in partial disclosure also raises the potential for emotional distress to the patient when they learn they have been deceived. This raises an important ethical concern for the researcher, who must take into account the risks posed to individual patients versus the benefits that successful completion of the study will provide to the scientific community and patients.
Authorized deception
Authorized deception is a form of monitoring in which the investigator informs the participant that the investigation involves a form of deception that will not be revealed to the participant until the conclusion of the study. Consent could involve informing patients that their adherence will be monitored, but the researcher conceals the particular adherence monitoring method. Because informed consent was obtained that acknowledged that some form of adherence monitoring would occur, participants are better able to determine whether participation in the study is in their own best interest (autonomy). However, the extent to which patients are told they will be monitored may result in changes in patients’ adherence behavior.19,23 Authorized deception creates a scenario in which patients can become distressed due to the level of deception used. There is the potential for inflicted insight to occur when and if patients are debriefed regarding the use of the adherence monitoring methods.
Withholding
In a more radical form of adherence monitoring, investigators obtain a patient’s consent to participate in the study, but patients are not informed that adherence monitoring will be utilized by the investigator, withholding information on adherence monitoring until debriefing at the conclusion of the study.24 Withholding does not result in truly “informed” consent, as patients may be unaware of the very purpose of the investigation. In studies utilizing withholding, autonomy is diminished. Furthermore, withholding has the potential to produce emotional distress in participants during debriefing when the goals of the study are revealed. The use of such an approach would need to be balanced against the potential benefit of obtaining adherence information unbiased by the knowledge of the adherence monitoring.
One approach to minimize the limitations on patient autonomy is to give patients the opportunity to provide informed consent to use adherence data “at the end of study” debriefing.24 Patients may or may not choose to allow their data to be used in the study. This approach allows data to be collected without being biased by knowledge that adherence is being monitored. However, this approach leaves open the possibility of bias if patients choosing not to allow their data to be used are not representative of the group – for example, if they tend to be nonadherent. If a true representation of clinical patient behavior is to be achieved by the study and if the benefits of doing so outweigh the risks, it may be necessary to inform subjects about monitoring without giving subjects the opportunity to withhold their data.25
Stealth monitoring
In scenarios in which it is critical and justifiable to obtain actual clinic patients’ adherence behavior, stealth monitoring can be used. With stealth monitoring, investigations proceed not only without letting patients know about the adherence monitoring but also by collecting data without patients knowing that they are in a study at all.26 Informed consent would not be obtained prior to study onset, and in some cases researchers would find it necessary to prevent study participants from withholding their data should they be uncomfortable with the deceptive monitoring practices at its conclusion. Even acknowledgment of the study may or may not be revealed to the participant, as patient’s withholding data would potentially confound the results, and therefore conclusions regarding actual patient adherence would be impossible to determine. This method uses deception to acquire data that most resembles behavior exhibited by patients in a clinical setting. In stealth monitoring, patients are under the assumption that the treatment is standard medical practice and they are being informally observed merely for outcomes of treatment. As such, stealth monitoring is the most comparable to the clinical environment.
Of most concern in regard to the ethics of stealth monitoring studies is the failure to achieve informed consent and to notify the patients of their participation in a clinical trial before an investigation begins, with the researchers obtaining only verbal consent. Furthermore, preventing patients from opting out of the investigation could also be ethically concerning as it eliminates patient autonomy.27 Furthermore, many critics argue that deception research causes patients unnecessary harm, as well as causing deceived patients to mistrust physicians or to refrain from participating in future studies. Of course, these negative outcomes would run counter to the goals of beneficence and nonmaleficence. The risk of stealth monitoring, however, may be justified if the study treatment is the care the patient would have received anyway and if the potential benefits to the patient and to society of having unbiased adherence information outweigh the risks.
More controversial than adherence monitoring in the research setting is adherence monitoring in the clinical setting. In this case, the autonomous patient could be compromised in that noncompliant patients might suffer consequences from insurance companies or other health care entities on account of personal behavior and choices.28 In transplant patients, health maintenance organizations monitor patient adherence and contact health care providers when treatment falls below desired standards due to the high adherence necessary with immunosuppressive pharmaceuticals for a successful long-term transplant.29 This type of monitoring raises ethical questions about a concept called “medical paternalism”, or the removal of patient autonomy by the health care provider for the greater good of the patient’s health.27 As more methods of adherence monitoring are developed, the medical community will need to further explore the implications of such monitoring in clinical situations.
Discussion
Adherence monitoring studies usually involve limiting the amount of information disclosed to patients at least to some degree. Various levels of disclosure have different advantages and disadvantages. To better understand the actual adherence of patients, the impact of study participation on patients’ behavior must be minimized. To achieve this, it may be best to collect adherence data before informed consent about the monitoring is obtained. After data are collected, patients can be debriefed and consent to use adherence data may or may not be acquired from the participants. In some studies, participants can opt to withhold their data from the researchers if they feel uncomfortable with the research design after debriefing. Again, such an approach may not provide fully representative adherence information if a nonrandom subset of the population refuses to participate. For example, if highly nonadherent subjects refused to allow the use of their adherence data, the study would be biased toward showing higher adherence rates in the study group. In cases where it is critical to determine patients’ adherence behavior, it may be necessary to obtain the adherence information without giving subjects the option to opt out. This degree of deception is not without risk. The revelation of the use of deception and adherence monitoring to the patient has the potential to cause emotional distress from a phenomenon called inflicted insight; such approaches should be used only if the benefits outweigh the risks.
Ethical concerns are important in all research studies, particularly in studies of behavior. Such studies are inherently problematic, because being part of the study can affect the behavior being studied, ie, the Hawthorne effect.19 Human subject research committees must weigh the risks and benefits of withholding information about the study procedures. The Belmont Report guidelines dictate that the investigator must achieve a balance between the three governing principles. While the patient may be displeased that monitoring occurred without permission or acknowledgment, if the physical harms are minimized and undue emotional distress is not expected to result from the experience, then potential benefits from an adherence study designed to improve the subjects’ treatment outcomes and/or generate important general knowledge may outweigh the risks of nondisclosure. The Belmont Report17 requires that studies only minimize the risk and that risk should be outweighed by both anticipated benefit to the patient and benefit to society at large as the result of extending scientific knowledge. Thus, when the study data are sufficiently important and when they cannot be obtained without deception, some degree of withholding or deception with regard to the mechanisms of adherence monitoring may be appropriate.25
Patients may benefit from adherence research in the form of better treatment and outcomes. Individual participants may benefit directly if the study reports their adherence behavior to them and the potential effects of that behavior on their own health. Moreover, considering the implications of poor adherence to treatment, there may be substantial benefits to the general patient population that result from a better understanding of the role of adherence in treatment failures and from the development of interventions that enhance patients’ adherence behavior.15 The potential risks and benefits of adherence research may be challenging to quantify. It is difficult to assess the implications of adherence monitoring on a patient’s emotional status. Even critics acknowledge that potential harms are largely theoretical.22 On the other hand, the potential benefits to developing new treatment strategies that improve adherence behavior are expected to have large benefits on patients’ health and well-being.
Patient adherence is poor in both the clinical and research settings across many medical specialties. Nonadherence is well characterized in many settings, and studies have begun to focus on ways to improve adherence.30–32 Deception in adherence studies are still needed to develop and test new interventions to improve adherence behavior. Such studies may require the highest levels of withholding information to prevent the Hawthorne effect and to prevent participant dropout from biasing the study results. It is critically important that these studies minimize risk and weigh that risk against the potential benefits of the specific study. The insight gained from such investigations will have the potential to lead physicians to more effective and prudent treatment plans that will greatly improve patients’ quality of life.
Acknowledgments
Contents of the manuscript have not been previously published and are not currently submitted elsewhere. The Center for Dermatology Research is supported by an unrestricted educational grant from Galderma Laboratories, LP.
Disclosure
Dr SRF is a speaker for Janssen and Taro. He has received research, speaking and/or consulting support from several companies including Galderma, GSK/Stiefel, Almirall, Leo Pharma, Baxter, Boehringer Ingelheim, Mylan, Celgene, Pfizer, Valeant, Abbvie, Cosmederm, Anacor, Astellas, Janssen, Lilly, Merck, Merz, Novartis, Qurient, National Biological Corporation, Caremark, Advance Medical, Suncare Research, Informa, UpToDate, and National Psoriasis Foundation. He is the founder and majority owner of DrScore.com. He is a founder and part owner of Causa Research, a company dedicated to enhancing patients’ adherence to treatment. The other authors report no conflicts of interest in this work.
References
Jimmy B, Jose J. Patient medication adherence: measures in daily practice. Oman Med J. 2011;26(3):155–159. | ||
Cushing A, Metcalfe R. Optimizing medicines management: from compliance to concordance. Ther Clin Risk Manag. 2007;3(6):1047–1058. | ||
Haynes R, Taylor D, Sackett D, editors. Compliance in Health Care. Baltimore: Johns Hopkins University Press; 1979. | ||
Conrad P. The meaning of medications: another look at compliance. Soc Sci Med. 1985;20(1):29–37. | ||
Chakrabarti S. What’s in a name? Compliance, adherence and concordance in chronic psychiatric disorders. World J Psychiatry. 2014;4(2): 30–36. | ||
De las Cuevas C. Towards a clarification of terminology in medicine taking behavior: compliance, adherence and concordance are related although different terms with different uses. Curr Clin Pharmacol. 2011;6(2):74–77. | ||
Spiro H. Compliance, adherence, and hope. J Clin Gastroenterol. 2001;32(1):5. | ||
Zaghloul SS, Cunliffe WJ, Goodfield MJ. Objective assessment of compliance with treatments in acne. Br J Dermatol. 2005;152(5): 1015–1021. | ||
Munger MA, Van Tassell BW, LaFleur J. Medication nonadherence: an unrecognized cardiovascular risk factor. MedGenMed. 2007; 9(3):58. | ||
Balkrishnan R, Carroll CL, Camacho FT, Feldman SR. Electronic monitoring of medication adherence in skin disease: results of a pilot study. J Am Acad Dermatol. 2003;49(4):651–654. | ||
Koehler AM, Maibach HI. Electronic monitoring in medication adherence measurement. Implications for dermatology. Am J Clin Dermatol. 2001;2(1):7–12. | ||
Feldman SR, Camacho FT, Krejci-Manwaring J, Carroll CL, Balkrishnan R. Adherence to topical therapy increases around the time of office visits. J Am Acad Dermatol. 2007;57(1):81–83. | ||
Carroll CL, Feldman SR, Camacho FT, Manuel JC, Balkrishnan R. Adherence to topical therapy decreases during the course of an 8-week psoriasis clinical trial: commonly used methods of measuring adherence to topical therapy overestimate actual use. J Am Acad Dermatol. 2004;51(2):212–216. | ||
Choo PW, Rand CS, Inui TS, Lee ML, Canning C, Platt R. A cohort study of possible risk factors for over-reporting of antihypertensive adherence. BMC Cardiovasc Disord. 2001;1:6. | ||
Wendel CS, Mohler MJ, Kroesen K, Ampel NM, Gifford AL, Coons SJ. Barriers to use of electronic adherence monitoring in an HIV clinic. Ann Pharmacother. 2001;35(9):1010–1015. | ||
Tikveel W. Trials of War Criminals before the Nuremberg military tribunals under control council law. US Gov Print Off. 1949;2(10):181–182. | ||
National Institutes of Health. The Belmont Report.Belmont Rep Ethical Princ Guidel Prot Hum Subj Res. 1979:4–6. Available from: http://www.hhs.gov/ohrp/regulations-and-policy/belmont-report/. Accessed November 01, 2016. | ||
Health D of Services H. Rules and regulations: protection of human subjects. Title 45, Code of Federal Regulations, part 46. Fed Regist. 1991;56:28003. | ||
Levine RJ. Monitoring for adherence: ethical considerations. Am J Respir Crit Care Med. 1994;149(2 pt 1):287–288. | ||
Levine R. Ethics and Regulation of Clinical Research. New Haven, CT: Yale University Press; 1988. | ||
Emanuel EJ, Grady CC, Crouch RA, Lie RK, Miller FG, Wendler DD [webpage on the Internet]. The Oxford Textbook of Clinical Research Ethics. Oxford University Press; 2008. Available from: https://books.google.com/books?id=vKFYAtcLAxgC. Accessed September 29, 2016. | ||
Wendler D, Miller FG. Deception in the pursuit of science. Arch Intern Med. 2004;164(6):597–600. | ||
Rand CS, Wise RA, Nides M, et al. Metered-dose inhaler adherence in a clinical trial. Am Rev Respir Dis. 1992;146(6):1559–1564. | ||
University of Virginia Institutional Review Board for Social and Behavioral Sciences [webpage on the Internet]. Post-Deception Debriefing Session.Institutional Review Board for Social and Behavioral Sciences. 2016. Available from: http://www.virginia.edu/vpr/irb/sbs/resources_guide_deception_debrief.html. Accessed September 29, 2016. | ||
Authority GL, Demands O, Judgments P, et al. Ethical principles of psychologists and code of conduct. Am Psychol. 2002;57(12): 1060–1073. | ||
Krejci-Manwaring J, Tusa MG, Carroll C, et al. Stealth monitoring of adherence to topical medication: adherence is very poor in children with atopic dermatitis. J Am Acad Dermatol. 2007;56(2):211–216. | ||
Rand CS, Sevick MA. Ethics in adherence promotion and monitoring. Control Clin Trials. 2000;21(5 suppl):241S–247S. | ||
Weinstein AG. Should patients with persistent severe asthma be monitored for medication adherence? Ann Allergy Asthma Immunol. 2005;94(2):251–257. | ||
Morrissey PE, Flynn ML, Lin S. Medication noncompliance and its implications in transplant recipients. Drugs. 2007;67(10):1463–1481. | ||
Ali SM, Brodell RT, Balkrishnan R, Feldman SR. Poor adherence to treatments: a fundamental principle of dermatology. Arch Dermatol. 2007;143(7):912–915. | ||
Baldwin HE. Tricks for improving compliance with acne therapy. Dermatol Ther. 2006;19(4):224–236. | ||
Ou HT, Feldman SR, Balkrishnan R. Understanding and improving treatment adherence in pediatric patients. Semin Cutan Med Surg. 2010;29(2):137–140. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
