Back to Journals » Clinical Ophthalmology » Volume 14
Dry Eye Syndrome and Sicca Complex are Commonly Found in Patients with Postural Orthostatic Tachycardia Syndrome
Authors Ho DS , Vaou OE , Hohler AD
Received 30 August 2020
Accepted for publication 23 October 2020
Published 20 November 2020 Volume 2020:14 Pages 4015—4021
DOI https://doi.org/10.2147/OPTH.S279520
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Dave S Ho,1 Okeanis E Vaou,1,2 Anna D Hohler2
1Neurology, Boston University School of Medicine, Boston, MA, USA; 2Steward Medical Group Neurology, St. Elizabeth’s Medical Center, Brighton, MA, USA
Correspondence: Dave S Ho
Boston University School of Medicine, 1949 Commonwealth Ave, Apt 35, Boston, MA, USA
Tel +1 949 468 8797
Fax +1 617 789 5177
Email [email protected]
Purpose: Patients with postural orthostatic tachycardia syndrome (POTS) present to outpatient dysautonomia clinics endorsing a wide range of symptoms. Dry eyes and mouth, or sicca complex are frequently reported. This retrospective study investigates the incidence and quantifies the severity of dry eye syndrome (DES) in patients with POTS.
Patients and Methods: This retrospective study compiles survey results, and dry eye clinical data from twenty-three POTS patients (22 females, average age 34.9 and st dev 14.0 years) surveyed during their initial or follow-up appointments. Patient’s medication lists were documented to account for anticholinergics, antihistamines, and anticholinesterase use. Patients endorsing dry eye symptoms were tested with Schirmer’s test strips to identify clinically dry eyes and stratified for severity.
Results: Sixty-five percent of patients endorsed dry eye symptoms (15/23). Seventy-four percent of patients endorsed dry mouth symptoms (17/23). Among patients endorsing dry eyes, 81% of eyes had decreased tear production with Schirmer’s strip wetting less than 10 mm/5 min (13/16).
Conclusion: DES is an additional and significant disease burden for the POTS patient population. Dry eye and exocrine gland function should be evaluated as part of the dysautonomia work up with referral to ophthalmology as appropriate. Patients with clinically dry eyes who report additional autonomic dysfunction should be further evaluated for widespread autonomic dysfunction.
Keywords: dry eye syndrome, Sjogren’s disease, keratoconjunctivitis sicca, sicca complex, POTS, dysautonomia
Introduction
Dry Eye Syndrome (DES), Dry Eye Disease (DED), or keratoconjunctivitis sicca has not been associated with Postural Orthostatic Tachycardia Syndrome (POTS) in the medical literature previously. In autonomic clinics, patients with POTS commonly endorse dry eyes and dry mouth difficulties. The association between DES, DED, and POTS has not yet been firmly established in the literature, which contributes to an underdiagnosis of this disruptive process.
Sjogren’s syndrome (SS) is well characterized across neurology and rheumatology journals to be associated with both impaired autonomic function and postural orthostasis. Also termed the sicca complex, the combination of DES and dry mouth is thought to be due to an autoimmune pathology in SS that causes dysfunction of exocrine glands. Autonomic symptoms are common and contribute to the disease burden of primary Sjogren’s disease.1 Dysautonomia and peripheral neuropathies are classically associated with Sjogren’s disease and there have been well-characterized clinical cases describing orthostatic hypotension in patients with Sjogren’s disease.
In a 2008 NEJM clinical practice guideline regarding neurogenic orthostatic hypotension, Sjogren’s syndrome and idiopathic immune-mediated autonomic neuropathies are listed as commonly associated with this disease.2 Neurological changes in primary SS are diverse in presentation and localization. A 2012 review paper by Tobon et al in Autoimmune Disorders catalogs central and peripheral neuropathies found to be manifestations of primary Sjogren’s disease and implicates vasculitis, antineuronal antibodies, and lymphocytic infiltration of spinal ganglion as possible pathogenic mechanisms.3
Historically, the first cases of patients with both sicca complex and dysautonomia were presented as letters to the editor of various journals. In 1999 a letter first reported recurrent syncope in a 37-year-old woman with SS and severe orthostatic hypotension that responded to IV Immunoglobulin (IVIG) therapy.4 A 2006 letter describes a 28-year-old woman with lupus and SS presenting with worsening postural hypotension and pandysautonomia.5 Both cases mentioned that no orthostatic tachycardia was observed. These cases posited that autonomic neuropathies arise in the setting of an autoimmune flare. Since these cases were published, the co-conditional prevalence between peripheral neuropathy and primary Sjogrens has been quoted to be as high as 20%.3,6
Despite an established association between the sicca complex and orthostatic hypotension (OH), no prior works report an association between sicca complex and POTS. This may be a matter of selection bias. Sjogren’s disease and OH share greater overlap in age demographic compared to Sjogren’s disease and POTS. The median age of onset for Sjogrens is 52 years, and OH is more likely to affect patients of advanced age. POTS, however, typically presents in women between the ages 14 and 45 years of age.7
We propose that the dry eye complaints of patients with POTS are not independent from their neurologic condition. DES may be the result of an immune-mediated or inflammatory damage related to the neuropathy causing dysautonomia and POTS, interrupting exocrine gland function, and causing a high incidence of sicca complex in this population. We hypothesize that there is a clinically significant incidence of dry eye symptoms in these patients.
Patients and Methods
This is a retrospective review of patient data collected from autonomic clinic visits between December 2019 and March 2020. During the typical autonomic visit, patients with POTS were asked to fill out a symptom survey. Patients that endorsed any dry eye symptoms were also assessed for clinically dry eyes in the physical exam portion of their visit. Figure 1 illustrates the symptom survey provided to patients during their clinical visit.
 |
Figure 1 Survey questions answered by patients in POTS clinic. |
Patients that presented to our neurology group autonomic clinic for a new assessment and work-up for postural tachycardia syndrome or for follow-up for previously diagnosed POTS had their data reviewed. Patients were diagnosed with POTS and eligible for recruitment to the study group if they either had confirmed orthostatic tachycardia with Tilt Table testing or a measured heart rate that increased greater than 30 beats per minute during postural testing in the clinic.
None of the patients presenting for POTS work-up or follow-up had been previously diagnosed with DES, sicca complex, Primary or Secondary Sjogren’s Disease. While no age, sex, or significant medical history excluded patients from enrollment, all subjects included in retrospective analysis were over 18 years of age, and had no history of cerebrovascular events, implanted nerve stimulators, pacemakers, or cardiothoracic surgeries.
Eligible patients were asked to fill a voluntary symptom survey consisting of 8 questions screening for sicca complex. Four questions correlate to each of the two symptom domains of Sjogren’s syndrome (SS). The questions were adopted from the ocular and oral symptom domains presented as classification criteria for secondary SS.8 The survey then adds additional questions screening patients for known rheumatic and common autoimmune diseases that are heavily associated with secondary SS. Finally, if patients endorsed a history of Connective Tissue Disease they are asked to specify whether they had been diagnosed with Mixed Connective Tissue Disease or Ehlers-Danlos Syndrome. This is documented as patients with joint hypermobility syndrome have been noted in prior studies to have ocular abnormalities including xerophthalmia.9
Medications Associated with DES
DES can be the adverse effect of many commonplace prescription medications in any clinical setting. This study proposes that the frequency distribution of DES symptoms endorsed among the POTS patient population is independent of the medications taken that are known to cause eye dryness and DES is a result of POTS pathology. In order to address the impact of medications on patients with POTS, a Chi-squared test for independence was performed. Every patient that filled out the symptom survey had an outpatient medication list that was reviewed. We defined a medication group as patients who, since their last clinic visit, have been managed in the outpatient setting with at least one medication that falls into the following groups: beta-2 agonists, loop diuretics, anticholinergics, or H1 receptor antagonists. Many other medications have pharmacologic monographs listing dry eye or mouth symptoms as possible adverse effects.10 This list includes beta blockers, hypnotics, neuroleptics, retinoids, and retroviral therapy. However, this study simplifies its categories by only taking into account the aforementioned known physiologic mechanisms for DES.
Furthermore, patients with POTS are commonly prescribed pyridostigmine for autonomic symptom management. This study took particular consideration towards this known anticholinesterase, which should counteract eye dryness. Patients enrolled in this study were also sorted into pyridostigmine and non-pyridostigmine groups. Pyridostigmine groups are not mutually exclusive categories from dry eye inducing medication groups. As such, pyridostigmine and DES Medication categories are used in separate Chi squared tests because patients would otherwise be organized into more than 2 variables and the study groups would not be independent.
With a confidence P-value of 0.05, we crafted two null hypotheses. Firstly, the prevalence of patients presenting to our POTS clinic with DES is independent of the medications they take that are labeled and known to cause dry eye symptoms. Secondly, the likelihood of patients presenting to our POTS clinic with DES is independent of whether they are on pyridostigmine, a medication known to increase lacrimation and prevent dry eyes.
Dry Eye Testing
If a patient endorsed dry eye symptoms in our screening survey, the physical exam portion of their visit included a Schirmer’s test.11,12 Fifteen millimeter test strips were placed in both eyes without anesthesia and left in place until either the entire test strip was wet or 5 minutes had elapsed. No patients tested with Schirmer’s strips used or were prescribed any lubricants or artificial tears nor were any used during their clinic visit. Based on the wetting of test strips for each eye, patients were stratified to the severity of ocular dryness.
While there is no true consensus to the cutoff of Schirmer score for dry eye diagnosis, this study adopted a cutoff value of <10mm/5 min as clinically dry, and used <5mm/5 min as moderate dryness.13,14 For further stratification, <1mm/5 min was selected as the cutoff for severe eye dryness as this was the smallest measurement in the clinic. The cutoff for abnormally dry eyes was less than or equal to 10 mm in 5 minutes.
Each eye was documented separately to identify potential ocular asymmetry in DES symptoms. Patients demonstrating keratoconjunctivitis sicca during their clinic visit were referred to Ophthalmology for additional dry eye work-up and management.
Results
A total of 23 patients participated in the symptom survey, and demographic information is presented in Table 1. Twenty-two of twenty-three patients were female sex and our sample had an age distribution with a mean of 34.9 years and a standard deviation of 14.0. Epidemiological studies report female to male ratios of POTS to 4–5:1 and a ten year retrospective study from Mayo clinic registered 152 patients with POTS of with 86.8% were female sex with an age distribution of 30.2 years and a standard deviation of 10.3.15
 |
Table 1 Demographic Data of the Survey |
Table 2 presents data compiled from dry eye and dry mouth symptom surveys. A majority of patients participating in survey collection endorsed dry eye (65.2%), dry mouth (73.9%), and sicca complex (52.2%). The age distribution of patient’s endorsing symptoms is presented in the table as well to address concerns that advanced age would be a confounding factor given the increased incidence of keratoconjunctivitis or keratostomia with age.
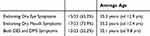 |
Table 2 Sicca Complex Data |
Among patients with POTS retrospectively enrolled in this study, eight patients had tear production quantified with Schirmer’s test strips and this is outlined in Table 3. Seven of eight patients had at least one eye with a tear strip wetting less than 10 mm/5 min. Among patients with dry eyes, 87.5% had at least one clinically measured dry eye. Eighty-one percent of eyes tested showed decreased tear production with strip wetting less than 10 mm/5 min (13/16).
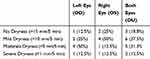 |
Table 3 Schirmer’s Tear Tests for N= 8 (10 Offered, 1 Declined, 1 Did Not Tolerate) |
Table 4 shows a two Pearson’s chi-squared test for independence between dry eye medications and DES in patients with POTS resulted X2 (1, N = 23) = 0.0137, p = 0.906855. Table 5 shows a test between pyridostigmine use and DES in patients with POTS resulted X2 (1, N = 23) = 1.7044, p = 0.191719. For P<0.05, the endorsed DES in patients with POTS is not confidently dependent on medications known to cause or present dry eyes.
 |
Table 4 Medications and Dry Eye Symptoms in the POTS Clinic |
 |
Table 5 Pyridostigmine and Dry Eye Symptoms in the POTS Clinic |
With regards to joint hypermobility disorders, 8 of the 23 surveyed patients endorsed a diagnosis of EDS either with genetic or pathologic verification. One of twenty-three had ongoing work-up for connective tissue disease, and one of the eight patients with EDS and POTS had a history of childhood arthritis. Four of eight (50%) EDS+POTS patients endorsed dry eye symptoms and only 1 patient with POTS and EDS had been tested for tear production. This patient had clinically dry eyes.
Discussion
The majority of patients presenting to the neurology clinic for POTS evaluation endorse dry eyes or dry mouth. This study’s survey results indicate that patients with POTS are likely to present with dry eye symptoms. Additionally, patients with POTS are likely to endorse dry mouth symptoms.
Dry eyes are an incredibly common complaint in the clinical setting. While common medications cause DES complaints in any setting, this study demonstrates that for numerous POTS patients these endorsed symptoms are backed by clinical evidence of significantly dry eyes. Our small sample of the POTS patient population demonstrates evidence of moderate to severe dry eyes with decreased tear production. There is some variability in using Schirmer test strips as there are differing cut offs among clinicians for determining clinically dry eyes.
The investigation into how POTS patient’s medications could impact the severity of eye complaints was telling. Commonly prescribed medications such as albuterol inhalers, furosemide diuretics, and antihistamine allergy medications are not associated with the DES that we see in POTS patients. Additionally, 87% of the patient group had measurable dryness on the Schirmer's test, which is a marked difference when compared to the general population, where the prevalence of DES has been quoted at 7% in women and 4% of men over the age of 50.16
A patient presenting to their POTS follow-up appointment endorsing dry eye symptoms offers a wide differential diagnosis. For patients of advanced age, the most common cause of dry eye syndrome (DES) excluding acute viral infection and idiopathic dry eyes is age-related glandular fibrosis. Contact lens use, prolonged screen use, allergic conjunctivitis are also on the differential. Uncontrolled diabetes, chronic alcoholism can cause both dry eyes and mouth related to the sicca complex.
With regards to age, our patient population is relatively young. The POTS dysautonomia patient population is younger by age distribution when compared to patients with orthostatic hypotension. While there is an element of age-related glandular fibrosis in older patients, this should not apply to our younger patients unless there was some suspected direct ocular pathology with POTS.
Medications including antidepressants and antihistamines can also cause dry eyes as an adverse effect. Patients concurrently suffering from chronic pain, neuropathic pain, fibromyalgia or small fiber neuropathy may be also taking tricyclic antidepressants and they are intentionally not excluded from this study. Dry mouth can arise or be exacerbated by alpha-1-agonists such as midodrine. In addition, antidepressants and neuroleptics such as quetiapine can cause both dry eyes and mouth. On the other hand, patients with POTS are commonly managed on pyridostigmine which is known to increase lacrimation. As demonstrated, the variety of medications used to treat dysautonomia can cause either facet of the sicca complex. To directly address this factor, our study presents a large P-value in independent Chi-squared tests which accept the null hypothesis. The frequency distribution of DES in patients with POTS in our sample is likely not related to the presence of anticholinergics and antihistamines. One clear criticism of our study is the sample size. Although this is a small sample, as per Table 1 the patients in this study are representative of the generally young and female POTS patient population. This population has a lower incidence of alcohol abuse and diabetes.
Primary SS has a high prevalence rate among the general population presenting with dry eyes, up to 10%. In populations with known autoimmune diseases the rate of primary SS is even higher.8 Up to 75% of patients with Sjogren’s disease have seropositivity in SS-A or SS-B, regardless of ANA and RF titers. As an aside, high serum ANA titers prevail in women between ages 20 to 50 which coincides with the epidemiology of POTS.17
The interconnection of joint hypermobility, autonomic dysfunction, and exocrine gland dysfunction is unexplored. POTS patients suffer from autonomic dysfunction affecting multiple organs.18,19 While none of our POTS subjects had a serologic diagnosis of Sjogren’s syndrome, many had been diagnosed with Ehlers-Danlos Syndrome (EDS). EDS has been associated with POTS, and prior studies on EDS have documented ocular manifestations of the disease, including dry eye syndrome.20 While the survey data demonstrates that patients with EDS and POTS can also endorse dry eyes, there is not enough power in our survey data to make any cautious interpretation of the relationship between the EDS, POTS, and DES.
Ultimately, POTS is an autonomic disorder with a heavy disease burden. Dry eye and dry mouth are additional manifestations of autonomic dysfunction and should be evaluated in POTS patients. If there is high pretest clinical suspicion of significant exocrine gland dysfunction patients should be referred for to ophthalmology for further dry eye work-up. There is a higher incidence of sicca complex in patients with POTS dysautonomia compared to the general public.
Conclusion
This project introduced quantitative dry eye testing to the neurology clinic and we demonstrate that Schirmer’s tests are feasible to incorporate into dysautonomia practice. Patients endorsing dry eye symptoms have been referred to outpatient Ophthalmology where we defer to their expertise regarding tear break up times, ocular surface staining, and osmolarity testing. The efficacy of dry eye medications and management in the POTS and dysautonomia patient population is currently unexplored and would benefit from additional research. Thus, this study opens a wide range of opportunities for interdisciplinary research into POTS and dysautonomia.
Dry mouth and exocrine gland dysfunction in the POTS clinic is another frontier for autonomic research. Dry mouth symptoms can be explored objectively in patients in the POTS clinic with further testing. Non-invasive options for future investigation include salivary gland scintigraphy, whole sialometry, and salivary gland ultrasound.
Finally, patients surveyed in our study were also asked to endorse whether they had been identified as having any genetic variant. Some of our patients had geneticist testing for Ehlers-Danlos Syndrome as there is significant clinical overlap between patients with hypermobility disorders and POTS. An additional direction for further investigation would be to see if patients with the subset of hypermobility disorders experienced a greater association with exocrine gland dysfunction compared to other patients with POTS.
Ethics Statement and Patient Consent
This retrospective study was completed with approval from the Institutional Review Board at St. Elizabeth’s Medical Center. This publication did not involve any sponsors or sources of funding for financial support. This study was completed with every effort made to adhere to the ethical principles presented in the WMA Declaration of Helsinki. The requirement for patient consent regarding the acquisition of medical records was waived by the IRB at St. Elizabeth’s Medical Center as this study was a retrospective analysis of anonymized data. Patient date of birth is initially obtained to determine the age of patients for the database and then removed thereafter. This is the only identifier used in data collection and it is removed immediately after logging other variables into the database. Otherwise no Personal Health Information was collected to be stored long term.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Newton JL, Frith J, Powell D, et al. Autonomic symptoms are common and are associated with overall symptom burden and disease activity in primary Sjogren’s syndrome. Ann Rheum Dis. 2012;71(12):1973–1979. doi:10.1136/annrheumdis-2011-201009
2. Freeman R. Clinical practice neurogenic orthostatic hypotension. N Engl J Med. 2008;358(6):615–624. doi:10.1056/NEJMcp074189
3. Tobón GJ, Pers JO, Devauchelle-Pensec V, Youinou P. Neurological disorders in primary sjögren’s syndrome. Autoimmune Dis. 2012;2012:645967.
4. Dupond JL, Gil H, de Wazieres B. Five-year efficacy of intravenous gammaglobulin to treat dysautonomia in Sjögren’s syndrome. Am J Med. 1999;106(1):125.
5. Law WG, Thong BY, Umapathi T, Chng HH. Acute pan-dysautonomia: a rare initial presentation of lupus with Sjogren’s syndrome. Lupus. 2006;15(12):899–900. doi:10.1177/0961203306070984
6. Barendregt PJ, van den Bent MJ, van Raaij-van den Aarssen VJ, et al. Involvement of the peripheral nervous system in primary Sjögren’s syndrome. Ann Rheum Dis. 2001;60(9):876–881.
7. Patel R, Shahane A. The epidemiology of Sjögren’s syndrome. Clin Epidemiol. 2014;6:247–255.
8. Sebastian A, Szachowicz A, Wiland P. Classification criteria for secondary Sjögren’s syndrome. Current state of knowledge. Reumatologia. 2019;57(5):277–280. doi:10.5114/reum.2019.89520
9. Gharbiya M, Moramarco A, Castori M, et al. Ocular features in joint hypermobility syndrome/ehlers-danlos syndrome hypermobility type: a clinical and in vivo confocal microscopy study. Am J Ophthalmol. 2012;154(3):593–600.e1. doi:10.1016/j.ajo.2012.03.023
10. Scully C. Drug effects on salivary glands: dry mouth. Oral Dis. 2003;9(4):165–176. doi:10.1034/j.1601-0825.2003.03967.x
11. Stevens S. Schirmer’s test. Community Eye Health. 2011;24(76):45.
12. Akpek EK, Amescua G, Farid M, et al. Dry eye syndrome preferred practice pattern®. Ophthalmology. 2019;126(1):P286–P334. doi:10.1016/j.ophtha.2018.10.023
13. Messmer EM. The pathophysiology, diagnosis, and treatment of dry eye disease. Dtsch Arztebl Int. 2015;112(5):71–81.
14. Senchyna M, Wax MB. Quantitative assessment of tear production: A review of methods and utility in dry eye drug discovery. J Ocul Biol Dis Infor. 2008;1(1):1–6. doi:10.1007/s12177-008-9006-2
15. Thieben MJ, Sandroni P, Sletten DM, et al. Postural orthostatic tachycardia syndrome: the Mayo clinic experience. Mayo Clin Proc. 2007;82(3):308–313. doi:10.1016/S0025-6196(11)61027-6
16. Gayton JL. Etiology, prevalence, and treatment of dry eye disease. Clin Ophthalmol. 2009;3:405–412. doi:10.2147/OPTH.S5555
17. Fritzler MJ, Pauls JD, Kinsella TD, Bowen TJ. Antinuclear, anticytoplasmic, and anti-Sjogren’s syndrome antigen A (SS-A/Ro) antibodies in female blood donors. Clin Immunol Immunopathol. 1985;36(1):120–128. doi:10.1016/0090-1229(85)90045-5
18. Wallman D, Weinberg J, Hohler AD. Ehlers-danlos syndrome and postural tachycardia syndrome: a relationship study. J Neurol Sci. 2014;340(1–2):99–102. doi:10.1016/j.jns.2014.03.002
19. Deb A, Morgenshtern K, Culbertson CJ, Wang LB, Hohler AD. A survey-based analysis of symptoms in patients with postural orthostatic tachycardia syndrome. Proc. 2015;28(2):157–159. doi:10.1080/08998280.2015.11929217
20. Perez-Roustit S, Nguyen DT, Xerri O, et al. [Ocular manifestations in Ehlers-Danlos syndromes: clinical study of 21 patients]. J Fr Ophtalmol. 2019;42(7):722–729. doi:10.1016/j.jfo.2019.01.005.French.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
