Back to Journals » Patient Preference and Adherence » Volume 11
Drug utilization and therapy provision patterns by prescriber types among patients with systemic lupus erythematosus in Korea
Authors Shin S
Received 12 July 2017
Accepted for publication 23 September 2017
Published 17 October 2017 Volume 2017:11 Pages 1779—1787
DOI https://doi.org/10.2147/PPA.S146119
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Sooyoung Shin
College of Pharmacy and Research Institute of Pharmaceutical Science and Technology (RIPST), Ajou University, Yeongtong-gu, Suwon, Republic of Korea
Background: Systemic lupus erythematosus (SLE) poses a growing challenge for healthcare systems, affecting an increasing number of people in Korea. This study aimed to investigate the prescribing patterns of SLE therapies and to compare common drug regimens prescribed by provider types.
Methods: Sampled national health insurance claims data in 2015 were used to select eligible SLE patients. Frequency analyses were carried out regarding patient characteristics related to relevant SLE prescriptions. Patient-days were calculated per substance and per drug class and then categorized by provider types. Differences in drug utilization trends among the main types of providers were examined with the chi-square test.
Results: A total of 2,074 patients with SLE were selected for study inclusion. Systemic corticosteroid therapy was provided for up to 67.9% of patients, frequently in conjunction with other SLE therapies. About 33.2% and 18.7% of steroid users were treated for more than 150 days and 300 days during the study period, respectively. The provider group that most frequently prescribed systemic corticosteroids was dermatologists. Hydroxychloroquine, an antimalarial considered pivotal to SLE management, was prescribed for only 32.4% of patients, predominantly by rheumatologists. Antimalarial therapy was associated with the longest therapy duration (257.7±120.1 days), followed by immunosuppressant therapy (187.0±153.0 days). Prescription rates of antimalarials and immunosuppressants were substantially lower in primary care doctor group and particularly in dermatologist group, compared to rheumatologist group (P-value associated with prescription patterns by provider types was <0.001 for both drug classes).
Conclusion: The drug utilization patterns among the main provider groups commonly providing care for SLE patients differed significantly depending on their practice areas. The prescription rates of corticosteroids were disproportionately higher among dermatologists. Rheumatologists appeared more cognizant of the importance of providing antimalarial therapy for SLE patients compared to other types of providers.
Keywords: systemic lupus erythematosus, drug utilization, antimalarials, corticosteroids
Introduction
Systemic lupus erythematosus (SLE) is a multisystem autoimmune disorder with chronic inflammation in diverse organs, which is speculated to be linked to overproduced autoantibodies attacking the body’s own organs and tissues.1 SLE is generally regarded as a rare, incurable, and possibly underdiagnosed disease.2,3 Similar to other autoimmune diseases, it develops more frequently in women than in men, particularly during their reproductive years.3 With recent upward trends in prevalence and incidence of SLE in Korea,4 concerns have been raised that the disease is placing an increasing burden on healthcare systems and that its negative effects on birth rates and productivity in society are projected to be a growing problem.5,6
SLE patients typically present with a varying degree of abnormalities of constitutional, musculoskeletal, cutaneous, renal, and/or hematologic features due to systemic inflammatory response associated with dysfunctional immunity.7 The disease can be life-threatening for some patients, especially those who experience recurrent exacerbations with complications related to neurological, renal, and/or cardiopulmonary systems.8 Given its nonspecific clinical presentations that mimic other disease states and the absence of confirmatory laboratory test for diagnosis along with disparities in validation methods,9,10 SLE can be a challenging disease to diagnose. As a result, delays in diagnosis or misdiagnosis can occur. A previous study reported on a low agreement between rheumatologists and primary care doctors for the diagnosis of rheumatic disorders, and 41% of primary care diagnoses were revised subsequently by rheumatologists following patient referral.11
With no definitive cure established thus far, the current standard of care for SLE centers on symptoms control with a goal of attaining remission at times of exacerbations and consolidating remission while preventing recurrent flares.12,13 Therapeutic modalities are primarily composed of four drug classes: nonsteroidal anti-inflammatory drugs (NSAIDs), antimalarials, corticosteroids, and immunosuppressants. As with other chronic autoimmune diseases, most lupus patients are treated life long and hence often faced with high medical expenses for disease management.5,6 They are also at substantially higher risk of mortality compared to the healthy population,14 and susceptible to a wide range of complications attributable to the systemic progression of the disease as well as adverse effects from chronic exposure to lupus treatments.15
Epidemiologic findings on medication utilization for the treatment of SLE in Korea has not been reported. The objectives of the present study were to analyze the prescribing patterns of SLE therapies and to evaluate the differences of pharmacologic regimens provided by prescribers depending on their practice areas by analyzing sampled claims data of Korean National Health Insurance (NHI).
Methods
Study population
Patient data were collected from the Korean Health Insurance Review & Assessment Service-National Patients Sample-2015 (HIRA-NPS-2015-0068), which contains three percent of the Korean population data with ensured national representativeness. The patient samples were extracted based on a stratified randomized sampling method. Under the NHI program, most of the Korean population of about 50 million are provided with universal coverage for medical services on the fee-for-services basis, where providers are paid a fixed amount per each service rendered.16 Korean patients typically have a universal co-payment rate of 30% for outpatient medicine including pharmaceutical expenditure. The HIRA database holds administrative claims data related to healthcare services provided for the entire national beneficiaries: patient demographics, procedures, diagnoses (the International Classification of Disease, 10th Revision [ICD-10]), and all medical utilization including prescriptions. Patients with SLE were identified if they had received a diagnosis of SLE (ICD-10 code M32.x) at least once and prescribed SLE therapy belonging to the following drug classes: NSAIDs, antimalarials, corticosteroids, and immunosuppressants. The protocol of this study was approved by the Institutional Review Board of Ajou University (201702-HB-EX-001). Informed consent from study subjects was waived by the Institutional Review Board because this was a retrospective study of anonymized patient data. Further ethics approval was not required for the present study, as the HIRA authorized the researcher to analyze de-identified patient health data for research purposes.
Study medications and variables
A total of 72 drug codes on the national formulary were used to capture the relevant patient data for the study analysis, including individual agents belonging to the aforementioned drug classes. All eligible prescriptions were extracted using prescription drug data. Only systemic treatment was selected for study inclusion: NSAIDs and antimalarials included for the analysis were all orally administered; corticosteroids and immunosuppressants were either orally or intravenously administered. Medication utilization patterns were tracked and analyzed by drug classes as well as by individual active ingredients. If a medication is prescribed within 7 days following the last dose, the use was considered as continued therapy. Any NSAIDs with a duration of less than 7 days were considered temporary therapy and excluded from the analysis. Concomitant use of multiple SLE therapies was defined as more than one agent belonging to different drug classes being prescribed to a single patient with the overlapping duration of treatment for at least 30 days. Switching patterns between pharmacologic substances within the same drug class were also investigated. A switch from one drug to a different drug was identified through screening those agents prescribed within 30 days prior to or following the discontinuation of the previous medication. Additionally, discontinuation patterns of SLE therapies were also analyzed. If no more prescriptions were issued within 60 days post the last dose, the therapy was considered discontinued. For the assessment of maintenance doses of corticosteroids, only those regimens with therapy duration of 30 days and more were included, and the total daily dose in mg was calculated by each steroid substance. Major types of providers commonly providing care for SLE patients were also identified by comparing provider types with different specialty backgrounds on the basis of the total volume of patient-days, and their prescribing patterns were assessed to investigate any differences in the provision of pharmacologic treatment depending on their practice areas. Patient demographic data were collected and assessed, including age, sex, practice areas, insurance type, level of institution, region of institution, and clinical manifestations of SLE (including oral ulcer, arthritis, nephritis, seizure, and psychosis).
Statistical analysis
Frequency analyses were performed to interpret the full scale of drug therapies provided for SLE patients by the type of insurance and healthcare institution, SLE manifestations, and other parameters for healthcare utilization. Patient-days were calculated by multiplying the number of patients by the number of prescribed days for each therapy, and expressed by drug class and by individual active ingredient. Pearson chi-square test was conducted to examine the differences in prescription patterns associated with the four classes of SLE therapy according to the practice areas of the common provider groups. All statistical tests were two-sided and the P-value below 0.05 was considered statistically significant. All statistical analyses were completed with SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Characteristics of study patients
In 2015, of the total number of Korean people registered in the HIRA database (50,490,157), the number of patients initially extracted for the patient sample was 1,454,249 (male 48.7%). Of those, patients with a history of SLE who received at least one lupus therapy were selected, and a total of 2,074 patients were eligible for study entry. Patient characteristics are summarized in Table 1. Female subjects outnumbered males by approximately threefold (74.6% versus 25.4%). The number of SLE patients increased substantially with age, regardless of sex, with the age group of 41–60 years showing the highest rates, but the percentage steeply decreased thereafter in both sexes. The visit episodes were predominantly covered by national health insurance (1,959 patients; 94.5%). With regard to the level of institution, the most common health facility where SLE patient care was provided was office-based physician practice (1,268 patients; 61.1%), followed by general hospitals (340 patients; 16.4%). Geographically, more patients appeared to reside in metropolitan areas near Seoul, the capital city, and Gyeonggi province (1,097 patients; 52.9%) than in rural areas. The common clinical presentations of SLE were arthritis (1,348 patients; 65.0%), followed by renal disorders (472 patients; 22.8%).
  | Table 1 Demographic features of patients with SLE |
Drug utilization patterns in SLE patients
Of the 2,074 patients, the number of patients who received NSAIDs, antimalarials, corticosteroids, and immunosuppressants were 1,751 (84.4%), 672 (32.4%), 1,408 (67.9%), and 309 (14.9%), respectively. The number of patients who had switched agents within the same drug class was as follows: 1,287 (62.1%) for NSAIDs, none for antimalarials (a single agent of hydroxychloroquine available in Korea), 518 (25.0%) for corticosteroids, and 49 (2.4%) for immunosuppressive agents (Table 2). With regard to therapy discontinuation patterns, NSAIDs had been stopped in 878 patients (42.3%), antimalarials in 120 (5.8%), corticosteroids in 648 (31.2%), and immunosuppressants in 68 (3.3%).
  | Table 2 Patterns of drug use in patients with SLE |
The most preferred class of medications prescribed as monotherapy among SLE patients was antimalarials (254 patients; 12.2%), followed by NSAIDs (217 patients; 10.5%). For dual combination therapy, an antimalarial combined with corticosteroid therapy was most common (275 patients; 13.3%), followed by NSAID plus antimalarial therapy (68 patients; 3.3%). For triple therapy, an antimalarial in combination with corticosteroid plus immunosuppressant therapy was most frequently used (92 patients; 4.4%). Only 13 patients (0.6%) received all four classes of medications concurrently.
The mean treatment duration in days was longest with antimalarial therapy (257.7±120.1), followed by immunosuppressant therapy (187.0±153.0), and lowest with NSAID therapy (53.8±88.1) (Figure 1). The percentage of patients who continued each therapy for over 150 days during the study period was up to 78.1% with antimalarials, 51.8% with immunosuppressants, 33.2% with corticosteroids, and 10.5% with NSAIDs. Of those patients, up to 47.0% of patients continued antimalarial therapy for more than 300 days, 32.0% for immunosuppressive therapy, 18.7% for corticosteroid therapy, and 4.2% for NSAID therapy.
When presented in order of prescription volume by drug classes regardless of prescriber types, loxoprofen, dexibuprofen, talniflumate, and diclofenac were the top four most frequently prescribed agents for NSAIDs; prednisolone, methylprednisolone, triamcinolone, and deflazacort for corticosteroids; methotrexate, mycophenolate, azathioprine, and leflunomide for immunosuppressants. Prednisolone showed the highest prescription rates (37.8%), which was also the most frequently switched-to agent (27.1%–46.7%) following discontinuation of other corticosteroids. Switching patterns within immunosuppressants revealed that methotrexate was associated with the highest prescription rates (32.9%) and also the most preferred agent to switch to (21.4%–27.1%) following discontinuation of other immunosuppressants.
The assessment findings for the maintenance dose of corticosteroids with therapy duration of at least 30 days are visually depicted in Figure 2. The mean maintenance dose of most orally administered steroids appeared to fall within the normal maintenance dose limits for anti-inflammatory or immunosuppressive effects. The largest proportion of patients (64.8%) received prednisolone and its maintenance dose showed the widest variation among steroids, ranging from 1.25 to 90 mg/day with the mean maintenance dose of 7.2±6.8 mg/day; 25% of patients received less than 5 mg/day, 50% of patients between 5 and 7.5 mg/day, and the remaining 25% of patients over 7.5 mg/day.
  | Figure 2 Maintenance dose of orally administered corticosteroids with therapy duration of at least 30 days. |
Prescription patterns based on provider types
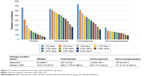
The prescription patterns for SLE patients depending on provider types were analyzed and presented per 1,000 patient-days and per patient-days in Figure 3 and Table 3, respectively. By reviewing the volume of patient-days and the relevance of both inpatient and outpatient visit episodes for SLE, the practice areas of those providers commonly treating SLE patients were identified as rheumatology, primary care, and dermatology. Overall, prescribing patterns of the four classes of SLE therapies were statistically significantly different among providers depending on their specialty backgrounds (P-value was <0.001 for all drug classes). For rheumatologists, antimalarials and corticosteroids were the most frequently prescribed drug classes, listed in order of the volume of patient-days (134,607 and 106,957, respectively). NSAIDs were most frequently prescribed by primary care doctors, followed by corticosteroids (38,322 and 28,827 in patient-days, respectively). Notably, corticosteroids were the most commonly prescribed therapy by dermatologists, followed by antimalarials (5,614 and 1,305 in patient-days, respectively).
  | Figure 3 Prescription patterns depending on provider types. |
Discussion
Overall, NSAIDs were the most commonly prescribed SLE therapy and corticosteroids were the next most frequently used therapeutic choice, based on patient volume (84.4% versus 67.9%, respectively). NSAIDs are commonly prescribed as first-line therapy for the symptomatic relief of SLE with musculoskeletal complaints, arthritis, and fever.17 Patients treated with NSAIDs were associated with the highest rate of substance switching as well as with the highest rate of therapy discontinuation (62.1% and 42.3%, respectively). This suggests as-needed-based medication utilization for symptom management and potentially adverse reactions or lack of efficacy with preceding therapy. Antimalarials were the most preferred class of agents used as monotherapy (12.2%), followed by NSAIDs (10.5%). By contrast, immunosuppressants were more commonly used in conjunction with corticosteroids and/or antimalarials. Only a limited number of patients received triple or quadruple combination therapy for SLE; of those the triple-combination regimen based on antimalarial, corticosteroid, plus immunosuppressant therapy showed the highest use rate (4.4%).
SLE can manifest in many different ways, and pharmacologic regimens for SLE treatment need to be personalized according to disease manifestations in individual patients.18,19 Patients with mild disease generally require NSAIDs and antimalarials with or without low-dose corticosteroids, whereas severe cases with major organ involvement are often treated with high-dose corticosteroids and/or immunosuppressive agents.17 Although NSAIDs are typically considered first-line therapy, their therapeutic effects are often not sufficient in SLE patients. Hence, as the findings in the present study suggest, corticosteroids are commonly prescribed as an add-on to the existing regimen and occasionally long-term despite potential adverse effects with prolonged systemic exposure to steroid therapy. For those with serious, life-threatening SLE-related problems or acute flares, especially with kidney damage, high-dose corticosteroids are generally used as the mainstay of treatment to induce a rapid remission.20 In this study, it appeared that up to 67.9% of patients received at least one dose of corticosteroids. Of those, about 33.2% and 18.7% were prescribed corticosteroid doses as maintenance therapy for more than 150 days and 300 days during the study period, respectively.
Although many lupus patients receive combination therapy, desired clinical outcomes have been most frequently reported with the use of antimalarial therapy.21–23 Hydroxychloroquine is known to be effective for SLE-related arthritis and rash control, but shows a low efficacy in preventing severe SLE presentations.24,25 More importantly, it has been associated with survival benefits in lupus patients, and confers an additional protective effect against damage accrued long-term with a good tolerance and a benign safety profile other than rare ocular toxicity.26–29 Hence, current expert opinion is that most SLE patients should be treated with hydroxychloroquine alone or concomitantly with other drugs appropriate for clinical presentations of the disease.30,31 In this study, antimalarial therapy was associated with the longest mean treatment duration (257.7±120.1 days). Additionally, greater percentage of patients who received at least one dose of antimalarials continued the treatment over 150 days and 300 days (78.1% and 47.0%, respectively) compared to those treated with other drug class treatments. However, of note was that only 32.4% of the study patients received antimalarial therapy during the study period as opposed to consensus expert recommendations concerning its universal use for most SLE patients regardless of disease severity.
A range of immunosuppressive drugs are usually considered for severe lupus with organ involvement, including lupus nephritis and neuropsychiatric lupus or for steroid-sparing purposes in SLE.32 In this study, methotrexate, mycophenolate, azathioprine, and leflunomide were the top four agents that showed the highest prescription frequencies. With the arrival of newer immunosuppressive agents, the use of cyclophosphamide, a traditional chemotherapy drug that has long been employed for the treatment of lupus, has been decreased substantially. Several severe adverse effects including malignancy, infection, infertility, and hemorrhagic cystitis are associated with cyclophosphamide.20 Hence, other immunosuppressants are more preferably prescribed for sustained remission, such as azathioprine and mycophenolate mofetil, due to their less toxic safety profile.33,34
Although pharmaceutical regimens based on NSAIDs, antimalarials, corticosteroids, and immunosuppressants have long been considered standard therapy for SLE, only four drugs have obtained an approval from the US Food and Drug Administration to be used to treat SLE thus far: aspirin, prednisone, hydroxychloroquine, and belimumab, a new addition to therapeutic options for SLE in over 50 years. Belimumab is also the first targeted monoclonal antibody-based immunotherapy that induces therapeutic effects by inhibiting autoantibody activation.35,36 The provision of drug regimens other than the above four agents is regarded as off-label use, implying those therapies have not actually been approved for use in SLE patients for treatment purposes. In addition, there are uncertainties surrounding the optimal duration and doses of off-label prescriptions for induction as well as for maintenance therapy for SLE management. Belimumab has been approved for treating SLE in Korea in 2013. However, despite expanded health insurance coverage of copayment for rare diseases including SLE,4 the NHI is still not providing coverage for belimumab. Improving access to such novel therapeutic option may have the potential to positively affect clinical outcomes and prognosis of patients with SLE.
With regard to the types of providers, SLE patients were predominantly treated and followed up by rheumatologists, primary care doctors, and dermatologists, listed in order of the total patient-days combined for all prescribed SLE therapies. Drug utilization patterns observed among prescribers were substantially distinct depending on their specialty backgrounds. Rheumatologists most frequently prescribed antimalarials, which was consistent with expert opinions that most patients with SLE should receive antimalarial therapy regardless of disease activity. By contrast, primary care doctors and dermatologists most frequently prescribed NSAIDs and corticosteroids, respectively. Interestingly, the prescription rates of immunosuppressants were disproportionately lower in primary care doctor group than in rheumatologist group. Of note was the prescribing pattern of dermatologists. They prescribed corticosteroids at disproportionally higher rates compared to other types of providers. These findings suggest that those patients not seen by rheumatologists are less likely to receive the antimalarial-based regimen, which is the most important therapy in long-term management of SLE. A prompt referral of suspected SLE patients to rheumatologists might have a positive effect on early diagnosis and improved patient outcomes.37,38 Considering the characteristics of SLE as a complex rheumatic disease with a myriad of disease manifestations and varied progression rates, the disease is recommended to be followed by specialists, such as rheumatologists. Previous studies reported that rheumatologists more frequently ordered SLE biomarkers that are strongly related to disease severity and damage accrual than did non-rheumatologists.39,40 More importantly, rheumatologists were more likely to prescribe hydroxychloroquine than other doctors.28,29,41 These findings suggest that all providers need to raise awareness on guideline recommendations to guide lupus control and should be more cognizant of the use of hydroxychloroquine in their lupus patients regardless of disease activity level and refer patients to a specialist promptly when deemed clinically necessary.
One of the strengths of this study is the use of dataset reflecting actual prescription patterns in real-world clinical practice. In a clinical research for a rare disease, recruiting enough study participants can be a challenge. Using health insurance claims data has an advantage in such case because SLE patients can be confirmed by diagnostic codes along with other relevant patient information including prescription data. With ensured national representativeness of the data source, the findings of the present study can be considered as reflecting real-world practice and convey clinical implications. It highlights the importance for providers to consider prescribing hydroxychloroquine therapy more cognizantly in their SLE patients.
This study was subject to many limitations. First, as the dataset contains the data from one particular year, those patients with a long remission period who did not require medical attention might not have been captured as SLE patients. Also, it is not certain whether patients followed by other providers had already been evaluated by rheumatologists and standard SLE therapy recommended by guidelines had been provided previously. Second, study subjects were identified if they had received a diagnosis of SLE at least once, although diagnostic codes not recorded or recorded incorrectly by providers could have affected the number of patients included in this study. However, by excluding prescription claims associated with irrelevant practice areas and including only those claims for health care visit episodes for SLE, the risk of overestimating the number of SLE patients was minimized. Lastly, the time elapsed since the initial diagnosis could not be determined, which may have influenced drug regimens prescribed by providers. Further studies with larger samples and more clinical information need to be conducted to confirm the findings of this study.
Conclusion
Prescription patterns of the four main classes of SLE therapies differed substantially with a statistical significance among prescribers depending on their practices areas. The prescription rates of corticosteroids were disproportionately higher among dermatologists. Rheumatologists were the provider group that most frequently prescribed hydroxychloroquine, suggesting they are more cognizant of the significance of treatment recommendations regarding antimalarial therapy for SLE patients compared to other types of providers.
Acknowledgments
This study was supported by Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Science, ICT & Future Planning (No 2017R1C1B5015912). The patient data for the analysis were provided by the HIRA. The contents of this research do not represent the official views of the HIRA.
Disclosure
The author reports no conflict of interest in this work.
References
Cassano G, Roverano S, Paira S, et al. Accrual of organ damage over time in Argentine patients with systemic lupus erythematosus: a multi-centre study. Clin Rheumatol. 2007;26(12):2017–2022. | ||
Chakravarty EF, Bush TM, Manzi S, Clarke AE, Ward MM. Prevalence of adult systemic lupus erythematosus in California and Pennsylvania in 2000: estimates obtained using hospitalization data. Arthritis Rheum. 2007;56(6):2092–2094. | ||
Pons-Estel GJ, Alarcón GS, Scofield L, Reinlib L, Cooper GS. Understanding the epidemiology and progression of systemic lupus erythematosus. Semin Arthritis Rheum. 2010;39(4):257–268. | ||
Shim JS, Sung YK, Joo YB, Lee HS, Bae SC. Prevalence and incidence of systemic lupus erythematosus in South Korea. Rheumatol Int. 2014;34(7):909–917. | ||
Lau CS, Mak A. The socioeconomic burden of SLE. Nat Rev Rheumatol. 2009;5(7):400–404. | ||
Slawsky KA, Fernandes AW, Fusfeld L, Manzi S, Goss TF. A structured literature review of the direct costs of adult systemic lupus erythematosus in the US. Arthritis Care Res (Hoboken). 2011;63(9):1224–1232. | ||
Von Feldt JM. Systemic lupus erythematosus. Recognizing its various presentations. Postgrad Med. 1995;97(4):79, 83, 86 passim. | ||
Fessler BJ, Boumpas DT. Severe major organ involvement in systemic lupus erythematosus. Diagnosis and management. Rheum Dis Clin North Am. 1995;21(1):81–98. | ||
Firooz N, Albert DA, Wallace DJ, Ishimori M, Berel D, Weisman MH. High-sensitivity C-reactive protein and erythrocyte sedimentation rate in systemic lupus erythematosus. Lupus. 2011;20(6):588–597. | ||
Gaitonde S, Samols D, Kushner I. C-reactive protein and systemic lupus erythematosus. Arthritis Rheum. 2008;59(12):1814–1820. | ||
Gamez-Nava JI, Gonzalez-Lopez L, Davis P, Suarez-Almazor ME. Referral and diagnosis of common rheumatic diseases by primary care physicians. Br J Rheumatol. 1998;37(11):1215–1219. | ||
Bertsias G, Ioannidis JP, Boletis J, et al; Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics. EULAR recommendations for the management of systemic lupus erythematosus. Report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics. Ann Rheum Dis. 2008;67(2):195–205. | ||
van Vollenhoven RF, Mosca M, Bertsias G, et al. Treat-to-target in systemic lupus erythematosus: recommendations from an international task force. Ann Rheum Dis. 2014;73(6):958–967. | ||
Borchers AT, Keen CL, Shoenfeld Y, Gershwin ME. Surviving the butterfly and the wolf: mortality trends in systemic lupus erythematosus. Autoimmun Rev. 2004;3(6):423–453. | ||
Bongu A, Chang E, Ramsey-Goldman R. Can morbidity and mortality of SLE be improved? Best Pract Res Clin Rheumatol. 2002;16(2):313–332. | ||
Kim JY, Lee J, Ko YJ, et al. Multi-indication carbamazepine and the risk of severe cutaneous adverse drug reactions in Korean elderly patients: a Korean health insurance data-based study. PLoS One. 2013;8(12):e83849. | ||
Xiong W, Lahita RG. Pragmatic approaches to therapy for systemic lupus erythematosus. Nat Rev Rheumatol. 2014;10(2):97–107. | ||
Wallace DJ. Improving the prognosis of SLE without prescribing lupus drugs and the primary care paradox. Lupus. 2008;17(2):91–92. | ||
Vitali C, Bencivelli W, Isenberg DA, et al. Disease activity in systemic lupus erythematosus: report of the Consensus Study Group of the European Workshop for Rheumatology Research. II. Identification of the variables indicative of disease activity and their use in the development of an activity score. The European Consensus Study Group for Disease Activity in SLE. Clin Exp Rheumatol. 1992;10(5):541–547. | ||
Yildirim-Toruner C, Diamond B. Current and novel therapeutics in the treatment of systemic lupus erythematosus. J Allergy Clin Immunol. 2011;127(2):303–312; quiz 313–314. | ||
Akhavan PS, Su J, Lou W, Gladman DD, Urowitz MB, Fortin PR. The early protective effect of hydroxychloroquine on the risk of cumulative damage in patients with systemic lupus erythematosus. J Rheumatol. 2013;40(6):831–841. | ||
Jung H, Bobba R, Su J, et al. The protective effect of antimalarial drugs on thrombovascular events in systemic lupus erythematosus. Arthritis Rheum. 2010;62(3):863–868. | ||
Pons-Estel GJ, Alarcón GS, Gonzalez LA, et al; Lumina Study Group. Possible protective effect of hydroxychloroquine on delaying the occurrence of integument damage in lupus: LXXI, data from a multiethnic cohort. Arthritis Care Res (Hoboken). 2010;62(3):393–400. | ||
Doria A, Briani C. Lupus: improving long-term prognosis. Lupus. 2008;17(3):166–170. | ||
Wallace DJ. Antimalarials – the ‘real’ advance in lupus. Lupus. 2001;10(6):385–387. | ||
Ho KT, Ahn CW, Alarcón GS, et al. Systemic lupus erythematosus in a multiethnic cohort (LUMINA): XXVIII. Factors predictive of thrombotic events. Rheumatology (Oxford). 2005;44(10):1303–1307. | ||
Lakshminarayanan S, Walsh S, Mohanraj M, Rothfield N. Factors associated with low bone mineral density in female patients with systemic lupus erythematosus. J Rheumatol. 2001;28(1):102–108. | ||
Molad Y, Gorshtein A, Wysenbeek AJ, et al. Protective effect of hydroxychloroquine in systemic lupus erythematosus. Prospective long-term study of an Israeli cohort. Lupus. 2002;11(6):356–361. | ||
Tam LS, Gladman DD, Hallett DC, Rahman P, Urowitz MB. Effect of antimalarial agents on the fasting lipid profile in systemic lupus erythematosus. J Rheumatol. 2000;27(9):2142–2145. | ||
Belmont HM. Treatment of systemic lupus erythematosus – 2013 update. Bull Hosp Jt Dis (2013). 2013;71(3):208–213. | ||
Ruiz-Irastorza G, Ramos-Casals M, Brito-Zeron P, Khamashta MA. Clinical efficacy and side effects of antimalarials in systemic lupus erythematosus: a systematic review. Ann Rheum Dis. 2010;69(1):20–28. | ||
Apostolopoulos D, Hoi AY. Systemic lupus erythematosus – when to consider and management options. Aust Fam Physician. 2013;42(10):696–700. | ||
Contreras G, Pardo V, Leclercq B, et al. Sequential therapies for proliferative lupus nephritis. N Engl J Med. 2004;350(10):971–980. | ||
Ginzler EM, Dooley MA, Aranow C, et al. Mycophenolate mofetil or intravenous cyclophosphamide for lupus nephritis. N Engl J Med. 2005;353(21):2219–2228. | ||
Navarra SV, Guzmán RM, Gallacher AE, et al; BLISS-52 Study Group. Efficacy and safety of belimumab in patients with active systemic lupus erythematosus: a randomised, placebo-controlled, phase 3 trial. Lancet. 2011;377(9767):721–731. | ||
van Vollenhoven RF, Petri MA, Cervera R, et al. Belimumab in the treatment of systemic lupus erythematosus: high disease activity predictors of response. Ann Rheum Dis. 2012;71(8):1343–1349. | ||
Guidelines for referral and management of systemic lupus erythematosus in adults. American College of Rheumatology Ad Hoc Committee on Systemic Lupus Erythematosus Guidelines. Arthritis Rheum. 1999;42(9):1785–1796. | ||
Urowitz MB, Kagal A, Rahman P, Gladman DD. Role of specialty care in the management of patients with systemic lupus erythematosus. J Rheumatol. 2002;29(6):1207–1210. | ||
Molina MJ, Mayor AM, Franco AE, Morell CA, López MA, Vilá LM. Utilization of health services and prescription patterns among lupus patients followed by primary care physicians and rheumatologists in Puerto Rico. Ethn Dis. 2008;18(2 Suppl 2):S2–S205–S210. | ||
Vilá LM, Alarcón GS, McGwin G Jr, Bastian HM, Fessler BJ, Reveille JD; LUMINA Study Group. Systemic lupus erythematosus in a multiethnic cohort (LUMINA): XXIX. Elevation of erythrocyte sedimentation rate is associated with disease activity and damage accrual. J Rheumatol. 2005;32(11):2150–2155. | ||
Zink A, Fischer-Betz R, Thiele K, et al; German Collaborative Arthritis Centers. Health care and burden of illness in systemic lupus erythematosus compared to rheumatoid arthritis: results from the National Database of the German Collaborative Arthritis Centres. Lupus. 2004;13(7):529–536. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.