Back to Journals » International Medical Case Reports Journal » Volume 14
Drug-Resistant Tuberculosis Presenting as a Testicular Mass: A Case Report
Authors Nuwagira E , Yekosani M , Abraham B, Atwine R, Caleb T, Baluku JB
Received 11 January 2021
Accepted for publication 23 February 2021
Published 2 March 2021 Volume 2021:14 Pages 145—149
DOI https://doi.org/10.2147/IMCRJ.S300216
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Edwin Nuwagira,1 Mitala Yekosani,2 Birungi Abraham,2 Raymond Atwine,2 Tuhumwire Caleb,3 Joseph Baruch Baluku4
1Department of Medicine, Mbarara University of Science and Technology, Mbarara, Uganda; 2Department of Pathology, Mbarara University of Science and Technology, Mbarara, Uganda; 3Department of Surgery, Mbarara University of Science and Technology, Mbarara, Uganda; 4Division of Pulmonology, Mulago National Referral Hospital, Kampala, Uganda
Correspondence: Edwin Nuwagira
Mbarara University of Science and Technology, P.O Box 1410, Mbarara, Uganda
Tel +256 779096887
Email [email protected]
Background: Extrapulmonary drug-resistant tuberculosis is extremely rare and is almost always associated with poor treatment outcomes. This is partly due to the difficulty in confirming the diagnosis.
Case Presentation: A 40-year-old HIV-negative male presented with a painless scrotal mass, low-grade fever, general malaise, night sweats, and no pulmonary symptoms. He was initially treated for malaria with no improvement. His final diagnosis was rifampicin-resistant tuberculosis following Xpert® MTB/RIF Ultra (Xpert-Ultra) assay performed on a fine needle aspirate of the scrotal mass. Second-line anti-tuberculosis medication was initiated, and the patient is being followed up with directly observed therapy.
Conclusion: With the scale-up of Gene-Xpert technology, this case raises awareness about tuberculosis masquerading as a testicular mass and the possibility of extrapulmonary drug-resistant tuberculosis in high endemic areas.
Keywords: drug-resistant tuberculosis, genitourinary tuberculosis, extrapulmonary tuberculosis, tuberculous orchitis, sub-Saharan Africa, Uganda
Background
Anti-microbial resistance is a growing threat to the effective treatment of various pathogens.1 In particular, drug-resistant tuberculosis (DR-TB) is the leading contributor to antimicrobial resistance-related death globally, with only a 55% treatment success rate reported globally.2 The global prevalence of multidrug-resistant tuberculosis (MDR-TB) continues to rise and is of public health concern. In 2019 alone, there were about half a million new cases of rifampicin-resistant tuberculosis (RR-TB), of which bout 80% had MDR-TB.3
Extrapulmonary tuberculosis (EPTB), which is tuberculosis outside the lung parenchyma, constitutes 10–15% of all tuberculosis cases among HIV-negative adults and 60% in HIV-infected.4 Extrapulmonary drug-resistant tuberculosis is extremely rare and constitutes 5% of DR-TB.5 This is attributed to the low numbers of Mycobacterium tuberculosis present in the tissue and the inadequate diagnostics, especially in limited-resource settings.6 Genitourinary tuberculosis is one of the late manifestations of what was initially pulmonary tuberculosis infection. While cases of testicular and scrotal DR-TB have been described before, they are extremely rare, and there is no consensus on the appropriate management. One hospital-based cross-sectional in Uganda showed that approximately 10% (7 out of 73) of the patients presenting with testicular pain had tuberculous epididymo-orchitis.7 Here, we describe a case of a middle-aged HIV seronegative male with testicular RR-TB, who had no evidence of pulmonary involvement.
Case Presentation
This 40-years-old male presented with painless scrotal swelling that progressively increased in size for one month. He also had low-grade fever, general malaise, and night sweats, but denied a history of cough. He initially received Coartem®(Artemether/Lumefantrine) as a treatment for clinical malaria at a rural health facility where laboratory services are limited. The symptoms did not improve, and he was subsequently referred to Mbarara Regional Referral Hospital, a tertiary health care facility. He did not have any chronic illnesses and his serology for the Human Immunodeficiency Virus (HIV) had been done and documented as negative before referral. At the time of presentation, he worked as a mechanic and denied exposure to anyone with chronic cough or history of tuberculosis treatment. He was not a smoker or an alcoholic. He was married and denied having multiple sexual partners.
On examination, he was a well-nourished male, had a Bacillus Calmette Guerin (BCG) scar on his right deltoid, and his vitals were stable (Table 1).
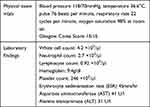 |
Table 1 Patient’s Characteristics |
The cardiovascular, neurological status, respiratory, and abdominal examination were all normal. The Chest X-ray was normal (Figure 1). His physical examination was significant for a fluctuant nontender left scrotal mass measuring 5cm × 8cm. It was neither translucent and nor ulcerated. A scrotal ultrasound scan showed a grossly enlarged left scrotum with a hyperechoic left testis. The right testis was normal. Fine needle aspiration revealed pus, which was positive on Xpert® MTB/RIF Ultra (Cepheid, Sunnyvale, CA, USA), with rifampicin resistance detected. A left orchidectomy was performed with clinical suspicion of a non-viable left testis, which was then sent for histopathology. The histopathology showed areas of caseous necrosis, granulomatous Langhan type giant cells, presence of mature lymphocytes and atrophic seminiferous vesicles, as shown in pictures A-D (Figure 2). The Ziehl-Neelsen (ZN) staining of the testis was negative. The patient was initiated on the non-injectable treatment protocol for DR-TB. He is now better on week 8 of treatment and the presenting symptoms; fever, night sweats, and general body weakness have since resolved.
 |
Figure 1 Normal chest X-ray. Histology of the left testis. |
Discussion
Genitourinary drug-resistant tuberculosis is extremely rare and often presents with vague symptoms, which poses a diagnostic challenge, especially in a low resource setting.4,8 The exact prevalence is unknown but is about 2–5% of DR-TB.6 Males are the most affected,9 and the commonest sites affected are the epididymides, followed by seminal vesicles, prostate, testis, and then vas deferens.10
Genitourinary DR-TB has been reported before in a case report, although the diagnosis was confirmed from respiratory specimens.4 In our patient who did not have any respiratory symptoms, making a diagnosis of extrapulmonary DR-TB was extremely difficult in a setting with limited laboratory and bronchoscopy services. Moreover, the mechanism of infection in our patient remains unknown but several mechanisms of dissemination of tuberculosis to the testis are mentioned in the medical literature. These include the local spread of infection, retrograde spread of the Mycobacteria tuberculosis bacilli from an infected urinary tract into the prostate, hematogenous and lymphatic spread of the bacilli from the lungs6,11. Fittingly, there are a few reported cases of sexual transmission of urogenital tuberculosis.12
Histopathology can be used to diagnose extrapulmonary tuberculosis. In our patient, the histopathologic examination revealed caseous necrosis, classic Langhans giant cells, and atrophic seminiferous tubules, as shown in Figure 2. While these are good diagnostic modalities, they would not differentiate drug-sensitive from drug-resistant tuberculosis.
The use of imaging in the diagnosis of TB-orchitis has been previously described, but, apart from a military pattern, the other findings are nonspecific to tuberculosis-orchitis.13 Patients may also present without respiratory symptoms and hence a normal chest radiograph, as seen in our scenario, Figure 1. The sonographic findings mimic other diagnoses such as tumors, infarcts, inflammation, and trauma.14
Pharmacological therapy is the mainstay of treatment and is analogous to pulmonary tuberculosis treatment. Currently, the World Health Organization(WHO) recommends injectable free regimens in the treatment of uncomplicated DR-TB,15 based on studies done in sub-Saharan Africa.16 In Uganda, we give a combination of Bedaquilline, Linezolid, Levofloxacin, Clofazimine, and Cycloserine for nine months (the modified short regimen). Due to the lack of a proper regimen, our patient is currently taking this injectable-free regimen that is recommended by the WHO for the treatment of pulmonary disease. While the risk of extrapulmonary tuberculosis increases with the levelof immunosuppression in people living with HIV,8 the patient in our case vignette was immunocompetent which makes this case unique. Generally, extrapulmonary drug-resistant tuberculosis has a good prognosis but, after treatment-follow up is required for urogenital tuberculosis for at least five years.17 Tuberculosis of the testis has mimics such as other chronic granulomatous diseases like Sarcoidosis and brucellosis, primary testicular tumors, lymphomas, and adrenal rests.14 Good knowledge of the epidemiology and appropriate diagnostic tests is essential to avoid unnecessary orchidectomy.
Conclusion
Tuberculosis should be considered while assessing a scrotal swelling or chronic epididymo-orchitis of a patient from a high TB endemic area like ours. The use of Xpert® MTB/RIF Ultra (Xpert Ultra) is an essential point-of-care test in identifying extra-pulmonary rifampicin-resistant tuberculosis, which is crucial in the choice of treatment.
Abbreviations
ALT, Alanine Transaminase; AST, Aspartate Aminotransferase; DR-TB, Drug-Resistant Tuberculosis; EPTB, Extra-Pulmonary Tuberculosis; ESR, Erythrocyte Sedimentation Rate; TB, Tuberculosis; WHO, World Health Organization; ZN, Ziehl-Neelsen.
Ethical Approval
Not applicable from the Institutional review board, but, we obtained written informed consent from the patient for publication of this case, his details and accompanying images.
Acknowledgments
The authors would like to thank the nurses and clinicians at the tuberculosis treatment unit of Mbarara Regional Referral Hospital.
Author Contributions
All authors made a significant contribution to the work reported that is in data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
No funding was received to have this manuscript written or published.
Disclosure
The authors have no conflicts of interest to declare for this work.
References
1. World Health Organization. Antimicrobial Resistance: Global Report on Surveillance. World Health Organization; 2014.
2. World Health Organization. Global Tuberculosis Report 2019. Geneva (Switzerland): World Health Organization; 2019.
3. WHO. Tuberculosis (TB) [Internet]. 2020. (TB and HIV, and other comorbidities). Available from: https://www.who.int/tb/areas-of-work/tb-hiv/en/.
4. Desai U, Joshi JM. Extrapulmonary drug-resistant tuberculosis at a drug-resistant tuberculosis center, Mumbai: our experience–hope in the midst of despair! Lung India Off Organ Indian. Chest Soc. 2019;36(1):3.
5. Lawn SD, Zumla AI. Diagnosis of extrapulmonary tuberculosis using the Xpert ® MTB/RIF assay. Exp Rev Anti Infect Ther. 2012;10(6):631–635. doi:10.1586/eri.12.43
6. Seo JW, Park CJ, Kim TK, et al. Testicular tuberculosis in multidrug-resistant pulmonary tuberculosis. J Infect Chemother. 2013;19(4):767–769. doi:10.1007/s10156-012-0508-2
7. Opio J, Byanyima R, Kiguli-Malwadde E, Kaggwa S, Kawooya M. The sonographic pattern of diseases presenting with scrotal pain at Mulago Hospital, Kampala, Uganda. East Cent Afr J Surg. 2008;13(2):68–74.
8. Golden MP, Vikram HR. Extrapulmonary tuberculosis: an overview. Am Fam Physician. 2005;72(9):1761–1768.
9. Hadadi A, Pourmand G, Mehdipour-Aghabagher B. Unilateral testicular tuberculosis: case report. Andrologia. 2012;44(1):70–72. doi:10.1111/j.1439-0272.2010.01097.x
10. Jumbi T, Mugo R, Onkunya L, et al. Testicular tuberculosis can mimic a testicular tumor. J Pediatr Surg Case Rep. 2019;41:43–45. doi:10.1016/j.epsc.2018.11.009
11. Das A, Batabyal S, Bhattacharjee S, Sengupta A. A rare case of isolated testicular tuberculosis and review of literature. J Fam Med Prim Care. 2016;5(2):468. doi:10.4103/2249-4863.192334
12. Angus BJ, Yates M, Conlon C, Byren I. Cutaneous tuberculosis of the penis and sexual transmission of tuberculosis confirmed by molecular typing. Clin Infect Dis. 2001;33(11):e132–4. doi:10.1086/324360
13. Drudi F, Laghi A, Iannicelli E, et al. Tubercular epididymitis and orchitis: US patterns. Eur Radiol. 1997;7(7):1076–1078. doi:10.1007/s003300050257
14. Nepal P, Ojili V, Songmen S, Kaur N, Olsavsky T, Nagar A. “The great masquerader”: sonographic pictorial review of testicular tuberculosis and its mimics. J Clin Imaging Sci. 2019:9.
15. Migliori GB, Tiberi S, Zumla A, et al. MDR/XDR-TB management of patients and contacts: challenges facing the new decade. The 2020 clinical update by the Global Tuberculosis Network. Int J Infect Dis. 2020;92:S15–25. doi:10.1016/j.ijid.2020.01.042
16. Mohr-Holland E, Reuter A, Furin J, et al. Injectable-free regimens containing bedaquiline, delamanid, or both for adolescents with rifampicin-resistant tuberculosis in Khayelitsha, South Africa. EClinicalMedicine. 2020;20:100290. doi:10.1016/j.eclinm.2020.100290
17. Figueiredo AA, Lucon AM, Junior RF, Srougi M. Epidemiology of urogenital tuberculosis worldwide. Int J Urol. 2008;15(9):827–832. doi:10.1111/j.1442-2042.2008.02099.x
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

