Back to Journals » Patient Preference and Adherence » Volume 13
Divergence in perceptions of diabetes control among patients with type 2 diabetes mellitus treated with basal insulin and health care professionals: results from the US Perceptions of Control (POC-US) study
Authors Tomaszewski KJ, Allen A, Mocarski M , Schiffman A , Kruger D, Handelsman Y , Heile M , Brod M
Received 14 November 2018
Accepted for publication 10 April 2019
Published 10 May 2019 Volume 2019:13 Pages 761—773
DOI https://doi.org/10.2147/PPA.S194598
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Kenneth J Tomaszewski,1 Amy Allen,1 Michelle Mocarski,2 Alisa Schiffman,2 Davida Kruger,3 Yehuda Handelsman,4 Michael Heile,5 Meryl Brod6
1KJT Group, Inc., Honeoye Falls, NY, USA; 2Novo Nordisk Inc., Plainsboro, NJ, USA; 3Henry Ford Health System, Detroit, MI, USA; 4Metabolic Institute of America, Tarzana, CA, USA; 5TriHealth, Cincinnati, OH, USA; 6The Brod Group, Mill Valley, CA, USA
Background: Approximately 60% of the patients with type 2 diabetes mellitus (T2DM) on basal insulin have an HbA1c ≥7%. This analysis of the US Perceptions of Control (POC-US) study aimed to understand US patient and health care professional (HCP) views of diabetes “control,” which may play a role in whether patients reduce their HbA1c or achieve HbA1c <7%.
Methods: A cross-sectional, Web-based survey of 500 US HCPs (primary care physicians, endocrinologists, nurse practitioners/physician assistants) and 618 US adults with T2DM using basal insulin was conducted to assess perceptions, attitudes, and behaviors associated with T2DM management. The survey was developed from previous research examples and qualitative exploratory research and was pretested. Patients self-reported their most recent HbA1c level and confirmed this value with their HCP, if necessary.
Results: Patients and HCPs differed on some definitions of “in control.” HbA1c value was used most often by both populations, but more frequently by HCPs (91% vs 69%). Patients also often used behavioral criteria (eg, adherence to lifestyle changes and/or treatment regimens), and HCPs often used clinical criteria (eg, hypoglycemia). Most HCPs focused on the last 3 months to define control (67% vs 34% patients; P<0.05), whereas patients more frequently reported focusing on “the current moment” or “the past week.” Patients were more likely to agree that controlling their condition is “completely the patients’ responsibility” (patients, 67%; HCPs, 34%; P<0.05); HCPs were more likely to agree that they have “a responsibility to actively contribute to the control of their patients’ T2DM” (90% vs 60%; P<0.05).
Conclusion: US patients with T2DM have differing views from HCPs on key aspects of diabetes control and management and are less likely to consider HbA1c value as a criterion for determining control. Recognizing and addressing these differences may improve patient-HCP communication and may potentially improve patient outcomes.
Keywords: Diabetes control, diabetes management, diabetes perceptions
Introduction
Diabetes is one of the most common chronic diseases in the United States, affecting approximately 30.3 million people, and type 2 diabetes mellitus (T2DM) accounts for an estimated 90% to 95% of all diabetes cases.1 The American Diabetes Association (ADA) recommends a hemoglobin A1c (HbA1c) goal of <7% (53 mmol/mol) for most adults with diabetes; however, one’s target HbA1c may be higher or lower depending on the individual patient’s circumstances such as severe hypoglycemia or extensive comorbidities.2 Patients who are unable to achieve their target HbA1c may face an increased risk for the development and progression of diabetic complications, and may potentially benefit from improved dialogue with their health care professionals (HCPs) and/or treatment escalation.
Productive communication between HCPs and patients with T2DM regarding treatment decisions and other management considerations is essential to successful diabetes care.2 Studies suggest, however, that there is a disconnect between how HCPs and patients with T2DM perceive control of T2DM, which may contribute to suboptimal control and ineffective management of the disease.3–9 Results from the European Perceptions of Control study, which compared the perceptions of diabetes control between HCPs and patients with poorly controlled T2DM (HbA1c >8%) who were receiving basal insulin, revealed that HCPs tended to define control in terms of clinically measurable outcomes, whereas patients focused on the amount of daily insulin used and the impact of diabetes on their daily lives.3 Results of this study demonstrated that there are important differences in perceptions of control of T2DM between HCPs and patients with uncontrolled T2DM, including the definition of control, the time frame in which control of T2DM is considered, and the obstacles associated with T2DM control.3
The US-based POC study (POC-US) was developed from US-based exploratory research as well as the European Perceptions of Control study, and builds upon the work previously conducted outside the US, but with a focus on patient demographics and provider types that are uniquely US focused. It aimed to identify whether perceptions of T2DM control vary between patients receiving basal insulin (with or without oral antidiabetic drugs) and HCPs in the US health care system. Previous research indicates that approximately 60% of the patients with T2DM who receive basal insulin with or without concomitant oral antidiabetic drugs are not well controlled,10 suggesting important opportunities to improve management of this patient population. Here we present results from POC-US, which may be used to promote more collaborative relationships between patients and HCPs, ultimately resulting in improved care, support for patients with T2DM, and clinical outcomes.
Methods
Study design and survey development
Two Internet-based surveys were conducted; one was administered to patients with T2DM using basal insulin with or without oral antidiabetic medication, and a separate survey was administered to HCPs in the United States. The patient survey was conducted between October 26, 2016, and October 9, 2017, and the HCP survey was conducted between October 18, 2016, and November 16, 2016. The patient survey was offered in both English and Spanish and took approximately 30 mins to complete. The survey for HCPs took approximately 20 mins to complete. Surveys were developed, in part, by replicating key domains of the European Perceptions of Control study and were then further tailored to the US population. Survey development also incorporated findings from a qualitative research phase and insights from in-person focus groups of patients (n=23) and HCPs (n=28), as well as in-depth telephone interviews with pharmacy benefit managers and individuals from managed care organizations and integrated delivery networks (n=20). Pretests were conducted to confirm language and understanding (60-min test for patients [n=7] and 60-min test for HCPs [n=6]). Study and survey instruments were approved by the Copernicus Group Institutional Review Board (One Triangle Drive, Suite 100, Durham, NC 27713; mailing address: P.O. Box 110605, Research Triangle Park, NC, 27709). Consent was obtained in the introduction to the survey instrument.
Recruitment
For surveys and patient recruitment, HCPs were recruited via email, United States Postal Service mail, and/or telephone through an online panel company with which respondents had provided permission to be contacted for research purposes or through the American Medical Association Masterfile. The HCP sample was monitored to ensure broad coverage across roles, regions, and years in practice. Patients were recruited in any of the following ways: 1) via email and/or telephone through an online panel company with which respondents had provided permission to be contacted for research purposes; 2) through a Meijer brand grocery store pharmacist; or 3) through an invitation given to them by their HCP. Online panel and Meijer respondents were requested to exit the survey and obtain their most recent HbA1c value from their HCP prior to completion of the full survey, and patients who were invited by their provider were able to continue immediately to the survey if their HCP had provided them with their HbA1c value.
The proportion of invited patient panel respondents who attempted to enter the survey was 28.6% and comprised 33% of the final interviews (n=201). Non-panel participants were recruited through 120 HCPs and 20 Meijer brand grocery store pharmacy locations, with an estimated response rate of 7.4% from these locations. These non-panel patient sources, however, comprised the greatest proportion of final respondents (67%). Meijer brand grocery store pharmacist-sourced respondents accounted for less than 1% of the final interviews (n=3). The greatest proportion of respondents was recruited by invitation from their HCP, accounting for 67% of the sample (n=414).
Of respondents that completed the screener (n=9,643) only 7.2% qualified for the study. The largest exclusion categories were treatment type (56.6% of excluded respondents) and other health conditions (17.1% of excluded respondents). Among HCPs, the participation rate was 15%.
Inclusion criteria
Inclusion criteria are diagrammed in Figure S1. To participate in the patient survey, individuals were required to be diagnosed with T2DM, between the ages of 35 and 70 years, living in the United States, and willing to provide information regarding their income and ethnicity. This age range was selected to target the age groups most likely to participate based on the mode of survey administration coupled with the rigorous screening and informed consent procedure. Respondents were required to be receiving basal insulin, with or without oral antidiabetic drugs. In addition, some respondents (see above) were required to contact their HCP to confirm their HbA1c value (measured within the previous 6 months) to be able to report their HbA1c value in the survey.
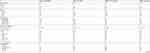
 | Figure 1 Definitions of being in control.Note: *P<0.05 vs HCPs.Abbreviations: T2DM, type 2 diabetes mellitus; HCPs, health care professionals. |
To participate in the HCP survey, respondents were required to be either a board-certified physician (in practice for 3–40 years) or a nurse practitioner (NP) or physician assistant (PA) (in practice for 3–35 years) in the United States, excluding Vermont, and excluding those who practiced in a government or Veterans Affairs hospital, due to the unique payment systems of these entities. HCPs were required to have seen at least 50 patients with T2DM in the past month and to have been treating patients with T2DM for at least 3 years. Primary care physicians (family physicians, general physicians, and internal medicine specialists) were required to be treating an average of at least 20 patients with T2DM per month with at least 5 patients receiving only basal insulin, and to have personally managed their patients’ insulin therapy decisions. Endocrinologists were required to have endocrinology as their primary specialty and to be treating an average of at least 50 patients with T2DM per month with at least 20 patients with T2DM on basal insulin only. For NPs and PAs, their primary specialty had to be family practice, general practice, or internal medicine, and they were required to be caring for an average of at least 20 patients with T2DM per month with at least 5 patients receiving only basal insulin.
Data analysis
The survey only collected information pertinent to the purpose of the study and did not collect any names or other identifying information. Survey data included patient/HCP demographic information, definitions of T2DM being “in control” (selected from a prespecified list), the time frame considered when defining control, and agreement with various statements related to one’s attitude towards control and T2DM management (using a 5-point scale from 1, “strongly disagree,” to 5, “strongly agree”). Agreement data were analyzed by post hoc grouping of responses as “disagree” (1–2), “neutral” (3), and “agree” (4–5). Data are presented as mean and median values, or as percentages. Patient and HCP responses were compared via chi-square test, and statistical significance was defined by P<0.05.
Results
Patient demographics
Patients were recruited through an online panel or by their HCP or pharmacist. In total, 618 patients completed the online survey (HbA1c <7%, n=231; HbA1c 7%–7.99%, n=194; HbA1c ≥8%, n=193) (Table 1). The mean age of respondents was 53.9 years, and 46% were female. Respondents reported a mean (median) of 9.0 (7.0) years since they were first diagnosed with T2DM. A majority (76%) of respondents were white, and 26% reported having a bachelor’s degree. Of those patients who reported that they were currently taking fast-acting bolus insulin (n=198), 28% had an HbA1c level of <7%, 26% had an HbA1c level of 7% to 7.99%, and 46% had an HbA1c level of ≥8%. Of note, on average, patients who were taking fast-acting insulin had received their T2DM diagnosis earlier than those who were not (mean, 10.7 vs 8.2 years). A minority (32%) of respondents needed and were willing to contact their HCP to confirm their most recent HbA1c value. Prior to contacting their HCP, these respondents reported an average HbA1c value of 7.7%, based on recall of the most recent value given to them by their HCP. After contacting their HCP, these respondents reported an average HbA1c value of 7.6%. Approximately half (51%) of these respondents reported no difference between the recalled HbA1c value and the value provided by their HCP; the standard deviation of this difference was 0.9 with a maximum of 9.6.
 | Table 1 Patient demographics |
HCP demographics
In total, 500 HCPs completed the survey (PCPs, n=280; endocrinologists, n=150; NPs/PAs, n=70) of whom 37% reported specializing in family practice, 31% in internal medicine, 30% in endocrinology, and 2% in general practice (Table 2). A majority (81%) of respondents reported practicing in a privately owned office or clinic. Thirty-four percent of respondents reported that they had been practicing for 22 or more years. Most respondents (82%) did not have a specific diabetes certification, however, 12% reported being a “Certified Diabetes Educator” and 11% reported being certified in “Advanced Diabetes Management.”
 | Table 2 HCP demographics |
Definitions of being in control (all patients)
Both patients and HCPs selected “what my/their HbA1c value is” most frequently when asked about which criteria they use to determine if their/their patients’ T2DM is in control (Figure 1); however, HCPs were more likely to use this criterion to define T2DM control. Nearly all HCPs (91%) reported defining control of T2DM by their patients’ HbA1c values, compared with 69% of the patients (P<0.05). Patients with lower HbA1c values were more likely to use Hb1Ac value to define T2DM control (73%, A1c <7% and 72%, A1c 7%–7.99% vs 62%, A1c ≥8%; P<0.05). HCPs were significantly more likely than patients to report determining their patients’ control of T2DM based on whether they were having complications from their diabetes (62% of HCPs vs 37% of patients; P<0.05). Clinical criteria such as frequency of episodes of high blood sugar and severity of high blood sugar episodes were significantly more likely to be used as a definition of control by HCPs than patients (frequency, 68% for HCPs vs 55% for patients; severity, 61% for HCPs vs 46% for patients; P<0.05). Patients were more likely than HCPs to use definitions of control related to adherence, such as whether they are eating a healthy diet (57% for patients vs 48% for HCPs; P<0.05) and how much insulin they take daily (43% for patients vs 26% for HCPs; P<0.05). In comparison with HCPs, patients were more likely to define TD2M control based on how high or low their energy levels are (29% for HCPs vs 37% for patients; P<0.05).
Time frame used when defining control of T2DM
Although both patients and HCPs most frequently selected the last 3 months as the time frame considered when assessing level of control, HCPs were significantly more likely than patients to focus on this time frame (67% of HCPs vs 34% of patients; P<0.05) (Figure 2). Patients with lower A1c levels were more likely to focus on the last 3 months when assessing level of control (36%, A1c <7% and 38%, A1c 7%–7.99% vs 27%, A1c ≥8%; P<0.05). In contrast, patients were more likely than HCPs to be focused on a more recent time frame when considering control. Seven percent of patients reported focusing on the current moment (vs 2% of HCPs; P<0.05), 9% of patients focused on the past 24 hrs (vs 1% of HCPs; P<0.05), and 13% of patients reported focusing on the last week (vs 4% of HCPs; P<0.05).
 | Figure 2 Time frame when considering level of control.Note: *P<0.05 vs HCPs.Abbreviation: HCP, health care professional. |
Attitudes toward T2DM control
Patients were more likely than HCPs to agree that they know how to control their T2DM (77% of patients vs 57% of HCPs who agreed that their patients know how to control their T2DM; P<0.05) (Figure 3). Patients were more likely to agree that they are motivated to control their T2DM (71% of patients vs 54% of HCPs who agreed that their patients are motivated to control their T2DM; P<0.05). Sixty-two percent of HCPs were likely to agree that their patients know how to control their T2DM but lack the motivation to actually do it, whereas 44% of patients agreed that they know how to control their T2DM but cannot seem to make themselves actually do it (P<0.05). Approximately half (49%) of patients agreed that their T2DM is completely in their control compared with 37% of HCPs who agreed that T2DM is completely in their patients’ control.
 | Figure 3 Patient and HCP attitudes toward T2DM: state of control.Note: *P<0.05 vs HCPs.Abbreviations: T2DM, type 2 diabetes mellitus; HCP, health care professional. |
Attitudes toward T2DM responsibility and support
Patients’ attitudes toward responsibility for control differed from those of HCPs, with patients being more likely to agree that controlling their diabetes is completely their responsibility (67% of patients vs 34% of HCPs; P<0.05) (Figure 4). Significantly more HCPs than patients agreed that HCPs have a responsibility to actively contribute to the control of their patients’ T2DM (90% of HCPs vs 60% of patients; P<0.05). Fifty-nine percent of HCPs agreed that their patients’ family and friends have a responsibility to actively contribute to control of their patients’ T2DM, whereas 32% of patients agreed that their family and friends have a responsibility to actively contribute to control of their T2DM (P<0.05). A significantly higher percentage of HCPs (33%) agreed that their patients lack the support to control their T2DM compared with 19% of patients who agreed that they lack the support (P<0.05).
 | Figure 4 Patient and HCP attitudes towards T2DM responsibility and support.Note: *P<0.05 vs HCPS. Abbreviations: T2DM, type 2 diabetes mellitus; HCP, health care professional. |
Discussion
Overall, the results of the POC-US study reveal several important differences between the criteria that HCPs and patients use to define control of T2DM. For example, HCPs were more likely than patients to consider clinical measures to determine whether their patients’ T2DM is in control, such as their patients’ HbA1c values or the frequency and severity of their patients’ episodes of hyperglycemia. In contrast, patients were more likely than HCPs to consider a more varied definition of control, and they tended to focus on aspects of their everyday lives including how high or low their energy levels are, the amount of insulin taken daily, their weight, and the amount of time they spend thinking about diabetes. Similarly, patients in the European Perceptions of Control study differed from HCPs in that they tended to define control by the quantity of insulin units per day and more broadly in terms of the impact of T2DM on their quality of life (eg, energy levels, how predictable life is, and how much they think about their disease).3
Regarding the time frame considered when defining control of T2DM, previous studies suggest that patients with T2DM may often think about control on a daily or weekly basis because of a greater focus on the impact of the disease on their lives, in contrast with physicians, who tend to think about control in terms of a 3-month period (consistent with how HbA1c is measured).3 Findings from the POC-US study were similar in that HCPs were more likely than patients to consider the last 3 months as the time frame for defining control, and higher percentages of patients than HCPs considered shorter time frames such as the current moment, the last 24 hrs, and the last week. Patients and HCPs also differed in their attitudes towards the state of T2DM control (ie, whether patients know how to control their T2DM) and towards responsibility and support for T2DM control (ie, whether control of T2DM is completely the patient’s responsibility). Patients were significantly more likely than HCPs to agree that they know how to control their T2DM and also were more likely than HCPs to agree that they are motivated to control their diabetes. Regarding responsibility for controlling T2DM, patients were less likely than HCPs to agree that their doctor has a responsibility to actively contribute to controlling their T2DM. These results suggest that HCPs may underestimate the perceived level of control their patients believe they have over their T2DM, and potentially overestimate the responsibility that their patients think HCPs should have in actively contributing to controlling their T2DM. Opportunities may exist to educate patients on the supportive resources that HCPs are able to provide and to encourage patients to engage more productively with their health care teams, to lessen the individual burden they may feel in managing their care.
Differing perceptions of T2DM control between HCPs and patients described in other studies3–9 that focused on different patient populations (eg, European, insulin-naïve) are consistent with the results of this study. HCPs may not be aware of the extent to which patients feel responsible for controlling their T2DM, potentially contributing to misalignment in expectations and lack of efficient communication. Studies indicate the importance of HCP support for patients with T2DM and education around self-management of diabetes in improving adherence and glycemic control.2,11,12 Recognition of the differences in perceptions of T2DM control between HCPs and patients highlighted by the POC-US study may be leveraged to enhance communication and enable HCPs to have more productive conversations with their patients, ultimately improving clinical outcomes and patient care. For example, understanding patient perspectives and attitudes toward their diabetes may help HCPs to facilitate a patient-centered communication style that assesses patient-specific barriers to care, an approach that is recommended by the American Diabetes Association for optimizing patient health outcomes and health-related quality of life.2 More specifically, using a nonjudgmental approach, empathizing, using active listening techniques, and managing patients’ perceptions about their ability to self-manage their diabetes may be important strategies to facilitate collaborative patient relationships. Interestingly, the European Perceptions of Control study, which compared perceptions of control between HCPs and patients with uncontrolled T2DM (HbA1c >8%), seemed to indicate even greater discrepancies in patient vs HCP definitions of control and the time frame of control,3 suggesting that patient-HCP alignment may be associated with improved clinical outcomes (ie, lower HbA1c). This is also consistent with our findings that lower HbA1c levels correlated with higher agreement with HCPs regarding definitions and time frame of control.
Limitations of this study may include the self-reported nature of the survey; however, this type of instrument was necessary to collect inherently subjective data and is consistent with previous studies assessing patient perceptions of control.3,4,6,8 Low participation rates are a potential limitation of the study, as selection criteria excluded a majority of potential respondents. To obtain results that better represent the target demographic, we employed a stratified approach to recruit patients from 3 distinct sources; however, this does not exclude the potential for recruitment bias. The patient population may also be biased towards more engaged patients who are willing to take a survey related to T2DM, and thus may not be reflective of the entire population of patients with T2DM. Relatively disengaged patients may be less aligned with HCPs and as a result, the study may underestimate the differences in perceptions between patients and providers. The patient and physician populations may have been subject to other selection biases such as those related to the online nature of the survey, in which less technologically savvy individuals may have been excluded. Additionally, notable demographic characteristics of the survey populations that may have affected the results include the high proportion of patients who were of white ethnicity (76%) and the length of time many HCPs reported being in practice (17 years or more, 58%). Patients reporting an HbA1c level of <7% appeared to have greater rates of advanced education (some graduate school or higher), suggesting that education may play a role in influencing patients’ approaches towards managing their disease.
Conclusion
In the POC-US study, patients with T2DM and HCPs differed in their views regarding key aspects of diabetes control and management, and patients were found to be less likely than HCPs to consider their HbA1c value as a criterion for determining control. Recognizing these differences in perceptions between patients and HCPs may provide insights for strategies to improve communication, with the potential to ultimately improve patient outcomes.
Acknowledgments
Writing assistance was provided by Jessica Monteith, PhD, of ETHOS Health Communications in Yardley, PA, USA, and was supported financially by Novo Nordisk Inc., Plainsboro, NJ, USA, in compliance with international Good Publication Practice guidelines. An abstract of this study was presented at the American Diabetes Association’s 78th Scientific Sessions as a poster presentation and is available at
Disclosure
KJ Tomaszewski is an employee of KJT Group, which provides paid research services to Novo Nordisk. A Allen is an employee of KJT Group, which provides paid research services to Novo Nordisk. M Mocarski is an employee of Novo Nordisk Inc. and a stockholder of Novo Nordisk A/S. A Schiffman is an employee of Novo Nordisk Inc. and a stockholder of Novo Nordisk A/S. D Kruger is a consultant and speaker for Novo Nordisk, and her institution receives research funding from Novo Nordisk. Y Handelsman has received research grants and consultant and speaker honoraria from Aegerion, Amarin, Amgen, AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Boehringer Ingelheim-Lilly, Gan & Lee Pharmaceutical, Gilead, Hanmi, Janssen, Lexicon, Lilly, Merck, Merck-Pfizer, Mylan, Novo Nordisk, Regeneron, and Sanofi. M Heile is an advisor for Bigfoot Biomedical Company, Janssen Pharmaceutical, Novo Nordisk, and Roche Diagnostics and a speaker for Insulet Corporation, Janssen Pharmaceutical, and Novo Nordisk. M Brod is a paid consultant for Novo Nordisk. A Allen reports professional fees for design and execution of supporting research from Novo Nordisk, during the conduct of the study. D Kruger reports grants and personal fees from Novo Nordisk, outside the submitted work. Y Handelsman reports grants and personal fees from Amgen, AstraZeneca, Merck, Janssen, Novo Nordisk, and Sanofi; and grants from BMS, BI, Gan & Lee, Hamni, Lexicon, and Mylan, personal fees from Aegerion, Amarin, Gilead, Intarcia, and Regeneron, outside the submitted work. M Heile served as an advisor and member of the speakers bureau for Novo Nordisk, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1.
2.
3. Brod M, Pfeiffer KM, Barnett AH, Berntorp K, Vilsboll T, Weissenberger B. Perceptions of diabetes control among physicians and people with type 2 diabetes uncontrolled on basal insulin in Sweden, Switzerland, and the United Kingdom. Curr Med Res Opin. 2016;32(6):981–989. doi:10.1185/03007995.2016.1150821
4. Fitzgerald JT, Stansfield RB, Tang T, et al. Patient and provider perceptions of diabetes: measuring and evaluating differences. Patient Educ Couns. 2008;70(1):118–125. doi:10.1016/j.pec.2007.09.005
5. Freeman J, Loewe R. Barriers to communication about diabetes mellitus. Patients‘ and physicians‘ different view of the disease. J Fam Pract. 2000;49(6):507–512.
6. Gopalan A, Moss H, Tao Y, Zhu J, Volpp K. Patient perceptions of current disease control in poorly controlled diabetes. Health. 2014;6:1964–1971. doi:10.4236/health.2014.615230
7. Jack L Jr, Liburd LC, Tucker P, Cockrell T. Having their say: patients‘ perspectives and the clinical management of diabetes. Clin Ther. 2014;36(4):469–476. doi:10.1016/j.clinthera.2014.02.003
8. McAndrew LM, Horowitz CR, Lancaster KJ, Leventhal H. Factors related to perceived diabetes control are not related to actual glucose control for minority patients with diabetes. Diabetes Care. 2010;33(4):736–738. doi:10.2337/dc09-1229
9. Stiffler D, Cullen D, Luna G. Diabetes barriers and self-care management: the patient perspective. Clin Nurs Res. 2014;23(6):601–626. doi:10.1177/1054773813507948
10. Giugliano D, Maiorino MI, Bellastella G, Chiodini P, Ceriello A, Esposito K. Efficacy of insulin analogs in achieving the hemoglobin A1c target of <7% in type 2 diabetes: meta-analysis of randomized controlled trials. Diabetes Care. 2011;34(2):510–517. doi:10.2337/dc10-1710
11. Brunisholz KD, Briot P, Hamilton S, et al. Diabetes self-management education improves quality of care and clinical outcomes determined by a diabetes bundle measure. J Multidiscip Healthc. 2014;7:533–542. doi:10.2147/JMDH.S69000
12. Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25(7):1159–1171.
Supplementary material
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

