Back to Journals » Psychology Research and Behavior Management » Volume 13
Diabetes-Related Distress and Depression in Saudis with Type 2 Diabetes
Authors Alzughbi T, Badedi M , Darraj H , Hummadi A, Jaddoh S, Solan Y, Sabai A
Received 26 March 2020
Accepted for publication 8 May 2020
Published 15 May 2020 Volume 2020:13 Pages 453—458
DOI https://doi.org/10.2147/PRBM.S255631
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Einar Thorsteinsson
Turki Alzughbi,1 Mohammed Badedi,1 Hussain Darraj,1 Abdulrahman Hummadi,1 Sattam Jaddoh,2 Yahiya Solan,1 Abdullah Sabai3
1Jazan Diabetes and Endocrine Center, Jazan Health Affairs, Jazan, Saudi Arabia; 2Jazan Psychiatry Hospital, Jazan Health Affairs, Jazan, Saudi Arabia; 3Public Health Administration, Jazan Health Affairs, Jazan, Saudi Arabia
Correspondence: Turki Alzughbi
Jazan Diabetes Center, Ministry of Health, Jazan, Saudi Arabia
Email [email protected]
Objective: This study aims to assess the prevalence of diabetes mellitus (DM)-related distress and depression and their associated factors in Saudi people with type 2 DM (T2DM) in Jazan, Saudi Arabia. It also aims to assess the association between glycemic control and DM-related distress and depression.
Methods: This is an analytical, cross-sectional study which recruited 300 Saudi patients with T2DM randomly from primary healthcare centers in Jazan, Saudi Arabia. DM-related distress and depression were measured by valid questionnaires, the 17-item Diabetes Distress Scale and the Patient Health Questionnaire-9, respectively. Logistic regression and an independent t-test were performed in the statistical analysis.
Results: The mean age of the study population was 52.7 years, with a range of 23– 83 years. The number of males was 147 (49%) and females was 153 (51%) in the study population. The prevalence of DM-related distress and depression in Saudi patients with T2DM in Jazan was 22.3% and 20%, respectively, and about 7.7% had both. Of DM-related distress, 12.3% had interpersonal-related DM distress, 11.7% had physician-related DM distress, 10.7% had emotional-related DM distress, and 7% had regimen-related DM distress. After adjusting for covariates, being female, patients aged < 45, physical inactivity, DM duration < 5 years, and smoking were significantly associated with DM-related distress and depression. There was also a significant association between DM-related distress and depression, OR = 3 [95% CI: 1.8, 6.4]. Furthermore, we found that glycated hemoglobin (A1C) levels were significantly higher in those with DM-related distress (small effect size, eta squared = 0.04) and depression (moderate effect size, eta squared = 0.06) (P < 0.001).
Conclusion: DM-related distress and depression are prevalent in patients with T2DM in Jazan, Saudi Arabia. Both these conditions need to be screened for and addressed in clinical settings. Establishing the causality of DM-related distress and depression in T2DM is an important aim for any future studies.
Keywords: type 2 diabetes, diabetes distress, depression
Introduction
Diabetes mellitus (DM) is a chronic condition that has a considerable impact on physical and psychosocial health.1 It is characterized by chronic high levels of glucose in the blood (hyperglycemia) that require long-term intensive care to reduce the risk of fatal complications.2 In Saudi Arabia, the prevalence of type 2 DM was 18.3%.1 Patients with DM experience psychological difficulties related to their chronic DM and being worried about the risk of complications.3 DM-related distress refers to the emotions related to living with and managing the disease.4 Depression is a mental disorder characterized by sadness and a lack of interest.5 DM-related distress and depression are prevalent among patients with type 2 DM (T2DM)6 and may become serious problems if they impair the motivation for self-care. Despite the correlation between DM distress and depression, it has been found that DM distress is more widespread than depression in people with DM and has a greater impact on self-care6 and glycemic control.7 Many studies have assessed the prevalence of DM distress and depression among people with T2DM, but most of these have been in Western countries. Because there are so many sociocultural and religious differences among populations, further studies are needed to assess DM distress and depression, particularly in large countries such as Saudi Arabia. To our knowledge, no study has measured the prevalence of DM distress and depression and their associated factors among people with DM in Jazan, Saudi Arabia. Therefore, this study aims to assess the prevalence of DM-related distress and depression and their associated factors in Saudi people with T2DM in Jazan, Saudi Arabia. It also aims to assess the association between glycemic control and DM-related distress and depression.
Methods
Study Design and Sample Size
Jazan is located in the southwest corner of Saudi Arabia and has a predominantly homogenous population that shares similar ethnic and socioeconomic characteristics. Every patient with T2DM in Jazan is registered in a primary health care (PHC) center. The registry of each PHC center was used as sampling frame. In this study, we applied an analytical, cross-sectional design on Saudi patients with T2DM selected proportionally from PHC centers in Jazan by simple random technique (Figure 1). The sample size was calculated using the Epi Info software program8 with a confidence interval (CI) of 95%, power of 80%, an odds ratio of 2 and Cronbach’s alpha, 0.5. The expected frequency of DM distress and depression was obtained from a previous study conducted in Taif City, Saudi Arabia.9 The computed sample size was 288, but 20% (58 participants) were added to the total calculated sample size to deal with the issue of non-respondents. The study successfully recruited 300 out of the 346 selected participants (response rate was 86.7%). Twelve participants (3.4%) did not meet the inclusion criteria, two of whom had a psychiatric illness. Fourteen (4%) participants did not respond, and 20 (5.8%) refused to participate (Figure 1).
Inclusion and Exclusion Criteria
Saudi patients with T2DM older than 18 were included. Those with a history of any psychiatric illness and who were unwilling to participate were excluded.
 |
Figure 1 Participant enrollment in the current study. |
Data Collection
Face-to-face interviews with the participants were conducted for data collection. The data collected consisted of sociodemographic characteristics, anthropometrics, and laboratory measurements. These included age, sex, marital status, education status, occupation, monthly income, smoking habits, associated DM complications, DM duration, physical activity, body mass index (BMI), and glycated hemoglobin (A1C) levels.
DM-related distress was assessed using a valid questionnaire (the 17-item Diabetes Distress Scale (DDS-17)) that was translated into Arabic and validated (Cronbach’s alpha = 0.87).9 Each item of the DDS-17 has a six-point Likert scale from 1 (indicating no problem) to 6 (indicating a very serious problem). The total DDS-17 score was calculated by summing a patient’s responses to the 17 items and dividing by the number of items on the scale. DM distress was considered clinically significant (moderate distress) if the total score was > 2, and severe if the score was ≥ 3. DDS-17 also assesses other components including emotional-related distress, physician-related distress, regimen-related distress, and interpersonal-related distress. Each component was scored separately by summing its specific item scores and dividing by the number of items on the scale. Patients were considered to have a particular kind of DM-related distress if the score for that specific kind of distress was > 2.
Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9) that was translated into Arabic and validated (Cronbach’s alpha = 0.83).10 Each questionnaire item has a four-point Likert scale 0 (indicating not at all) to 3 (indicating nearly every day). Mild depression was considered to significant if the total score was > 5, moderate if the total score was between 5 and 14, and severe if the total score was > 14.
Following the World Health Organization guidelines,11 BMI was calculated as weight in kilograms divided by the square of the person’s height in meters. BMI was categorized as not obese if the score was < 30 and obese if the score was ≥ 30. T2DM was diagnosed following the American Diabetes Association’s guidelines.12 A1C ≥ 7% was categorized as poor glycemic control, while A1C < 7% was categorized as good glycemic control.13 Physical activity of less than 150 minutes per week was categorized as inadequate physically activity, based on the American Diabetes Association’s guidelines.14
Ethical Consideration
The Jazan Hospital Institutional Review Board (reference number: H-10-Z-068)15 granted ethical approval (No. 1922) for the study, which also complied with the Helsinki Declaration. Written informed consent was obtained from all the participants before enrolment.
Statistical Analysis
Data entry and analysis were performed using Statistical Package for the Social Sciences software.16 The data were coded with anonymous identification numbers in order to guarantee the privacy of the participants. The continuous variables were described by means and standard deviation (SD), and the categorical variables were described by percentages and frequencies. Logistic regression was used to explore the predictors of DM distress and depression in participants with T2DM. An independent t-test was also performed to test for any mean differences between the studied groups. P values < 0.05 were considered statistically significant.
Results
The current study recruited 300 participants with T2DM. The participants’ sociodemographic characteristics and health risks are presented in Table 1. The mean age of the study population was 52.7 years old ± 11.4 (range 23–83 years old), and the mean BMI of the participants was 30.4 ± 5.6, ranging from 17.1–46.5.
 |
Table 1 Sociodemographic Characteristics and Health Habits of the Study Population |
Diabetes Distress and Depression and Associated Factors
The prevalence of DM distress in the study population was 22.3%, with 17.3% (52) having moderate DM distress and 5% (15) having severe distress. Emotional-related DM distress was experienced by 10.7% of the study population, physician-related DM distress was experienced by 11.7%, regimen-related DM distress was experienced by 7%, and interpersonal-related DM distress was experienced by 12.3%. The prevalence of depression in the study population was 20%, with 15.3% (46) having moderate depression and 4.7% (14) having severe depression. The variables marital status, education, occupation, monthly income, and obesity were not significantly associated with DM distress or depression according to a Chi-square test and univariate analysis. Table 2 presents the significant variables associated with DM distress and depression based on multivariate regression analysis. There was also a significant association between DM distress and depression, OR = 3 [95% CI: 1.8, 6.4].
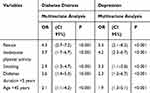 |
Table 2 Significant Predictors of Diabetes Distress and Depression in Regression Analysis |
Diabetes Distress and Depression and A1C
The mean A1C of the study population was 8.9 ± 1.8, ranging from 5.3–14. Of the study participants, 74% had poor glycemic control. An independent t-test was performed to compare the A1C mean between participants with DM distress and depression and those who did not suffer from either. Medication adherence was considered, and the vast majority of participants were adherent to medication regimen (97%). Table 3 shows that the participants with DM distress and depression had higher A1C levels compared to those without DM distress and depression.
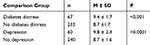 |
Table 3 Independent t-Test Compared Mean Differences for Glycated Hemoglobin (A1C) Levels Between Different Comparison Groups with Type 2 Diabetes |
Discussion
To our knowledge, the current study is the first to measure the prevalence of DM distress and its associated factors among Saudi people with T2DM in Jazan, Saudi Arabia. We focused on T2DM because it is the most common type of DM in Jazan.17 The study showed that approximately one quarter of Saudi patients with T2DM in Jazan suffer from DM-related distress or depression. The prevalence of DM-related distress was estimated to be 22.3%, which is higher than what has been reported in other studies in Australian people (7%),18 German people (8.9%),19 and Indian people (18%).20 The current study results show that the prevalence of depression in T2DM was 20%. This is similar to the prevalence reported in Spain (20%)21 and is higher than the prevalence reported in Canada (12%)22 and Pakistan (14.7%).23 The difference between our population in this study and other populations in other studies might be due to genetic, culture, education factors.
We found that women were more likely to experience DM-related distress and depression. The high prevalence of DM-related distress and depression in females in our study is consistent with the findings of other studies.18,19,21,23 However, some studies have found no association between gender and DM distress or depression.22 Age < 45 and DM duration < 5 years were also significantly associated with DM-related distress and depression in our study. The development of DM at a young age, especially for those recently diagnosed with DM, might affect psychological status.24 The evidence shows that physical activity reduces the risk of developing a psychological disorder, such as depression25 or depression symptoms.26 Our study shows that patients with T2DM who have been physically inactive were more likely to have depression and DM distress, which is consistent with other studies.21 Smoking was also associated with DM distress and depression in our study, which is also in line with other studies.18 The association between smoking and DM distress or depression might be bidirectional, as some people tend to use smoking to relieve symptoms. It has been found that long-term exposure to nicotine dysregulates the hypothalamic-pituitary-adrenal system. This results in changes in the associated monoamine neurotransmitter system, the function of which is to regulate reactions to stressors.27
Susceptibility to DM distress or depression in patients with T2DM is not yet fully understood. It has been found that during psychological stress, the physiology of the neuroendocrine system and of neurotransmitters in the brain (serotonin, dopamine, and norepinephrine) might change and therefore affect mood and behavior.28 It has also been suggested that distress associated with a new T2DM diagnosis might exacerbate depressive symptoms.29
Approximately two thirds of our study population had poor glycemic control. Similar results were found in previous studies conducted in Jazan.30–32 It has been found that DM-related distress18,19,22 and depression18,22 have a negative impact on glycemic control. In psychological conditions such as DM distress and depression, regulatory hormones and neurotransmitters, such as catecholamine, glucocorticoids, growth hormones, and glucagon, are activated.24 Blood glucose levels therefore increase, as these hormones interfere with the action of insulin.33
Limitations
There are several limitations in our study. First, although genetic susceptibility might play a role in DM distress and depression, we did not investigate this. Second, although we used valid subjective methods to assess DM-related distress and depression, clinical objective methods remain the gold standard for diagnosing DM-related distress and depression.
Conclusion
It seems clear that patients with T2DM are susceptible to DM-related distress and depression. In our study, DM-related distress and depression were prevalent in T2DM patients in Jazan, Saudi Arabia. We can therefore conclude that both these conditions need to be screened for and addressed in clinical settings. Establishing the causality of DM-related distress and depression in T2DM is an important aim for any future studies.
Data Sharing Statement
The data are available on request from the corresponding author, Turki Alzughbi.
Acknowledgments
We would like to express our gratitude to the team who helped us in completing this research. To begin with, we would like to thank Jazan Diabetes & Endocrine Center staff, endocrinologists, family and community medicine consultants, and technicians in the registry department for their help. Finally, we would like to thank all participants for their response and cooperation.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This is self-funded research. There was no funding provided for this research.
Disclosure
The authors report no conflict of interests in this work.
References
1. International Diabetes Federation. IDF Diabetes Atlas.
2. UK Prospective Diabetes. Study (UKPDS) Group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837–853. doi:10.1016/S0140-6736(98)07019-6
3. Penckofer S, Ferrans C, Velsor-Friedrich B, Savoy S. The psychological impact of living with diabetes: women’s day-to-day experiences. Diabetes Educ. 2007;33(4):680–690. doi:10.1177/0145721707304079
4. Fisher L, Gonzalez J, Polonsky W. The confusing tale of depression and distress in patients with diabetes: a call for greater clarity and precision. Diabetic Medi. 2014;31:764–772. doi:10.1111/dme.12428
5. Darraj H, Mahfouz M, Al Sanosi R, et al. Psychometric evaluation of the depression literacy questionnaire among adolescents. Psychiatry J. 2016;2016:8045262. doi:10.1155/2016/8045262
6. Perrin N, Davies M, Robertson N, Snoek F, Khunti K. The prevalence of diabetes-specific emotional distress in people with Type 2 diabetes: a systematic review and meta-analysis. Diabet Med. 2017;34(11):1508–1520. doi:10.1111/dme.13448
7. Fisher L, Mullan J, Arean P, Glasgow R, Hessler D, Masharani U. Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care. 2010;33:23–28. doi:10.2337/dc09-1238
8. Dean A, Arner T, Sunki G, et al. Epi Info Program for Public Health Professionals. Atlanta: CDC; 2011.
9. Aljuaid M, Almutairi A, Assiri M, Almalki D, Alswat K. Diabetes-related distress assessment among Type 2 diabetes patients. J Diabetes Res. 2018;2018:7328128. doi:10.1155/2018/7328128
10. Badedi M, Solan Y, Darraj H, et al. Factors associated with long-term control of type 2 diabetes mellitus. J Diabetes Res. 2016;Article ID 2109542:8.
11. World Health Organization (WHO). Physical status: the use and interpretation of anthropometry: report of a WHO Expert committee. Technical report series 854. Geneva: WHO; 1995.
12. American Diabetes Association (ADA). Introduction: standards of medical care in diabetes 2019. Diabetes Care. 2019;42(1):61–66. doi:10.2337/dc19-S006
13. American Diabetes Association (ADA). Introduction: standards of medical care in diabetes 2019. Diabetes Care. 2019;42(1):104.
14. American Diabetes Association (ADA). Introduction: standards of medical care in diabetes 2019. Diabetes Care. 2019;42(1):30.
15. Jazan Hospital IRB. National Committee of Bio Ethics. King Abdulaziz City for Science & Technology (KACST): H-10-Z-068.
16. BM Corp. IBM SPSS Statistics for Windows. NY: IBM Corp; 2012.
17. Bani I. Prevalence, knowledge, attitude and practices of diabetes mellitus among Jazan population, Kingdom of Saudi Arabia (KSA). J Diabetes Mellitus. 2015;5(2):115–122. doi:10.4236/jdm.2015.52014
18. Nanayakkara N, Pease A, Ranasinha S, et al. Depression and diabetes distress in adults with type 2 diabetes: results from the Australian National Diabetes Audit (ANDA). 2018;8:7846.
19. Kuniss N, Kramer G, Müller N, et al. Diabetes-related burden and distress is low in people with diabetes at outpatient tertiary care level. Exp Clin Endocrinol Diabetes. 2016;124(05):307–312. doi:10.1055/s-0042-103685
20. Gahlan D, Rajput R, Gehlawat P, Gupta R. Prevalence and determinants of diabetes distress in patients of diabetes mellitus in a tertiary care centre. Diabetes Metabol Syndr. 2018;12(3):333–336. doi:10.1016/j.dsx.2017.12.024
21. Salinero-Fort M, Gómez-Campelo P, San Andrés-Rebollo F, et al.; MADIABETES Research Group. Prevalence of depression in patients with type 2 diabetes mellitus in Spain (the DIADEMA Study): results from the MADIABETES cohort. BMJ Open. 2018;8:e020768. doi:10.1136/bmjopen-2017-020768
22. Wong E, Afshar R, Qian H, Zhang M, Elliott T, Tang T. Diabetes distress, depression and glycemic control in a canadian-based specialty care setting. Can J Diabetes. 2017;41(4):362–365. doi:10.1016/j.jcjd.2016.11.006
23. Zahid N, Asghar S, Claussen B, Hussain A. Depression and diabetes in a rural community in Pakistan. Diabetes Res Clin Pract. 2008;79(1):124–127. doi:10.1016/j.diabres.2007.07.006
24. Jaser S. Psychological problems in adolescents with diabetes. Adolesc Med State Art Rev. 2010;21(1):138–xi.
25. Mammen G, Faulkner G. Physical activity and the prevention of depression: a systematic review of prospective studies. Am J Prev Med. 2013;45(5):649–657. doi:10.1016/j.amepre.2013.08.001
26. Rosenbaum S, Tiedemann A, Sherrington C, Curtis J, Ward P. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiatry. 2014;75(9):964–974. doi:10.4088/JCP.13r08765
27. Markou A, Kosten TR, Koob GF. Neurobiological similarities in depression and drug dependence: a self-medication hypothesis. Neuropsychopharmacology. 1998;18:135–174. doi:10.1016/S0893-133X(97)00113-9
28. Grisel J, Rasmussen P, Sperry L. Anxiety and depression: physiological and pharmacological considerations. J Individ Psychol. 2006;62(4):398–416.
29. Rotella F, Mannucci E. Diabetes mellitus as a risk factor for depression. A meta-analysis of longitudinal studies. Diabetes Res Clin Pract. 2013;99(2):98–104. doi:10.1016/j.diabres.2012.11.022
30. Darraj H, Badedi M, Poore K, et al. Vitamin D deficiency and glycemic control among patients with type 2 diabetes mellitus in Jazan City, Saudi Arabia. Diabetes Metab Syndr Obes. 2019;12:853–862. doi:10.2147/DMSO.S203700
31. Badedi M, Darraj H, Hummadi A, et al. Vitamin B12 deficiency and foot ulcers in type 2 diabetes mellitus: a case-control study. Diabetes Metab Syndr Obes. 2019;12:2589–2596. doi:10.2147/DMSO.S233683
32. Badedi M, Darraj H, Hummadi A, et al. Khat chewing and Type 2 diabetes mellitus. Diabetes Metab Syndr Obes. 2020;13:307–312. doi:10.2147/DMSO.S240680
33. Lustman P, Clouse R. Depression in diabetic patients: the relationship between mood and glycemic control. J Diabetes Complications. 2005;19(2):113–122. doi:10.1016/j.jdiacomp.2004.01.002
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
