Back to Journals » Clinical Ophthalmology » Volume 14
Cross-Sectional Study on the Coping Strategies Among Glaucoma Patients Attending a Secondary Eye Clinic in Calabar, Nigeria
Authors Eni EN , Edet BE, Ibanga AA , Duke RE
Received 15 December 2019
Accepted for publication 9 April 2020
Published 13 May 2020 Volume 2020:14 Pages 1307—1313
DOI https://doi.org/10.2147/OPTH.S242443
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Egbula Nkanu Eni,1 Bassey Eyo Edet,2 Affiong Andem Ibanga,3 Roseline Ekanem Duke1
1Department of Ophthalmology, University of Calabar Teaching Hospital, Calabar, Nigeria; 2Federal Neuropsychiatric Hospital, Calabar, Nigeria; 3Department of Ophthalmology, University of Calabar, Calabar, Nigeria
Correspondence: Egbula Nkanu Eni
Department of Ophthalmology, University of Calabar Teaching Hospital, Calabar, Nigeria
Tel +234 7035252071
Email [email protected]
Purpose: The major objective of this cross-sectional study was to examine the coping strategies of glaucoma patients at a secondary eye care unit with a view to deciding whether an intervention programme would be justified.
Patients and Methods: The coping styles of 130 consenting adult glaucoma patients aged 18 years and above who were being treated for glaucoma in the Cross River State Eye Care Programme clinic in Calabar, Nigeria, were investigated by means of the 28-item Brief-COPE inventory in this descriptive cross-sectional study.
Results: The mean age of the participants was 54.2 years (± 14.3) while almost three quarters (73.8%) of them were married. About four out of every five persons examined (81.5%) had a minimum of primary education. “Substance (alcohol and other drug) use”, “self-blame” and “behavioural disengagement” are coping styles that were reported by 33%, 42% and 42% of the participants, respectively. This group of patients should be identified in the clinic for appropriate psychological intervention.
Conclusion: The present study confirms previous findings and contributes additional evidence that suggests that coping strategies should be considered in the holistic management of glaucoma patients. The information from the current study can be used to develop targeted interventions aimed at improving the coping styles of glaucoma patients.
Keywords: adults, coping styles, Brief-COPE inventory, Cross River State
Introduction
Glaucoma affects an increasing number of people worldwide and is the leading cause of irreversible blindness and significant visual impairment or low vision.1 Low vision has been noted as one of the most important reasons for poor quality of life, anxiety and poor adaptation.2 Thus, coping with stress seems especially important for adaptation to low vision.3 Several studies have associated poor health-related quality of life with glaucoma,4–11 with resultant adoption of different methods of coping with chronic eye disease.
Coping has been defined as
cognitive and behavioural efforts to manage specific external or internal demands (and conflicts between them) that are appraised as taxing or exceeding the resources of a person.12
The use of some coping strategies such as seeking comfort in religious beliefs and practices may prove beneficial for the person.13 On the other hand, the use of some other coping methods such as “substance use” may be termed “maladaptive” and may result in poorer health outcomes for the patients.
Knowledge of coping styles is important in the care of patients, as these coping methods can be identified and to some extent modified by the attending clinician,13
towards ensuring that the glaucoma patient copes positively with the chronic disease.
At the time of this research, no published study was found in Nigeria where glaucoma is a major cause of visual impairment and blindness,14 or in any other part of Africa to have assessed the coping strategies in patients with glaucoma. Since patient perceptions of disease and methods of coping are heavily influenced by culture and ethnicity,9 it would be difficult to generalise results from studies on coping in other regions. It is therefore important that a study on the coping methods of glaucoma patients be conducted in this part of the world. It is against this background that this study was conducted to examine the coping strategies of glaucoma patients at a secondary eye care facility in Calabar, Nigeria with a view to obtaining evidence-based information that could be used to provide psychosocial support to glaucoma patients in the setting.
Patients and Methods
Study Design and Setting
This descriptive cross-sectional research was conducted among adult glaucoma patients (aged 18 years and above) of the Cross River State Eye Care Programme clinic in Calabar, Nigeria from 1 February 2016 to 21 May 2016. The clinic which is a secondary eye care facility is in Calabar Municipal within Calabar Metropolis, the capital city of Cross River State of Nigeria. Calabar has an area of 406km2 and a population of 371,022 at the 2006 national census.15 The clinic is a high-volume centre that attends to an average of 100 patients a day with a range of 80 to 120 patients. About 8 glaucoma patients are attended to each working day. The participants for this study were drawn from this population of patients.
Ethical Considerations
Ethical clearance was obtained from the Cross River State Health Research Ethics Committee. The ophthalmologist in charge of the Cross River State Eye Care Programme clinic in Calabar also gave approval for conducting the study.
Participant consent was written informed consent, and this study was conducted in accordance with the Declaration of Helsinki.
Sample Size Determination
The sample size was determined based on the primary outcome and calculated using the formula:16

where
n = minimum sample size (when population is >10,000)
z = Standard error of the mean which corresponds to 95% confidence level (1.96)
p = Proportion of coping strategies we anticipated within the sample size which was 0.92 (92%).
q = 1-p
d = Precision with which p is determined which is 5% (0.05)
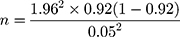
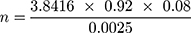


10% of 113 = (10 x 113)/100
= 1130/100
= 11.3
Allowing for 10% attrition, n becomes 113 + 11.3 = 124 (to the nearest whole number).
Thus, the minimum sample size required for the study was 124 as illustrated above.
Study Population
The study population comprised men and women aged 18 years and above who had been diagnosed with glaucoma and had been on some form of treatment for glaucoma prior to the study. Lower age limit of 18 years was chosen because the targeted study populations were adults with glaucoma.
Inclusion criteria
Individuals with the following criteria were included:
- Individuals aged 18 years and above with a diagnosis of glaucoma for a minimum period of 3 months.
- Daily use of topical glaucoma medications for at least 3 months.
- Individuals who gave informed consent.
These criteria helped to ensure that participants had an experience of living with glaucoma and receiving treatment and follow-up care.
Exclusion criteria
Participants with concomitant ocular diseases that could significantly affect vision were excluded from the study.
Sampling Technique
The Cross River State Eye Care Programme clinic in Calabar was purposively selected for the study because it is the only public secondary eye care facility in Calabar that offers comprehensive eye care services to a teeming population of patients. All consecutive patients with glaucoma that attended the clinic during the period of the study who met the inclusion criteria and consented to the study were recruited as they presented to the clinic.4,17 An average of 4 participants were recruited per clinic day twice a week to achieve a total of 130 patients over a period of 4 months.
Instruments and Data Collection
With the help of pretested, semi-structured, self-administered questionnaires, information on sociodemographic characteristics was obtained. Written informed consent was obtained from each participant before data collection. Each participant was then administered the Brief-COPE inventory. The Brief-COPE inventory (available online: http://www.psy.miami.edu/faculty/ccarver/sclBrCOPE.html) developed by Professor Charles Carver at the University of Miami is one of the most commonly used validated coping measures. It is a 28-item questionnaire on 14 different ways of coping (2 questions per type) with the stress of a chronic disease.18 This includes, for instance, “religion” (I have been praying or meditating), “venting” (I have been expressing my negative feelings), and “substance use” (I have been using alcohol or other drugs to make myself feel better).13 Some of the participants that present to the Cross River State Eye Care Programme clinics are not literate, these items were therefore paraphrased into questions so that the questionnaire became interviewer-based. For instance, for “venting”, “Have you been expressing your negative feelings?” The responses to these questions were assessed on a 4-point Likert-type scale with answers ranging from 1 (“I’ve not done this at all”) to 4 (“I’ve been doing this a lot”).13 The questionnaires were administered in Pidgin English without back translation by a trained research assistant.
The scales in The Brief-COPE Inventory were computed as follows (with no reversals of coding):18 Self-distraction (items 1 and 19), active coping (items 2 and 7), denials (items 3 and 8), substance use (items 4 and 11), use of emotional support (items 5 and 15), use of instrumental support (items 10 and 23), behavioural disengagement (items 6 and 16), venting (items 9 and 21), positive reframing (items 12 and 17), planning (items 14 and 25), humour (items 18 and 28), acceptance (items 20 and 24), religion (items 22 and 27) and self-blame (items 13 and 26). There is no such thing as an “overall score” on The Brief-COPE measure. The developer of the scales recommends that each scale should be looked at separately to see what its relation is to other variables.18
As part of screening and service provision, ocular examination including presenting visual acuity was tested in each eye in all participants with an illuminated tumbling E Snellen chart at 6 metres. Anterior segment examination was carried out with a loupe magnification and a pen-torch. The intraocular pressure of each eye was assessed with a Goldmann applanation tonometer attached to a Carl Zeiss slit lamp mounted on a motorized stand. The posterior segment was examined in a dimly lit room, with a direct ophthalmoscope (HEINE BETA200 LED ophthalmoscope, HEINE Optotechnik, Germany) through an undilated pupil and a slit lamp biomicroscopy with a Volk 78 D lens through a dilated pupil. Ocular examination of all the participants as well as documentation of the findings in examination proforma was performed by an ophthalmologist (ENE).
Data Management
The questionnaires were reviewed daily and entered in Statistical Package for the Social Sciences (SPSS) database (Version 20, SPSS Inc., Chicago, IL) for analysis. Descriptive statistics (frequencies and proportions) were used to summarize variables.
Results
A total of 130 participants, from an initial sample of 137 (95% response rate), took part in the study. There were more males than females in the study sample (69/130, 53.1%). The mean age of participants was 54.2 years (±14.3). Most of the study participants were in the age range of 41 to 60 years (64/130, 49.2%) (Table 1). Nearly three quarters of the study population (73.8%) were married while almost 9 out of every 10 persons examined belong to the most popular religion in southern Nigeria: Christianity. Just below a fifth of those surveyed had no formal education (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Study Participants (N=130) |
Frequency of the Coping Mechanisms Adopted by the Study Participants
It can be seen from the data in Table 2 that the commonest coping strategies reported by the respondents were the subscales: “Acceptance” (130/130, 100.0%), “Active coping” (129/130, 99.2%), “Religion” (124/130, 95.4%) and “Venting” (124/130, 95.4%).
 |
Table 2 Frequency of the Coping Methods (Brief-COPE Subscales) Practiced by Study Participants |
Discussion
Glaucoma has a huge impact on the quality of life of patients owing to its chronic nature, associated deterioration of visual function and its lifelong treatment.19 It may affect an individual’s quality of life in various ways: psychological sequelae of diagnosis (e.g. fear of blindness), the visual effects of glaucoma (such as visual field loss), the side-effects of treatment (medical or surgical) and the economic impact from direct and indirect costs.20 The Brief-COPE Inventory was used to assess the coping methods that are commonly adopted by glaucoma patients in an attempt to adapt to the reduced quality of life that is associated with this eye disease.
In this study, nearly half of the participants were in the age group 41 to 60 years. This finding is consistent with the widely held view that glaucoma is commoner among those over 40 years of age.21 The lower number of participants in the age group 61 years and above (compared to the age group 41 to 60 years) (Table 1) can be explained by the report that the life expectancy for Nigerian males is 52.4 years and 53.1 years for females.22 Nearly three quarters of the study population (73.8%) were married and therefore had some form of family support. Family support has been found to have a significant association with good mental health.23 These findings may, therefore, help us to better understand the coping strategies reported by the participants in this study.
Individual’s coping responses to threats and stressors (such as fear of blindness from glaucoma) are key determinants of their psychological adjustment and well-being.24 The commonest coping strategy reported in the current study was acceptance. This was followed by active coping which has been found to be associated with better quality of life and less depression in a recent study.25 Active coping involves taking actions aimed at eliminating the stressor or reorganising its effects.26 In the present study, religion and venting was the third commonest coping strategy, after acceptance and active coping. These findings differ from a previous research in Pakistan which reported religion as the most frequent coping strategy in patients with anxiety and depression.13 The study which utilised the 28-item Brief-COPE inventory that was used in the current study, however, also reported acceptance and active coping as other commonly used coping methods. Even though the Pakistani study was not conducted primarily on glaucoma patients, it can be compared to the present study since glaucoma has been associated with anxiety and depression.27 The overlapping of acceptance and religion in our study may be explained anecdotally that those who are religious are more likely to accept glaucoma as the will of God. This could probably explain why acceptance tops the list of the reported coping strategies. Religion and spirituality offer a source of hope. The belief in an omnipotent God who helps an individual through a difficulty can be mentally beneficial and enhance acceptance.28 A previous study that was conducted in Shanghai, China found religious involvement to be associated with better outcomes in the physical and mental health of the glaucoma patients that were studied.29 Religion plays a predominant role in the lives of many patients and may help them cope with their symptoms.28 These results provide further support for the hypothesis that incorporating a positive aspect of faith into health care may make medical practice more holistic.
The “Denial” scale of the Brief-COPE inventory was reported by some of the study participants as a coping strategy, including those that reported beneficial coping strategies (Table 3). Although in the short-term denial may offer an individual temporary relief from the stress of a “horrible” diagnosis or the fear of blindness, in the long term, denial can lead to deteriorated health outcomes.30 Denial has been associated with worse outcomes for a number of other chronic diseases such as type 1 diabetes31 and acquired immunodeficiency syndrome.32
 |
Table 3 Tallied Score of Beneficial and Maladaptive Coping Strategies |
The least reported coping strategy in the current study was substance (alcohol and other drugs) use, followed by self-blame and behavioural disengagement which are all maladaptive coping styles that were also reported by some participants that reported positive coping methods (Table 3). These findings could be explained by the well-documented report that maladaptive coping strategies such as substance use are under-reported when assessed by self-reporting.33,34 The present findings seem to be consistent with another research which found substance use and behavioural disengagement the least used coping strategies.25 Behavioural disengagement involves giving up attempts aimed at tackling the stressor.26 Maladaptive coping styles may result in poorer health outcomes for the patients.35 A group of researchers in Malaysia who also found substance use and behavioural disengagement to be the least frequently used coping mechanisms reported that higher perceived stress was associated with frequent use of behavioural disengagement coping, lack of religious coping and lack of emotional support coping.26 An implication of this is the need for the attending clinician to identify this group of patients in the clinic through detailed clinical history-taking and institute appropriate psychological intervention (which may involve a psychiatrist) with the aim of modifying or replacing such negative coping strategies with more adaptive ones. Interventions (educational and self-care interventions) to target maladaptive coping strategies such as denial have been effective in other chronic diseases such as acquired immunodeficiency syndrome and chronic kidney disease.36 Thus, to improve the overall quality of life of glaucoma patients, there is a need to empower them with positive coping styles or discourage negative coping strategies. Counselling on positive coping strategies should be incorporated into the routine care of glaucoma patients. Such counselling can be provided by appropriately trained counsellors. This opens the door for consideration of an integrated biopsychosocial approach in the management of chronic illnesses like glaucoma.
Limitations of the Study
This study had a relatively low number of elderly respondents and a preponderance of the participants were married, had tertiary education and a constant source of income. This fact might have biased the results towards more positive coping strategies.
Conclusion
In this exploratory analysis of the coping strategies that glaucoma patients adopt in a secondary eye clinic in Calabar – Nigeria, positive coping strategies such as acceptance and active coping which have been associated with better quality of life and less depression were the most common coping strategies reported. Some glaucoma patients were however found to adopt maladaptive coping strategies such as substance use and self-blame which can lead to deteriorated health outcomes. These findings underline the importance of incorporating coping strategy assessment in the management of glaucoma patients. Furthermore, the findings from this exploratory study can be used to develop targeted multifaceted interventions (such as health education and counselling) aimed at improving the coping strategies of glaucoma patients.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Hommer A. A review of preserved and preservative-free prostaglandin analogues for the treatment of open-angle glaucoma and ocular hypertension. Drugs Today (Barc). 2010;46(6):409–416. doi:10.1358/dot.2010.46.6.1482107
2. Kurna SA, Altun A, Gencaga T, Akkaya S, Sengor T. Vision related quality of life in patients with keratoconus. J Ophthalmol. 2014;2014.
3. Bittner AA, Edwards L, George M. Coping strategies to manage stress related to vision loss and fluctuations in retinitis pigmentosa. Optometry. 2010;81(9):461–468. doi:10.1016/j.optm.2010.03.006
4. Mbadugha C, Onakoya A, Aribaba O, Akinsola F. A comparison of the NEIVFQ25 and GQL-15 questionnaires in Nigerian glaucoma patients. Clin Ophthalmol. 2012;6(1):1411–1419. doi:10.2147/OPTH.S33592
5. Gupta V, Srinivasan G, Mei SS, Gazzard G, Sihota R, Kapoor KS. Utility values among glaucoma patients: an impact on the quality of life. Br J Ophthalmol. 2005;89(10):1241–1244. doi:10.1136/bjo.2005.068858
6. Guedes RA, Guedes VM, Freitas SM, Chaoubah A. Quality of life of medically versus surgically treated glaucoma patients. J Glaucoma. 2013;22(5):369–373. doi:10.1097/IJG.0b013e31824ceb8b
7. Gutierrez P, Wilson MR, Johnson C, et al. Influence of glaucomatous visual field loss in health-related quality of life. Arch Ophthalmol. 1997;115(6):777–784. doi:10.1001/archopht.1997.01100150779014
8. Janz NK, Wren PA, Lichter PR, Musch DC, Gillespie BW, Guire K. Quality of life in newly diagnosed glaucoma patients: the collaborative initial glaucoma treatment study. Ophthalmol. 2001;108(5):887–897. doi:10.1016/S0161-6420(00)00624-2
9. Lee JW, Chan CW, Chan JC, Li Q, Lai JS. The association between clinical parameters and glaucoma-specific quality of life in Chinese primary open angle glaucoma patients. Hong Kong Med J. 2014;20(4).
10. Lester M, Zingirian M. Quality of life in patients with early, moderate and advanced glaucoma. Eye. 2002;16(1):44–49. doi:10.1038/sj.eye.6700036
11. McKean-Cowdin R, Wang Y, Wu J, Azen SP, Varma R. Impact of visual field loss on health-related quality of life in glaucoma: the Los Angeles Latino Eye Study. Ophthalmol. 2008;115(6):941–948. doi:10.1016/j.ophtha.2007.08.037
12. Lazarus RS. Emotion and Adaptation. London: Oxford University Press; 1991.
13. Kasi PM, Naqvi HA, Afghan AK, et al. Coping styles in patients with anxiety and depression. Psychiatry. 2012;2012. doi: 10.5402/2012/461265
14. Federal Ministry of Health, Nigeria. The Nigeria National Blindness and Visual Impairment Survey 2005–2007. Vol. 1. 2007. Available from: http://iceh.lshtm.ac.uk/files/2014/04/NigeriaSurvey.pdf.
15. Ottong JG, Ering SO, Akpan FU. The population situation in Cross River State of Nigeria and its implications for socio-economic development, observation from 1991 and 2006 censuses. J Emerg Trends Educ Res Policy Stud. 2010;1(1):36–42.
16. Charan J, Biswas T. How to calculate sample size for different study designs in medical research. Indian J Psychol Med. 2013;35(2):121–126. doi:10.4103/0253-7176.116232
17. Onokoya AO, Mbadugha CA, Aribaba OT, Ibidapo OO. Quality of life of primary open angle glaucoma patients in Lagos, Nigeria: clinical and sociodemographic correlates. J Glaucoma. 2012;21(5):287–295. doi:10.1097/IJG.0b013e31820d7cfd
18. Carver CS. You want to measure coping but your protocol is too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100. doi:10.1207/s15327558ijbm0401_6
19. Hirneiss C, Vogel M, Kampik A, Neubauer AS, Kent M. Measurement of glaucoma-specific functionality with the GQL-15 and correlation with parameters of visual function. Ophthalmol. 2011;108(10):939–946.
20. Kong XM, Zhu WQ, Hong JX, Sun XH. Is glaucoma comprehension associated with psychological disturbance and vision-related quality of life for patients with glaucoma? A cross-sectional study. BMJ Open. 2014;4(5):1–9. doi:10.1136/bmjopen-2013-004632
21. Bettine P, Matteo FD. Glaucoma: present challenges and future trends. Ophthalmic Res. 2013;50(4):197–208. doi:10.1159/000348736
22. World Bank Group. World Development Indices. 2016.
23. Cheung K, Taillieu T, Turner S, et al. Relationship and community factors related to better mental health following child maltreatment among adolescents. Child Abus Negl. 2017;24(70):377–387. doi:10.1016/j.chiabu.2017.06.026
24. Monzani D, Steca P, Greco A, D’Addario M, Cappelletti E, Pancani L. The situational version of the brief COPE: dimensionality and relationships with goal-related variables. Eur J Psychol. 2015;11(2):295–310. doi:10.5964/ejop.v11i2.935
25. Nipp RD, Greer JA, El-Jawahri A, et al. Coping and prognostic awareness in patients with advanced cancer. J Clin Oncol. 2017;35(22):2551. doi:10.1200/JCO.2016.71.3404
26. Isa SN, Ishak I, Rahman AA, et al. Perceived stress and coping styles among Malay caregivers of children with learning disabilities in Kelantan. Malays J Med Sci. 2017;24(1):81–93. doi:10.21315/mjms2017.24.1.9
27. Gupta V, Dutta P, OV M, Kapoor KS, Sihota R, Kumar G. Effect of glaucoma on the quality of life of young patients. Invest Ophthalmol Vis Sci. 2011;52(11):8433–8437. doi:10.1167/iovs.11-7551
28. Saad M, de Medeiros R. Spiritual-Religious Coping-Health Services Empowering Patients’ Resources. Rijeka: INTECH Open Access. 2012;doi:10.5772/50443
29. Wu P, Guo W, Xia H, Lu H, Xi S. Patients’ experience of living with glaucoma: a phenomenological study. J Adv Nurs. 2011;67(4):800–810. doi:10.1111/j.1365-2648.2010.05541.x
30. Goldbeck R. Denial in physical illness. J Psychosom. 1998;43(6):575–593. doi:10.1016/S0022-3999(97)00168-2
31. Jaser SS, White LE. Coping and resilience in adolescents with type 1 diabetes. Child Care Heal Dev. 2011;37(3):335–342. doi:10.1111/j.1365-2214.2010.01184.x
32. Temoshok LR, Wald RL, Synowski S, Garzino-Demo A. Coping as a multisystem construct associated with pathways mediating HIV-relevant immune function and disease progression. Psychosom Med. 2008;70(5):555–561. doi:10.1097/PSY.0b013e318177354f
33. Harrison ER, Haaga J, Richards T. Self-reported drug use data: what do they reveal? Am J Drug Alcohol Abuse. 1993;19(4):423–441. doi:10.3109/00952999309001632
34. Bone C, Gelberg L, Vahidi M, Leake B, Yacenda-Murphy J, Andersen RM. Under reporting of risky drug use among primary care patients in federal qualified health centres. J Addict Med. 2016;10(6):387–394. doi:10.1097/ADM.0000000000000246
35. Vosvick M, Koopman C, Gore-Felton C, Thoresen C, Krumboltz J, Spiegel D. Relationship of functional quality of life to strategies for coping with the stress of living with HIV/AIDS. Psychosomatics. 2003;44(1):51–58. doi:10.1176/appi.psy.44.1.51
36. Carrico AW, Antoni MH, Duran RE, et al. Reductions in depressed mood and denial coping during cognitive behavioural stress management with HIV-positive gay men treated with HAART. Ann Behav Med. 2006;31(2):155–164. doi:10.1207/s15324796abm3102_7
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
