Back to Journals » Clinical Ophthalmology » Volume 12
Contralateral eye comparison of the phacoemulsification metrics, patient experience and clinical outcomes in patients undergoing bilateral cataract surgery with two commonly used femtosecond laser systems
Authors Khodabakhsh AJ, Hofbauer J
Received 3 February 2018
Accepted for publication 5 April 2018
Published 8 August 2018 Volume 2018:12 Pages 1391—1398
DOI https://doi.org/10.2147/OPTH.S164513
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Afshin James Khodabakhsh, John Hofbauer
Beverly Hills Institute of Ophthalmology, Beverly Hills, CA, USA
Purpose: The purpose of the study was to compare phacometrics, patient experience factors and clinical outcomes in patients undergoing bilateral laser-assisted cataract surgery using two common femtosecond laser platforms.
Setting: This study was conducted in Beverly Hills Institute of Ophthalmology, Beverly Hills, California, USA.
Study design: This was a prospective, comparative, contralateral eye study.
Methods: Femtosecond laser-assisted cataract surgery was performed in the first eye of 50 patients with bilateral cataract (mean age 69.9 ± 8.61 years) using either the Catalys (Johnson & Johnson Vision) or the LenSx (Alcon Laboratories, Inc.) laser system. The fellow eye was treated with the laser not used in the first eye. The primary outcome measures included overall procedural times, and the secondary outcome measures included patient experience with the two laser systems.
Results: There were no statistical differences between the two groups in terms of patient interface preparation time and number of docking attempts as well as effective phaco time, average phaco power, total ultrasound time and nucleus removal time. However, the LenSx group demonstrated a significantly longer cortex removal time and higher perception of pressure and vision loss (p < 0.001) compared to the Catalys group. A significantly higher number of Catalys eyes achieved complete capsulotomy (p < 0.001). The ease of cortex removal was also better in the Catalys group. Postoperative visual acuity, keratometry, endothelial cell count and intraocular pressure were comparable in the two groups.
Conclusion: With similar phacometric and clinical outcomes, both laser platforms were efficient, safe and effective during cataract surgery; however, the Catalys group demonstrated superior outcomes in terms of the patient experience, completeness of capsulotomy and ease of cortex removal.
Keywords: femtosecond laser-assisted cataract surgery, Catalys, liquid optics interface, LenSx, curved contact lens, subconjunctival hemorrhage
Introduction
Cataract has affected over 24.4 million Americans.1 With advancements in technologies and techniques of cataract surgery, patient expectations have steadily increased. This has led to a shift in thinking about cataract surgery, from the correction of pathology and restoration of prior visual status to a refractive procedure that can provide the patient with a better uncorrected vision than previously enjoyed.2
The introduction of femtosecond laser technology has been a significant change in the field of cataract surgery. Femtosecond lasers can focus at a specific depth within the targeted structure and cut the tissue very precisely through a process of photodisruption, enabling incisions to be performed exactly to the desired specifications.3 In addition to corneal incisions, femtosecond laser technology can also perform capsulorrhexis and lens fragmentation. There is substantial evidence that femtosecond laser-assisted cataract surgery (FLACS) yields excellent clinical outcomes in terms of precisely shaped and well-centered anterior capsulorrhexis, better corneal wound construction and lower ultrasound time and energy required for lens fragmentation and liquefaction, thereby resulting in less endothelial cell loss compared to conventional phacoemulsification.4–8
Several femtosecond laser systems for cataract surgery are now commercially available and have demonstrated good results.9 Although these femtosecond laser systems share the same basic principle of photodisruption of corneal tissues, there are differences in imaging, docking and laser characteristics such as pulse duration, pulse frequency and pulse energy.10–12 While the comparison of outcomes after manual cataract surgery and FLACS is well documented,5–7,13 there is a paucity of literature comparing outcomes of cataract surgery with different femtosecond laser platforms. The purpose of this prospective, contralateral eye study was to compare the phacometrics, patient experience factors and clinical outcomes obtained in patients undergoing bilateral FLACS with two commonly used femtosecond laser systems.
Methods
Primary and secondary objectives
This study was conducted primarily to evaluate differences in cataract laser-assisted procedural times and effective phacoemulsification time (EPT) between the Catalys system and the LenSx laser system and secondarily to evaluate patient satisfaction when undergoing cataract surgery.
Patients
This prospective, single-center, randomized, observer-masked, contralateral, comparative study included 100 eyes of 50 patients with bilateral cataract. All subjects were in good general health. Table 1 presents the demographic data of the study subjects. The study protocol was reviewed and approved by an independent institutional review board (IRB), Alpha IRB, San Clemente, CA, USA. At the time of the first visit, written informed consent to participate in the study was obtained from each patient. The study was conducted in compliance with the tenets of the Declaration of Helsinki.
  | Table 1 Demographic data |
The inclusion criteria were age older than 18 years, visual potential of 20/25 or better after cataract removal and intraocular lens (IOL) implantation, preoperative corneal astigmatism of ≤1.5 D in each eye, clear ocular media other than cataract in each eye, normal optical coherence tomography (OCT) of the macula in each eye, naturally dilated mesopic pupil of >3.5 mm in each eye and refractive target of emmetropia in each eye.
The exclusion criteria were known pathology that could affect visual acuity, particularly retinal changes (macular degeneration, cystoid macular edema, proliferative diabetic retinopathy, etc.), amblyopia or strabismus, capsule or zonular abnormalities with preoperative lens tilt and/or decentration, which could affect postoperative centration or tilt of the lens (eg, Marfan syndrome, pseudoexfoliation syndrome), significant irregular astigmatism, history of ocular trauma or prior ocular surgery and uncontrolled glaucoma.
In this contralateral eye study, 50 subjects were randomized to undergo FLACS with either the Catalys system (Johnson & Johnson Vision, Santa Ana, CA, USA) or the LenSx system (Alcon Laboratories, Inc., Fort Worth, TX, USA) in the first eye. The fellow eye was treated 7–28 days later with the laser not used on the first eye.
Two femtosecond laser platforms
The Catalys Precision femtosecond laser platform uses a wavelength of 1,030 nm, pulse duration of 600 femtoseconds, pulse energy of 5–10 μJ and variable pulse repetition rate of 30–120 kHz. Imaging performed by three-dimensional spectral domain OCT (820–920 nm wavelength) and video microscope is used to generate laser treatment plans. The patient interface design is a two-piece, nonapplanating, liquid optics system with vacuum docking.10
The LenSx femtosecond laser platform uses a wavelength of 1,030 nm, pulse duration of 600–800 femtoseconds, maximum pulse energy of 15 μJ and pulse repetition rate of 50 kHz. The imaging system uses three-dimensional spectral domain OCT and video microscope to allow image-guided FLACS. The patient interface design is a one-piece, applanating, curved lens with vacuum docking.10
Preoperative assessment
Preoperatively, all patients underwent comprehensive ophthalmic examination of both eyes, including refraction (sphere and cylinder), keratometry, uncorrected distance acuity (UDVA) and corrected distance acuity (CDVA), slit lamp examination, intraocular pressure (IOP) and fundoscopy. Other evaluations included A-scan, pupil size, corneal thickness, endothelial cell density (ECD) and macular OCT. Preoperative nuclear density was assessed at the slit lamp using the Lens Opacity Classification System III nuclear grading score.
Surgical procedure
All surgeries were performed under topical anesthesia by two experienced surgeons (AJK and JH). Both eyes of a patient were operated by the same surgeon. All patients received the same standardized preoperative, intraoperative and postoperative management for both eyes.
A 4.9–5.0 mm diameter capsulotomy was created, and the lens was fragmented using the randomly assigned femtosecond laser system. In addition, patients presenting with significant amounts of corneal astigmatism (56% [28/50 eyes] in the Catalys laser group and 52% [26/50 eyes] in the LenSx laser group) also underwent femtosecond laser astigmatic keratotomy.
After the laser pretreatment of the crystalline lens, a 2.4 mm incision was created in both groups using a diamond blade. The anterior chamber was filled with a viscoelastic solution, and lens segmentation was undertaken using a phaco chop technique. For all study eyes, the same phacoemulsification machine, Whitestar Signature System with Ellips FX Technology (Johnson & Johnson Vision), was used for the emulsification of nucleus and aspiration of lens cortex. Finally, a foldable IOL was implanted into the capsular bag. The IOLs implanted in the study eyes included monofocal, multifocal and toric IOLs, depending on the patient’s desired visual goals. These included ZCB00 (45 eyes, 45%), ZLB00 (29 eyes, 29%), ZKB00 (14 eyes, 14%), ZMB00 (2 eyes, 2%) and a variety of toric IOLs from several manufacturers (10 eyes, 10%).
Intraoperative measurements
In the femtosecond laser suite, patient interface preparation time (time required to unpack, assemble and dock), the number of docking attempts and suction time (suction ON to suction OFF) were recorded. Patients were asked about their perception of pressure during the laser portion of the procedure (5-point scale: none, trace, mild, moderate, severe) and experience of transient vision loss during the laser pass (yes or no). The surgeon also recorded the completeness of the capsulotomy (yes or no) and incidence of subconjunctival hemorrhage (5-point scale: none, trace, mild, moderate, severe). Additional metrics were recorded during the phacoemulsification portion of the procedure in the operating room, including the presence of a capsule tags, total ultrasound time, average phacoemulsification power, EPT (determined by phacoemulsification time multiplied by average phacoemulsification power), cortex removal time, nucleus removal time and ease of cortex removal (4-point scale: very easy, easy, difficult, very difficult). Immediately after the laser procedure, patients were asked about their perception of pressure (5-point scale: none, trace, mild, moderate, severe) and experience of transient vision loss during the laser pass (yes or no).
Postoperative measurements
Postoperatively, all patients were evaluated at day 1, day 7 and 30–60 days after surgery. At day 1 postoperatively, UDVA and slit lamp examination of the anterior chamber, ECD and IOP were evaluated. The examination variables evaluated at 1 week postoperatively included UDVA, CDVA, slit lamp examination, manifest refraction, keratometry, ECD and IOP. The last postoperative visit, at 1 month, was a detailed ophthalmic examination similar to the preoperative protocol.
Statistical analyses
Data analysis was performed using JMP 10 software (SAS Institute Inc., Cary, NC, USA). For comparisons between preoperative and postoperative data within groups as well as for the comparison between femtosecond laser platforms, the Student’s t-test for paired data was used. In addition, categorical variables were compared using the chi-square test. For all statistical tests, a p-value of <0.05 was considered to be statistically significant.
Results
Laser outcomes and patient experience
The results of laser system measurements for both laser systems are shown in Table 2. No statistically significant difference was observed for patient interface preparation time and number of docking attempts between the two laser systems. However, the Catalys group had a significantly longer suction time compared to the LenSx group (p < 0.001).
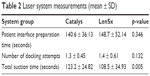  | Table 2 Laser system measurements (mean ± SD) |
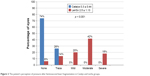
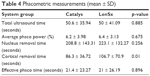
The LenSx laser group had a significantly greater incidence of subconjunctival hemorrhage (p < 0.001), with 78% of eyes having mild-to-severe subconjunctival hemorrhage compared to 2% of eyes with mild subconjunctival hemorrhage in the Catalys laser group (Figure 1). While undergoing the Catalys procedure, 74% of subjects felt no pressure and 26% of subjects felt only trace pressure. While undergoing the LenSx procedure, 80% of subjects felt some pressure, varying from mild to severe (p < 0.001; Figure 2). No subjects experienced transient vision loss during the Catalys laser treatment, while 22 subjects (44%) experienced transient vision loss during the LenSx procedure (p < 0.001; Figure 3).
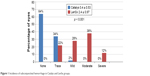  | Figure 1 Incidence of subconjunctival hemorrhage in Catalys and LenSx groups. |
  | Figure 2 The patient’s perception of pressure after femtosecond laser fragmentation in Catalys and LenSx groups. |
  | Figure 3 Patient’s experience with vision loss after femtosecond laser fragmentation in Catalys and LenSx groups. |
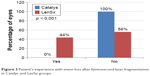
All eyes in the Catalys group achieved complete capsulotomy compared to 92% of eyes in the LenSx group (p < 0.001; Figure 4).
  | Figure 4 Completeness of capsulotomy in Catalys and LenSx groups. |
Phacometric measurements
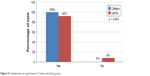
The distribution of lens opacity grades was significantly different between the two femtosecond laser groups, with 44% of eyes in the Catalys group categorized as grade 3 or 4 compared to 32% of eyes in the LenSx group (p = 0.005; Table 3).
  | Table 3 Cataract density |
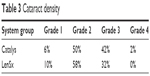
Most of the phacoemulsification parameters, including total ultrasound time, average phacoemulsification power, nucleus removal time and EPT, were comparable in both the laser groups. However, cortex removal time was significantly faster in the Catalys group (p = 0.01) (Table 4). Correspondingly, ease of cortex removal was rated better with the Catalys laser (Figure 5).
  | Table 4 Phacometric measurements (mean ± SD) |
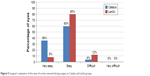  | Figure 5 Surgeon’s evaluation of the ease of cortex removal during surgery in Catalys and LenSx groups. |
Clinical outcomes
At baseline, axial length, pupil size, corneal thickness, ECD and IOP were similar in both laser groups. There was no statistically significant difference between the two groups in preoperative manifest refraction spherical equivalent (MRSE), UDVA or CDVA.
Postoperatively, both the Catalys and LenSx laser groups showed improvements in UDVA and CDVA compared to baseline; however, there was no statistical difference between the two laser groups. Similar findings were observed for MRSE and keratometric outcomes. The mean ECD and IOP values at the last postoperative visit were similar to the preoperative measures, with no statistically significant differences between the two groups (Table 5).
Complications
There was one case with anterior capsular tags in the LenSx group and none in the Catalys group. There were no posterior capsular tears in either group. Postoperatively, lid edema, conjunctival hyperemia, conjunctival and corneal edema and anterior chamber cells and flare were observed in both the groups. The incidence of complications was not significantly different between the two laser groups.
Discussion
Both lasers performed well, facilitating the cataract procedure for the surgeons and delivering excellent clinical results for our patients.
While most of the intraoperative laser system parameters and phacometric parameters were found to be comparable for both laser groups in this study, there were some important differences, primarily in the patient experience. The mean suction time in the LenSx laser group was significantly lower than that in the Catalys group (108.5 vs 123.2 seconds, respectively), which was expected due to the differences in the optical interface design of the two laser systems and has been similarly reported in the literature.14,15
Immediately after the laser procedure, all patients were asked to evaluate their perception of pressure and vision loss during the laser procedure. While the patients in the Catalys group either did not perceive any pressure or perceived only trace pressure, ~60% of patients felt moderate to severe pressure during the LenSx procedure (p < 0.001; Figure 2). Likewise, a transient loss of vision as the patient’s vision was obscured during the laser pass was noted by more than four of 10 subjects after the LenSx procedure and not at all during the Catalys procedure (p < 0.001; Figure 3), despite the fact that suction duration was longer in the Catalys laser group. This finding is similar to the one reported by Rivera et al,14 who observed that suction time may not be an important factor in the sensation of high pressure and vision loss experienced by the patients during FLACS.
Subconjunctival hemorrhage may occur as a result of the docking process and strong suction force applied at the patient interface and is more commonly observed with contact corneal applanation interface systems.16 Correspondingly, in the current study, the incidence of subconjunctival hemorrhage was significantly higher in the LenSx group. The differences in docking systems between the two laser systems could also influence the completeness of capsulotomy; in the current study, complete capsulotomies were observed in 100% of eyes in the Catalys group compared to 92% of eyes in the LenSx group (Figure 4). A recent experimental study compared two optical interface designs, curved contact lens (CCL) and liquid optics interface (LOI), for FLACS. It was found that femtosecond laser using CCL interface produced significant corneal folds resulting in incomplete capsulotomy; however, complete capsulotomy was observed in all cases with the LOI system.16 A layer of transparent fluid between the cornea and the optical window reduces the area of direct contact with the eye; as a result, an LOI design may reduce eye deformations, corneal folds, globe instability and subconjunctival hemorrhage compared to a CCL interface.16 The differences in the optical interface designs most likely account for the significant differences observed in terms of patient experience, completeness of capsulotomy and incidence of subconjunctival hemorrhage between the two laser groups.
The phacoemulsification parameters between the two groups were also found to be comparable in terms of total ultrasound time, average phacoemulsification power, nucleus removal time and EPT. However, the Catalys eyes had denser nuclei, which are typically associated with longer phaco time and more phaco energy. Future studies in which researchers control for cataract grade would be helpful.
A significantly lower cortex removal time was recorded in the Catalys group than in the LenSx group in this study. Rivera et al,14 in contrast, reported comparable values, which could potentially be explained by the differences in the phacoemulsification machines between the two studies. Correspondingly, the ease of cortex removal was also better in the Catalys group (96% very easy to easy vs 88% in the LenSx group; Figure 5). Since, ultrasonic phacoemulsification was performed using the same phacoemulsification machine in both the groups, some technical differences in laser characteristics such as pulse energy, pulse frequency and repetition rate may be responsible for these results.
Several studies have reported that femtosecond laser treatment may significantly reduce the phacoemulsification time and energy, thus alleviating corneal endothelial cell loss and corneal edema in the early postoperative period.4,8 Consistent with previous findings of FLACSs,14 we recorded no significant differences in endothelial cell count between the two laser groups at different time points in this study. Furthermore, the complication rate was found to be comparable between the two laser systems. These findings would suggest that both the femtosecond lasers used in the current study were similarly safe.
This study evaluated and compared the outcomes of two different femtosecond laser platforms with the most up-to-date software features. Laser, phacometric and safety parameters were largely comparable, demonstrating that both systems are effective tools for the refractive cataract surgeon. The LOI system of the Catalys laser platform (vs the CCL of the LenSx) was apparently instrumental in the significantly lower perception of pressure and vision loss, lesser incidence of postlaser subconjunctival hemorrhage and more complete capsulotomies. Given the high expectations of patients undergoing premium surgical procedures, patient experience factors such as these may affect the overall perception of the procedure, surgeon and surgery center and are worth considering and measuring in future studies.
Acknowledgments
Raman Bedi, MD (IrisARC – Analytics, Research & Consulting, Chandigarh, India) and Jan Beiting (Wordsmith Consulting, Cary, NC, USA) provided research and editorial assistance in the preparation of this manuscript. The authors received research funding from Abbott Medical Optics (AMO), now part of Johnson & Johnson Vision.
Disclosure
AJK serves as a consultant to AMO/Johnson & Johnson Vision. The authors report no other conflicts of interest in this work.
References
National Eye Institute [webpage on the Internet]. Cataracts. Available from: https://www.nei.nih.gov/eyedata/cataract. Accessed August 9, 2017. | ||
Kanellopoulos AJ, Asimellis G. Standard manual capsulorhexis/ultrasound phacoemulsification compared to femtosecond laser-assisted capsulorhexis and lens fragmentation in clear cornea small incision cataract surgery. Eye Vis (Lond). 2016;3:20. | ||
Abouzeid H, Ferrini W. Femtosecond-laser assisted cataract surgery: a review. Acta Ophthalmol. 2014;92:597–603. | ||
Abell RG, Kerr NM, Vote BJ. Toward zero effective phacoemulsification time using femtosecond laser pretreatment. Ophthalmology. 2013;120(5):942–948. | ||
Conrad-Hengerer I, Hengerer FH, Schultz T, Dick HB. Effect of femtosecond laser fragmentation on effective phacoemulsification time in cataract surgery. J Refract Surg. 2012;28(12):879–883. | ||
Nagy ZZ, Kránitz K, Takacs AI, Miháltz K, Kovács I, Knorz MC. Comparison of intraocular lens decentration parameters after femtosecond and manual capsulotomies. J Refract Surg. 2011;27(8):564–569. | ||
Palanker DV, Blumenkranz MS, Andersen D, et al. Femtosecond laser-assisted cataract surgery with integrated optical coherence tomography. Sci Transl Med. 2010;2(58):58ra85. | ||
Takács AI, Kovács I, Miháltz K, Filkorn T, Knorz MC, Nagy ZZ. Central corneal volume and endothelial cell count following femtosecond laser-assisted refractive cataract surgery compared to conventional phacoemulsification. J Refract Surg. 2012;28(6):387–391. | ||
Roberts TV, Lawless M, Chan CC, et al. Femtosecond laser cataract surgery: technology and clinical practice. Clin Exp Ophthalmol. 2013;41(2):180–186. | ||
Donaldson KE, Braga-Mele R, Cabot F, et al. Femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2013;39(11):1753–1763. | ||
Grewal DS, Schultz T, Basti S, Dick HB. Femtosecond laser-assisted cataract surgery – current status and future directions. Surv Ophthalmol. 2016;61(2):103–131. | ||
Wu BM, Williams GP, Tan A, Mehta JS. A comparison of different operating systems for femtosecond lasers in cataract surgery. J Ophthalmol. 2015;2015:616478. | ||
Abell RG, Darian-Smith E, Kan JB, Allen PL, Ewe SY, Vote BJ. Femtosecond laser-assisted cataract surgery versus standard phacoemulsification cataract surgery: outcomes and safety in more than 4000 cases at a single center. J Cataract Refract Surg. 2015;41(1):47–52. | ||
Rivera RP, Hoopes PC Jr, Linn SH, Hoopes PC. Comparative analysis of the performance of two different platforms for femtosecond laser-assisted cataract surgery. Clin Ophthalmol. 2016;10:2069–2078. | ||
Yeoh R. Practical differences between 3 femtosecond phaco laser platforms. J Cataract Refract Surg. 2014;40(3):510. | ||
Talamo JH, Gooding P, Angeley D, et al. Optical patient interface in femtosecond laser-assisted cataract surgery: contact corneal applanation versus liquid immersion. J Cataract Refract Surg. 2013;39(4):501–510. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

