Back to Journals » Clinical Ophthalmology » Volume 12
Comparative study of induced changes in effective lens position and refraction after Nd:YAG laser capsulotomy according to intraocular lens design
Authors Monteiro T, Soares A , Dourado Leite R , Franqueira N, Faria-Correia F, Vaz F
Received 10 November 2017
Accepted for publication 22 December 2017
Published 19 March 2018 Volume 2018:12 Pages 533—537
DOI https://doi.org/10.2147/OPTH.S156703
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Tiago Monteiro,1,2 Andreia Soares,1 Ricardo Dourado Leite,1 Nuno Franqueira,1 Fernando Faria-Correia,1,2 Fernando Vaz1
1Department of Ophthalmology, Hospital de Braga, Braga, Portugal; 2Life and Health Sciences Research Institute (ICVS), School of Health Sciences, University of Minho, Braga, Portugal
Purpose: To evaluate and compare the changes in refraction and effective intraocular lens (IOL) position between a plate-haptic IOL and a c-loop single-piece IOL after neodymium-doped yttrium aluminium garnet (YAG) laser posterior capsulotomy.
Methods: In a prospective study, anterior chamber depth and subjective refraction were measured in 110 pseudophakic eyes from 110 patients, before and 1 month after YAG laser capsulotomy. Patients were divided into 2 groups according to the IOL design: group 1 (plate-haptic acrylic hydrophilic AT LISA tri 839MP®) and group 2 (c-loop acrylic hydrophobic single-piece AcrySof® SA60AT). Lens position was obtained through optical coherence biometry (Biograph WaveLight OB820®).
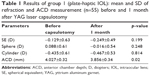
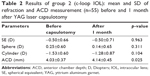
Results: YAG laser capsulotomy was performed 37.8±9.8 months after surgery in group 1 and 40.6±8.6 months in group 2 (p=0.125). Significant changes were found in the lens effective position after treatment in the 2 groups. The YAG posterior capsulotomy led to a change of anterior chamber depth in group 1 from 4.03±0.32 mm to 3.86±0.34 mm (p=0.02) and in group 2 from 4.03±0.37 mm to 4.14±0.45 mm (p=0.025). After YAG laser posterior capsulotomy, no significant changes were observed in mean spherical equivalent, sphere or cylinder for both groups (p>0.05).
Conclusion: YAG laser posterior capsulotomy can induce a significant change in the IOL position according to the IOL type; however, the refractive change after treatment is clinically insignificant.
Keywords: intraocular lens, YAG capsulotomy, refraction, effective lens position, multifocal IOL
Introduction
Posterior capsular opacification (PCO) is a common complication of cataract surgery; the overall incidence of PCO has been demonstrated to depend on the surgical technique, the intraocular lens (IOL) material, and the IOL design.1–5 The standard treatment is neodymium-doped yttrium aluminum garnet (Nd:YAG) laser posterior capsulotomy; the complications associated include elevated intraocular pressure, IOL damage, uveitis, cystoid macular edema, vitreous and retinal detachments as well as refractive changes due to possible axial IOL displacement. The morphologic and tensile changes in the capsular bag after treatment may cause a longitudinal movement of the IOL, and, consequently, a refractive change, leading to decreased uncorrected visual acuity. This last aspect is particularly crucial after multifocal IOL implantation and should be considered before other treatments are indicated, especially laser ablative surgical enhancements.
Previous studies6–13 have addressed the change in IOL position and clinical refraction after YAG treatment. However, only 1 study found a significant change in axial IOL position; none of the studies available found differences on subjective or automatic refraction. Findl et al13 described that IOL style and size of capsulotomy are determinant factors in lens movement; the authors demonstrated that a larger capsulotomy size is associated with increased posterior displacement of the IOL and a hyperopic shift, which is more pronounced with plate-haptic IOLs. However, all other studies available only evaluate one type of IOL, and some of them were performed after extracapsular cataract extraction or using old-fashioned IOLs (3-piece foldable IOLs, single-piece polymethyl methacrylate [PMMA] or silicone IOLs), not taking into consideration the modern trends in phacoemulsification surgery.
This study aims to evaluate and compare the differences in subjective refraction and effective lens position after Nd:YAG laser posterior capsulotomy between a plate-haptic foldable IOL and a single-piece c-loop IOL.
Methods
Study design
This prospective single-center study included patients with PCO submitted to Nd:YAG laser posterior capsulotomy at the Ophthalmology Department of Hospital de Braga, Portugal. The tenets of the Declaration of Helsinki were followed, and full ethical approval from the Ethical Commission of Hospital de Braga was obtained. After receiving a full explanation of the nature and possible consequences of the study and treatment, all patients provided a written informed consent.
Inclusion criteria were patients with visually significant PCO, previous cataract surgery by standard phacoemulsification, IOL implantation in the capsular bag, no intraoperative complications, and anterior capsulotomy fully covering the lens in the capsular bag. We excluded patients with intraoperative complications, pseudoexfoliation syndrome, any preoperative evidence of zonulopathy or intraoperative implantation of capsular tension ring, and poor mydriasis.
Patients were divided into 2 groups. Group 1 included patients with a single-piece plate haptic IOL (AT LISA tri 839MP®; Carl Zeiss, Meditec, Germany) implantation and group 2 patients with a single-piece c-loop IOL (AcrySof® SA60AT; Alcon Laboratories, Inc., Fort Worth, TX, USA). Both groups were treated with Nd:YAG laser (Ellex Super Q) capsulotomy, with 4.5 mm diameter (1.2 mJ/spot). After the procedure, inflammation was controlled with 0.3 mg/mL Bromofenac eye drops, 2 times daily for 15 days.
The AT LISA tri 839MP (Carl Zeiss) is a diffractive trifocal preloaded IOL with a 6.0 mm biconvex optic, an overall length of 11.0 mm, and a posterior surface with asphericity of 0.18. It has a plate-haptic design with 4-point fixation, with an angulation of 0 degrees. The IOL optic has a 360-degree square edge to prevent PCO, with no interruption at the optic–haptic junction and an anti-PCO barrier ring around the optic. The IOL is made of foldable hydrophilic acrylate with a water content of 25% and has a hydrophobic surface and a refractive index of 1.46.
The AcrySof SA60AT (Alcon Laboratories) is a foldable single-piece open-loop IOL, with anterior asymmetric biconvex optic design, made of acrylic hydrophobic polymer with modified L-shaped haptics. The IOL has a 6.0 mm optic and 13.0 mm overall diameter. The IOL optic has a 360-degree square edge design.
Before and 1 month after YAG capsulotomy, a complete ophthalmological examination was performed, which included the measurement of visual acuity, subjective refraction, and the anterior chamber depth (ACD) value. The ACD value was obtained through optical coherence biometry (Biograph WaveLight OB820®; Alcon Laboratories), taking the average of 5 measurements and manually adjusting the position of the anterior surface of the IOL detected by the device. Subjective refraction included spherical equivalent (SE), sphere, cylinder, and axis, and was performed by the same ophthalmologist for all patients. The SE values were calculated as the sum of the sphere and half of the cylindrical power.
Statistical analysis was performed with SPSS (SPPS Inc, Chicago, IL, USA). All data were reported as mean and SDs. Data normality was calculated with Kolgomorov–Smirnov test; for parametric data, a paired t-test was used to compare the values of refraction and ACD; for data not normally distributed, the Wilcoxon signed-rank test was used. A value of p<0.05 was considered statistically significant.
Results
One hundred and ten pseudophakic eyes of 110 patients were enrolled in this study. Fifty-five eyes underwent a single-piece plate-haptic IOL (AT LISA tri 839MP; Carl Zeiss) implantation (group 1) and 55 eyes a single-piece c-loop IOL (AcrySof SA60AT; Alcon Laboratories) implantation (group 2). None of the patients presented surgical complications, previous ocular surgeries or previous ocular pathology. The mean ages of groups 1 and 2 were 65.7±6.08 and 68.3±11 years, respectively (p=0.235). Capsulotomy was performed 37.8±9.8 months after surgery in group 1 and 40.6±8.6 months after surgery in group 2 (p=0.125).
Tables 1 and 2 provide the results obtained from the data of subjective refraction (SE, sphere, cylinder, and axis) and axial IOL position before and after capsulotomy for both groups. In group 1 (Table 1), we observed a significant anterior movement of the IOL (from 4.027±0.32 mm to 3.856±0.34 mm; p=0.02, paired t-test) and in group 2 (Table 2) we observed a backward movement of the implant (from 4.03±0.37 to 4.14±0.45 mm; p=0.025, paired t-test). No significant refractive change was observed in SE, sphere, or cylinder for any group (p>0.05). Group 1 SE changed from −0.13±0.63 D to −0.25±0.49 D and group 2 SE from −0.50±0.66 D to −0.50±0.71 D.
Discussion
Our study is the first to demonstrate that the IOL design can have an impact on IOL stability in the capsular bag after YAG laser capsulotomy. We were able to show that Nd:YAG capsulotomy induced a significant change in the axial position of the IOL inside the capsular bag and that the axial IOL movement differs according to the IOL design. A haptic plate IOL has the tendency to move anteriorly after YAG capsulotomy, while a C-loop lens shows a significant posterior movement. Both changes, however, induced a minor refractive change that was not statistically or clinically relevant in our patient’s cohort.
Thornval et al14 were the first to describe the changes in IOL position after YAG capsulotomy. The authors showed no difference in axial position and SE after the treatment, but the measurements were taken with an optical pachymeter (50.0 μm resolution), different types of IOLs were used, and the study group also included patients after extracapsular cataract extraction. Findl et al13 were the first to report a significant backward movement of IOLs after YAG capsulotomy. In all eyes studied, the authors observed a significant backward movement of all the 3 types of IOLs studied (1-piece PMMA IOL, 3-piece foldable IOL, and a plate-haptic IOL), and the change was more pronounced with plate-haptic IOLs. The authors also found a hyperopic shift that was not clinically relevant, based on the small amplitude of the lens movement. In our study group, we observed a different IOL movement according to the IOL type; the plate-haptic IOLs moved anteriorly and the single-piece c-loop IOLs moved posteriorly. We consider that the major factor responsible for this aspect observed in our results is the lens design; the plate-haptic IOL has a tendency to move in the opposite direction of a c-loop IOL. The tension exerted by the haptics of the IOL on the capsular bag is higher for a plate-haptic IOL, since there are 4 points of contact between the IOL and the capsular bag and less compressibility of the haptics, and they are a part of the main body of the lens. As for the c-loop IOL design, there are 2 points of contact between the IOL and the capsular bag and higher compressibility of the haptics in case of compression by the capsular bag, since they are open and separate from the optical body of the lens. This difference found in our study in comparison with Findl’s study could be explained by the different timing of evaluation after treatment (immediately after the capsulotomy was performed in Findl’s study and 1 month after treatment in our study) and possibly by the different design of both plate-haptic IOLs. As in our study, Vrijman et al8 concluded that capsulotomy in patients with multifocal pseudophakia did not result in a significant change in refraction. The majority of patients (93%) showed a small change of SE <0.50 D, always a myopic change. The study did not measure the position of the IOL before and after treatment, and only included single-piece foldable IOL patients. Khambhiphant et al6 also observed a nonsignificant myopic change in a cohort of 47 pseudophakic patients; the authors found no difference in the axial displacement or SE before and after 3 months between a single-piece and a three-piece IOL. Other similar studies, from Hu et al12 and Ozkurt et al,9 did not observe a significant change in refraction or IOL axial position after YAG capsulotomy; however, these were not comparative studies and only one type of IOL was evaluated.
Despite the fact that we observed a significant change in axial position of the IOL after YAG capsulotomy, there was no difference observed in SE, sphere, and cylinder. This important aspect of our study was observed in both the plate-haptic IOL group and the single-piece c-loop IOL. This finding is significant, because any significant refractive change in a patient with a multifocal IOL implant can have a major impact on the uncorrected distance and uncorrected near visual acuity. Even though we did not find any refractive change, there was a tendency for a small myopic shift in group 1 (SE from −0.13±0.63 D to −0.25±0.49 D), which is explained by the anterior movement observed with this type of IOL design. In group 2, the SE remained unchanged, even though there was a small but significant posterior movement of the implant, which could result in a slight hyperopic shift. The majority of other studies6,8–14 also reported that the change in SE after Nd:YAG laser capsulotomy was statistically insignificant.
This study, however, has some limitations. The results were based on a short-time follow-up period, and we did not measure the capsulotomy size area accurately. Many studies have shown that a large capsulotomy size is associated with an increased posterior movement of IOL. It has also been described that a hyperopic shift may be caused by a large capsulotomy size.13,15 Holladay et al16 concluded that optimal capsulotomy should be equal to or exceed the diameter of the pupil in the scotopic conditions and remain within the border of IOL. Another aspect that was not taken into consideration was the white–white diameter in each group of patients, as it can be a factor that influences the movement of the IOL, and also the fact that the ACD measurements after YAG laser capsulotomy were all performed on an undilated pupil. Even though most recent studies have shown that the pupil diameter does not have a clinically significant impact on IOL calculation and biometric measurements, it could have a statistically significant impact on the ACD measurement after IOL implantation, since all the studies published report their results based on phakic patients.
In conclusion, our data show that Nd:YAG capsulotomy promotes significant changes of the axial position of an IOL inside the capsular bag, inducing significant anterior movement of a plate-type lens and posterior displacement of c-loop lens. This movement was not associated with a significant refractive change in both the plate-haptic and the single-piece c-loop IOLs.
Disclosure
The authors report no conflicts of interest in this work.
References
Johansson B. Glistenings, anterior/posterior capsular opacification and incidence of Nd:YAG laser treatments with two aspheric hydrophobic acrylic intraocular lenses – a long-term intra-individual study. Acta Ophthalmol. 2017;95(7):671–677. | ||
Haripriya A, Chang DF, Vijayakumar B, et al. Long-term posterior capsule opacification reduction with square-edge polymethylmethacrylate intraocular lens: randomized controlled study. Ophthalmology. 2017;124(3):295–302. | ||
Chang A, Kugelberg M. Posterior capsule opacification 9 years after phacoemulsification with a hydrophobic and a hydrophilic intraocular lens. Eur J Ophthalmol. 2017;27(2):164–168. | ||
Kalauz M, Masnec S, Kordic R, et al. Posterior capsule opacification and Nd:YAG rates with two acrylic intraocular lenses after age-related cataract treatment: three-year results. Semin Ophthalmol. 2016:1–7. | ||
Heatley CJ, Spalton DJ, Kumar A, Jose R, Boyce J, Bender LE. Comparison of posterior capsule opacification rates between hydrophilic and hydrophobic single-piece acrylic intraocular lenses. J Cataract Refract Surg. 2005;31(4):718–724. | ||
Khambhiphant B, Liumsirijarern C, Saehout P. The effect of Nd:YAG laser treatment of posterior capsule opacification on anterior chamber depth and refraction in pseudophakic eyes. Clin Ophthalmol. 2015;9:557–561. | ||
Karahan E, Tuncer I, Zengin MO. The effect of ND:YAG laser posterior capsulotomy size on refraction, intraocular pressure, and macular thickness. J Ophthalmol. 2014;2014:846385. | ||
Vrijman V, van der Linden JW, Nieuwendaal CP, van der Meulen IJ, Mourits MP, Lapid-Gortzak R. Effect of Nd:YAG laser capsulotomy on refraction in multifocal apodized diffractive pseudophakia. J Refract Surg. 2012;28(8):545–550. | ||
Ozkurt YB, Sengor T, Evciman T, Haboglu M. Refraction, intraocular pressure and anterior chamber depth changes after Nd:YAG laser treatment for posterior capsular opacification in pseudophakic eyes. Clin Exp Optom. 2009;92(5):412–415. | ||
Levy J, Lifshitz T, Klemperer I, et al. The effect of Nd:YAG laser posterior capsulotomy on ocular wave front aberrations. Can J Ophthalmol. 2009;44(5):529–533. | ||
Chua CN, Gibson A, Kazakos DC. Refractive changes following Nd:YAG capsulotomy. Eye (Lond). 2001;15(Pt 3):304–305. | ||
Hu CY, Woung LC, Wang MC, Jian JH. Influence of laser posterior capsulotomy on anterior chamber depth, refraction, and intraocular pressure. J Cataract Refract Surg. 2000;26(8):1183–1189. | ||
Findl O, Drexler W, Menapace R, et al. Changes in intraocular lens position after neodymium:YAG capsulotomy. J Cataract Refract Surg. 1999;25(5):659–662. | ||
Thornval P, Naeser K. Refraction and anterior chamber depth before and after neodymium- YAG laser treatment for posterior capsule opacification in pseudophakic eyes: a prospective study. J Cataract Refract Surg. 1995;21(4):457–460. | ||
Yilmaz S, Ozdil MA, Bozkir N, Maden A. The effect of Nd:YAG laser capsulotomy size on refraction and visual acuity. J Refract Surg. 2006;22(7):719–721. | ||
Holladay JT, Bishop JE, Lewis JW. The optimal size of a posterior capsulotomy. J Am Intraocul Implant Soc. 1985;11(1):18–20. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.