Back to Journals » Clinical Interventions in Aging » Volume 14
Clinical performance of a bone-anchored annular closure device in older adults
Authors Bouma GJ , Ardeshiri A, Miller LE , Van de Kelft E, Bostelmann R , Klassen PD, Flüh C , Kuršumović A
Received 9 March 2019
Accepted for publication 14 May 2019
Published 19 June 2019 Volume 2019:14 Pages 1085—1094
DOI https://doi.org/10.2147/CIA.S208098
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Gerrit J Bouma,1 Ardeshir Ardeshiri,2 Larry E Miller,3 Erik Van de Kelft,4,5 Richard Bostelmann,6 Peter D Klassen,7 Charlotte Flüh,8 Adisa Kuršumović9
1Department of Neurosurgery, OLVG and Amsterdam University Medical Centers, Amsterdam, the Netherlands; 2Section for Spine Surgery, Klinikum Itzehoe, Itzehoe, Germany; 3Miller Scientific Consulting, Asheville, NC, USA; 4Department of Neurosurgery, AZ Nikolaas, Sint-Niklaas, Belgium; 5Antwerp University, Antwerp, Belgium; 6Department of Neurosurgery, University Clinic Düsseldorf, Duesseldorf, Germany; 7Department of Neurosurgery, St. Bonifatius Hospital, Lingen, Germany; 8Department of Neurosurgery, University Medical Center Schleswig-Holstein, Kiel, Germany; 9Department of Neurosurgery, Donauisar Klinikum Deggendorf, Deggendorf, Germany
Background: Lumbar discectomy is a common surgical procedure in middle-aged adults. However, outcomes of lumbar discectomy among older adults are unclear.
Methods: Lumbar discectomy patients with an annular defect ≥6 mm width were randomized to receive additional implantation with a bone-anchored annular closure device (ACD, n=272) or no additional implantation (controls, n=278). Over 3 years follow-up, main outcomes were symptomatic reherniation, reoperation, and the percentage of patients who achieved the minimum clinically important difference (MCID) without a reoperation for leg pain, Oswestry Disability Index (ODI), SF-36 Physical Component Summary (PCS) score, and SF-36 Mental Component Summary (MCS) score. Results were compared between older (≥60 years) and younger (<60 years) patients. We additionally analyzed data from two postmarket ACD registries to determine consistency of outcomes between the randomized trial and postmarket, real-world results.
Results: Among all patients, older patients suffered from crippling or bed-bound preoperative disability more frequently than younger patients (57.9% vs 39.1%, p=0.03). Among controls, female sex, higher preoperative ODI, and current smoking status, but not age, were associated with greater risk of reherniation and reoperation. Compared to controls, the ACD group had lower risk of symptomatic reherniation (HR=0.45, p<0.001) and reoperation (HR=0.54, p=0.008), with risk reductions comparable in older vs younger patients. The percentage of patients achieving the MCID without a reoperation was higher in the ACD group for leg pain (81% vs 72%, p=0.04), ODI (82% vs 73%, p=0.03), PCS (85% vs 75%, p=0.01), and MCS (59% vs 46%, p=0.007), and this benefit was comparable in older versus younger patients. Comparable benefits in older patients were observed in the postmarket ACD registries.
Conclusion: Outcomes with lumbar discectomy and additional bone-anchored ACD are superior to lumbar discectomy alone. Older patients derived similar benefits with additional bone-anchored ACD implantation as younger patients.
Keywords: annulus fibrosus, disc, elderly, herniation, lumbar, sciatica
Introduction
The intervertebral discs are cartilaginous joints connecting the vertebral bodies that function by transmitting loads through the spinal column and imparting normal mobility. Each intervertebral disc is comprised of an internal gelatinous nucleus pulposus, the surrounding collagen-rich annulus fibrosus, and the cartilage endplates connecting the disc to the adjacent vertebral bodies. Increases in the internal pressure of the intervertebral disc convey stretch forces to the annulus. If these forces exceed the capacity of the annulus to withstand them, the annulus may tear, disc material may exit through the defect and enter the spinal canal, and nerve root compression with local inflammation may ensue. Herniation of a lumbar intervertebral disc is a common incidental radiographic finding in adults,1 with the prevalence increasing from 29% at age 20 to 43% at age 80.2 Imaging evidence of lumbar disc herniation requires no specific treatment unless the patient experiences associated sciatica or neurological deficits that are resistant to conservative therapy.
Approximately 1–5% of the general population experience sciatica each year, most commonly due to lumbar disc herniation.3 While most sciatica episodes eventually resolve with or without treatment, approximately 20% of affected individuals suffer from debilitating symptoms that are refractory to conservative management.4,5 In these patients, accumulating evidence suggests that lumbar discectomy offers faster and more durable pain relief compared to continued nonsurgical management.6,7 A meta-analysis of comparative studies with at least 1-year follow-up concluded that surgery offered greater reductions in leg pain compared to nonsurgical treatments.8 The most common surgical technique for treatment of symptomatic lumbar disc herniation is lumbar discectomy.9
Contemporary lumbar discectomy surgery involves a limited approach in which extradiscal nuclear material is excised to decompress the adjacent nerve root with little to no removal of disc material within the intervertebral space.10 Compared to aggressive discectomy techniques, limited lumbar discectomy preserves disc height and lowers the risk of future lumbar degenerative changes at the expense of a higher reherniation risk.15 Following removal of the offending disc material, the defect in the annulus fibrosus is typically left unrepaired. Since the annulus fibrosus has limited capacity for healing,11 the residual annular defect serves as a constant potential pathway by which remaining disc material may reherniate, resulting in symptom recurrence. Small (<6 mm width) annular defects do not confer an elevated risk of reherniation, but patients with large defects (≥6 mm width) comprise a high-risk subset with a 2- to 3-fold increase in reherniation risk.12 Thus, patients with large annular defects are appropriate candidates for additional intraoperative treatments intended to reduce the risk of reherniation.
Numerous studies have reported clinically important reductions in reherniation and reoperation rates in patients treated with lumbar discectomy and additional implantation with a bone-anchored annular closure device (ACD) compared to patients treated with lumbar discectomy alone.13,14 The ACD (Barricaid, Intrinsic Therapeutics, Woburn, MA, USA) is comprised of an occlusion component to physically block the annular defect and a titanium anchor to secure the occlusion component to an adjacent vertebral body. Based on safety and efficacy data derived from preclinical and clinical studies, the ACD received marketing approval by the US Food and Drug Administration in February 2019. Because most patients in clinical studies of the ACD were middle aged, it remains unclear whether the favorable outcomes demonstrated with the ACD are generalizable to older patients. Investigation of sciatica treatments in older adults is an important pursuit since affected individuals suffer from disability levels comparable to those with a history of chronic obstructive pulmonary disease, stroke, or myocardial infarction.22 Thus, the purpose of this study was to compare the efficacy of lumbar discectomy with or without a bone-anchored ACD among older (≥60 years) versus younger (<60 years) patients with large postsurgical annular defects.
Methods
Study design
The primary findings of this report were derived from 3-year results of a randomized trial conducted at 21 sites involving patients with a large annular defect at completion of a lumbar discectomy procedure who received additional implantation with an ACD (276 patients) or no additional interoperative treatment (278 patients). A total of 19 patients in each group were older adults (≥60 years). Given the relatively small number of older adults treated with the ACD in this randomized trial, we supplemented this report with data from two large postmarket ACD registries.
Randomized trial
This multicenter randomized trial was approved by local ethics committees (listed in Table S1), and all participants provided written informed consent. The trial was prospectively registered at ClinicalTrials.gov (NCT01283438). Eligible adults aged 21–75 years presented with radicular symptoms that were refractory to at least 6 weeks of conservative management. Preoperative imaging tests included magnetic resonance imaging (MRI) of the lumbar spine, low-dose computed tomography (CT) at the level of herniation, and flexion/extension x-rays. The correlation of imaging-confirmed lumbar disc herniation with clinical symptoms was determined by a positive straight leg test or femoral stretch test. Minimum symptom severity thresholds were 40/100 for leg pain severity on a visual analogue scale (VAS) and 40/100 for back dysfunction on the Oswestry Disability Index (ODI). Patients with lumbar spine osteoporosis, significant spondylolisthesis, previous surgery at the level of herniation, active infection, or spinal tumor were not eligible for the trial. Patients who met initial eligibility criteria were scheduled for lumbar discectomy during which a final eligibility criterion was evaluated.
All patients were treated with limited lumbar discectomy in which extradiscal nuclear material was excised to relieve nerve root compression, but no attempts were made to remove significant amounts of intradiscal material.10 After the discectomy procedure was completed, the final eligibility assessment was performed. The size of the surgically induced defect in the annulus fibrosus was measured with a specialized tool. In patients with small annular defects, discectomy was concluded and patients were discontinued from the study owing to their low risk of future reherniation.12 Patients with large annular defects measuring at least 6 mm in width were intraoperatively randomized (1:1) to receive additional implantation with an ACD or to receive no additional treatment (controls).
In patients assigned to the ACD group, a bone-anchored ACD was implanted as a stand-alone procedure following the lumbar discectomy. A sizing trial was performed under fluoroscopic control to establish the correct access trajectory and placement of the device. Next, the ACD was implanted under fluoroscopic guidance by placing the occlusion component in the annular defect to prevent future expulsion of disc material into the extradiscal space. After fluoroscopic confirmation of correct device placement, the surgical site was inspected and standard wound closure was performed. Perioperative care was at the discretion of each hospital.
Patients returned for follow-up visits at 6 weeks, 3 months, 6 months, and annually for 3 years. Physical and neurological examinations, as well as lateral and anteroposterior x-rays, were performed at each visit; MRI, CT, and flexion/extension x-rays were performed annually. Patients presenting with symptoms indicative of reherniation received imaging at the time of presentation to confirm the diagnosis. Reoperations at the level of the original herniation were recorded throughout follow-up. Key patient-reported outcomes included leg pain severity, ODI, SF-36 Physical Component Summary (PCS) score, and SF-36 Mental Component Summary (MCS) score.
Preoperative patient characteristics were reported using the mean and standard deviation (SD) or the count and percentage. The minimum clinically important difference (MCID) was defined as a ≥20-point decrease from baseline for leg pain,16 a ≥15-point decrease from baseline for ODI,17 a ≥5.7-point increase from baseline for PCS,18 and a ≥6.3-point increase from baseline for MCS.18 Severe disability in follow-up was defined by an ODI score >40/100.17 Cox proportional hazard models were developed to determine the association of baseline patient characteristics with the risk of symptomatic reherniation and reoperation following lumbar discectomy. Statistical analyses were performed using Stata v14.2 (StataCorp).
Postmarket ACD registries
Due to the limited number of older adults enrolled in the randomized trial, supplementary data were provided by two postmarket ACD registries, with study oversight separately provided by study authors (AA and AK). Each registry was approved by an ethics committee (Klinikum Itzehoe, Itzehoe, Germany; Donauisar Klinikum Deggendorf, Deggendorf, Germany), and all participants provided written informed consent. Complete eligibility criteria, methodology, and main study results from each of these registries were previously published,19–21 but the influence of patient age on ACD performance was not reported. Patients in each registry were treated with limited lumbar discectomy and received additional bone-anchored ACD implantation following verification of a large annular defect. Patient eligibility requirements were generally comparable to the randomized trial, but fewer criteria were applied since these were postapproval registries of patients treated in real-world conditions. Key outcomes in the registries were symptomatic reherniation, reoperation, leg pain severity, and ODI over a minimum of 2 years follow-up.
Results
Randomized trial
Patient status
Among 554 randomized patients, 276 were treated with lumbar discectomy and additional ACD implantation, while 278 were treated with lumbar discectomy only. A total of 550 patients (272 ACD, 278 controls) with 3-year theoretical follow-up were included in this analysis; ACD implantation was not attempted in 4 patients because of the proximity of the nerve root to the intended device implantation location. There were 19 older patients (≥60 years) in each treatment group (6.9% of patients). Ultimately, 75% of patients returned for the 3-year follow-up visit.
Preoperative data
When pooling preoperative data from both treatment groups, older patients had a lower frequency of smoking and herniated more frequently at lumbar levels versus at L5/S1 relative to younger patients. Older patients reported greater back-related disability than their younger counterparts and tended to present with more severe leg pain (Table 1).
 | Table 1 Preoperative characteristics of older versus younger patients treated with lumbar discectomya |
Predictors of reherniation and reoperation with lumbar discectomy
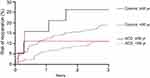
Among control patients treated with lumbar discectomy alone, higher ODI score, female sex, lower PCS score, and greater leg pain were associated with higher risk for symptomatic reherniation in univariate analysis, with only female sex (HR =1.72, p=0.02) and higher ODI (HR=1.22 per 10-point increase, p=0.01) remaining in the multivariate model. Univariate predictors of reoperation were female sex, lower PCS score, greater leg pain, and current smoking status, with only female sex (HR =2.81, p<0.001) and current smoking (HR=1.31, p=0.004) remaining in the multivariate model. Age was not associated with the risk of symptomatic reherniation (p=0.68) or reoperation (p=0.66) (Table 2 and Figure 1).
 | Table 2 Predictors of symptomatic reherniation and reoperation risk over 3 years after lumbar discectomy |
 | Figure 1 Rates of symptomatic (Symp) reherniation and reoperation over 3 years after lumbar discectomy by age group. |
Effect of additional bone-anchored ACD implantation
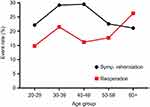
Compared to lumbar discectomy alone, the clinical benefit of additional bone-anchored ACD implantation was comparable in older and younger patients. Over 3 years of follow-up, the risk of symptomatic reherniation was 12.5% with ACD versus 21.1% in controls in older patients and 14.8% versus 30.2% in younger patients. The corresponding HRs were 0.63 in older patients (indicating a 37% relative risk reduction with ACD) and 0.44 in younger patients (indicating a 56% relative risk reduction with ACD) (Figure 2). The benefit of bone-anchored ACD in preventing reoperation was also comparable between older and younger age groups. The risk of reoperation was 11.1% with ACD versus 26.3% in controls in older patients and 11.0% versus 18.8% in younger patients. The corresponding HRs were 0.41 in older patients (indicating a 59% relative risk reduction with ACD) and 0.55 in younger patients (indicating a 45% relative risk reduction with ACD) (Figure 3).
The percentage of patients who achieved the MCID while remaining free from a reoperation favored the ACD group for all patient-reported outcomes in older and younger patients. Among older patients comparing ACD to controls, success rates were 83.3% vs 70.6% for leg pain, 84.6% vs 70.6% for ODI, 83.3% vs 68.8% for PCS, and 53.8% vs 41.2% for MCS. Among younger patients, success rates were 80.4% vs 72.0% for leg pain, 81.9% vs 73.0% for ODI, 84.9% vs 75.1% for PCS, and 59.8% vs 46.5% for MCS (Figure 4). Comparing the ACD group to controls, the percentage of patients at 3 years who were free from reoperation and severe disability was 84.6% vs 58.8% in older patients and 81.4% vs 72.5% in younger patients.
Postmarket ACD registry outcomes
A total of 268 patients from 2 postmarket registries were treated with lumbar discectomy and additional bone-anchored ACD implantation. Mean patient age was 46±14 years, with 46 (17.2%) older patients at least 60 years of age and 222 (82.8%) younger patients under 60 years of age. Mean preoperative leg pain severity was 78±21 and ODI was 51±20. Comparing older vs younger patients treated with the ACD, symptomatic reherniation rates were 3.2% vs 14.9% and reoperation rates were 0% vs 8.2%. The percentage of older vs younger patients who achieved the MCID without a reoperation at 2 years minimum follow-up was 80.0% vs 69.9% for leg pain and 92.7% vs 72.3% for ODI (Table 3).
 | Table 3 Results of annular closure device postmarket registries by age group |
Discussion
We examined for the first time the influence of patient age on surgical outcomes among patients with large annular defects following lumbar discectomy. With the benefit of approximately 1,500 patient-years of follow-up from a randomized trial and over 500 patient-years of follow-up from postmarket registries, we identified several important clinical findings. First, older patients with large postsurgical annular defects had a high risk of symptomatic reherniation and reoperation that was comparable to younger patients. Second, additional implantation of a bone-anchored ACD resulted in significant reductions in reherniation and reoperation risk, regardless of age. Finally, leg pain, disability, and quality of life greatly improved with lumbar disc surgery regardless of age, were durably maintained during follow-up, and favored patients treated with the ACD. Overall, these results highlight the clinical utility and patient-centric benefit of the additional use of a bone-anchored ACD in older, as well as younger, adults with large annular defects following lumbar disc surgery.
Sciatica secondary to lumbar disc herniation most often affects adults in their 40s and, therefore, the clinical impact of sciatica in older adults is likely underappreciated. Contrary to popular belief, sciatica is quite common among the elderly, affecting more than 20% of adults aged 65 and older.22 The negative impact of sciatica on quality of life in older adults is tremendous. The results of the current study suggest that older adults suffer from severe symptoms prior to discectomy surgery, and with a greater magnitude compared to their younger counterparts, a finding that has been confirmed by others.23 The preoperative disability associated with sciatica in the elderly is so incapacitating that affected individuals report a quality of life that is comparable to those with a history of COPD, stroke, or myocardial infarction.22 Thus, effective treatments for sciatica in the elderly should be identified since there is a paucity of clinical guidance specific to this underrepresented population.24,25
We also observed that among patients with large postsurgical annular defects following lumbar discectomy, age was not associated with reherniation rates. This was a unique finding since it is commonly reported in the general discectomy literature that reherniation rates decline by 4% with every additional year of age,26 which is hypothesized to relate to the increasing disc degeneration that accompanies aging which protects against reherniation.27 It has also been suggested that older individuals undergoing surgery for lumbar disc herniation have inferior patient-reported outcomes compared to younger patients.23 However, in patients with large annular defects, it appears that reherniation risk remains at an increased level and is fairly stable during the lifespan. A possible explanation for this finding is that the influence of a large annular defect on the subsequent risk of reherniation may be much greater than the influence of patient age. Support for this hypothesis comes from the study of Kim et al.28 that reported a strong association of reherniation risk with large annular defects but no association with patient age. This implies that lumbar discectomy does not necessarily confer lower reherniation rates in older adults and that additional procedures may be warranted in high-risk patients with large defects in the annulus fibrosus.
Additional implantation of an ACD resulted in significant reductions in the risk of reherniation and reoperation, regardless of age. Comparing older to younger patients treated with an ACD, older patients derived similar or superior benefits across all study outcomes. Thus, age alone should not be a contraindication for lumbar surgery or for ACD implantation, provided the patient is fit for surgery. However, as a group, older patients suffering from sciatica tend to face more unique challenges that warrant additional consideration such as a higher risk of spinal osteoporosis, concomitant comorbidities that may influence surgical risk, and challenges in differential diagnosis owing to coexisting lumbar degenerative changes such as spinal stenosis.25,29 Independent of age, these surgical considerations should be weighed against the potential for symptom relief and associated quality-of-life benefits. Results of the current study, for the first time, demonstrate that lumbar discectomy with ACD implantation reliably and significantly reduces the risk of reherniation and reoperation and improves patient symptoms and quality of life, in older and younger patients alike.
Strengths of the randomized trial include results derived from 1,500 patient-years of follow-up and recruitment of the largest known sample of older adults with large postsurgical annular defects. The randomized, multicentric nature of the trial further improves generalizability of conclusions while minimizing bias. Additionally, we report here the largest known series of older adults treated with an ACD, the results of which were derived from a randomized trial and two real-world postmarket registries. There are also limitations of this study, which are mainly related to patient selection. First relates to annular defect size. It has been estimated that large annular defects are observed following approximately 30% of discectomy procedures.12 Patients with smaller defects may not benefit from ACD implantation since their reherniation risk is inherently lower. Thus, the results presented here are generalizable only to patients deemed to be a high risk for reherniation based on the size of the postsurgical defect. A second limitation relates to the sample size of the subgroups included in this analysis. While this study included the largest known sample of older patients with large annular defects, the sample size of 19 older ACD patients and 19 older controls has low power to detect clinically meaningful group differences and, therefore, age group comparisons were descriptive in nature. In order to overcome this limitation, we supplemented the results of the randomized trial with additional data derived from two large postmarket registries with the ACD. Results of these registries corroborated those from the randomized trial, which improves confidence in the overall conclusions of this study. Still, lack of a control group in the registries is an acknowledged limitation. Third, diseases that negatively impact bone quality (eg, lumbar osteoporosis or malignancy) or increase surgical complexity (eg, significant spondylolisthesis) preferentially impact the elderly. While such conditions are not absolute contraindications to lumbar disc surgery, they were exclusion criteria in the randomized trial reported here and, therefore, the performance of the ACD in the presence of these conditions is unclear. Finally, continued patient observation is warranted to determine whether the reported outcomes are maintained in long-term follow-up.
Conclusion
Outcomes with lumbar discectomy and additional bone-anchored ACD are superior to lumbar discectomy alone. Older patients derived similar benefits with additional bone-anchored ACD implantation as younger patients.
Abbreviation list
ACD, annular closure device; MCID, minimal clinically important difference; MCS, Mental Component Summary; ODI, Oswestry Disability Index; PCS, Physical Component Summary.
Data sharing statement
All authors have agreed to the submission and publication of this manuscript. The authors confirm that requests for data underlying the findings described in this manuscript may be made to the corresponding author starting 1 year following publication of this article.
Acknowledgment
There were no contributors to the article other than the authors. No writing assistance regarding this study was received.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Dr Ardeshiri, Dr Miller, Dr Klassen, and Dr Kuršumović disclose consultancy with Intrinsic Therapeutics. Dr Ardeshiri reports personal fees and non-financial support from Intrinsic Therapeutics outside the submitted work. Dr Miller reports personal fees from Intrinsic Therapeutics during the conduct of the study. Dr Klassen reports personal fees from Intrinsic Therapeutics and non-financial support from Intrinsic Therapeutics during the conduct of the study. Dr Kuršumović reports personal fees from Intrinsic Therapeutics during the conduct of the study. The authors report no other conflicts on interest in this work.
References
1. Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69–73. doi:10.1056/NEJM199407143310201
2. Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36:811–816. doi:10.3174/ajnr.A4173
3. Frymoyer JW. Back pain and sciatica. N Engl J Med. 1988;318:291–300. doi:10.1056/NEJM198802043180506
4. Vroomen PC, de Krom MC, Knottnerus JA. Predicting the outcome of sciatica at short-term follow-up. Br J Gen Pract. 2002;52:119–123.
5. Vroomen PC, de Krom MC, Wilmink JT, Kester ADM, Knottnerus JA. Lack of effectiveness of bed rest for sciatica. N Engl J Med. 1999;340:418–423. doi:10.1056/NEJM199902113400602
6. Peul WC, van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356:2245–2256. doi:10.1056/NEJMoa064039
7. Kreiner DS, Hwang SW, Easa JE, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014;14:180–191. doi:10.1016/j.spinee.2013.08.003
8. Arts MP, Kursumovic A, Miller LE, et al. Comparison of treatments for lumbar disc herniation: systematic review with network meta-analysis. Medicine (Baltimore). 2019;98:e14410. doi:10.1097/MD.0000000000014410
9. Gray DT, Deyo RA, Kreuter W, et al. Population-based trends in volumes and rates of ambulatory lumbar spine surgery. Spine (Phila Pa 1976). 2006;31:1957–1963. discussion 1964. doi:10.1097/01.brs.0000229148.63418.c1
10. Spengler DM. Lumbar discectomy. Results with limited disc excision and selective foraminotomy. Spine (Phila Pa 1976). 1982;7:604–607.
11. Bron JL, Helder MN, Meisel HJ, et al. Repair, regenerative and supportive therapies of the annulus fibrosus: achievements and challenges. Eur Spine J. 2009;18:301–313. doi:10.1007/s00586-008-0856-x
12. Miller LE, McGirt MJ, Garfin SR, Bono CM. Association of annular defect width after lumbar discectomy with risk of symptom recurrence and reoperation: systematic review and meta-analysis of comparative studies. Spine (Phila Pa 1976). 2018;43:E308–E315. doi:10.1097/BRS.0000000000002501
13. Thome C, Klassen PD, Bouma GJ, et al. Annular closure in lumbar microdiscectomy for prevention of reherniation: a randomized clinical trial. Spine J. 2018;18:2278–2287. doi:10.1016/j.spinee.2018.05.003
14. Choy WJ, Phan K, Diwan AD, Ong CS, Mobbs RJ. Annular closure device for disc herniation: meta-analysis of clinical outcome and complications. BMC Musculoskelet Disord. 2018;19:290. doi:10.1186/s12891-018-2213-5
15. Watters WC
16. Ostelo RW, de Vet HC. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol. 2005;19:593–607. doi:10.1016/j.berh.2005.03.003
17. Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25:2940–2952. discussion 2952.
18. Ware JE
19. Kursumovic A, Rath S. Performance of an annular closure device in a ‘real-world’, heterogeneous, at-risk, lumbar discectomy population. Cureus. 2017;9:e1824.
20. Kursumovic A, Rath SA. Effectiveness of an annular closure device in a “real-world” population: stratification of registry data using screening criteria from a randomized controlled trial. Med Devices (Auckl). 2018;11:193–200. doi:10.2147/MDER.S167381
21. Ardeshiri A, Miller LE, Synowitz M, et al. Surgical experience and complications in 50 patients treated with an anular closure device following lumbar discectomy. Orthopaedic Surgery. In press 2019.
22. Jia H, Lubetkin EI, Barile JP, et al. Quality-adjusted life years (QALY) for 15 chronic conditions and combinations of conditions among US adults aged 65 and older. Med Care. 2018;56:740–746. doi:10.1097/MLR.0000000000000943
23. Stromqvist F, Stromqvist B, Jonsson B, et al. The outcome of lumbar disc herniation surgery is worse in old adults than in young adults. Acta Orthop. 2016;87:516–521. doi:10.1080/17453674.2016.1205173
24. Cloyd JM, Acosta FL
25. Ferreira ML, McLachlan A. The challenges of treating sciatica pain in older adults. Drugs Aging. 2016;33:779–785. doi:10.1007/s40266-016-0404-z
26. Abdu RW, Abdu WA, Pearson AM, Zhao W, Lurie JD, Weinstein JN. Reoperation for recurrent intervertebral disc herniation in the spine patient outcomes research trial: analysis of rate, risk factors, and outcome. Spine (Phila Pa 1976). 2017;42:1106–1114. doi:10.1097/BRS.0000000000002088
27. Wilke HJ, Ressel L, Heuer F, Graf N, Rath S. Can prevention of a reherniation be investigated? Establishment of a herniation model and experiments with an anular closure device. Spine (Phila Pa 1976). 2013;38:E587–E593. doi:10.1097/BRS.0b013e31828ca4bc
28. Kim KT, Lee DH, Cho DC, Sung J-K, Kim Y-B. Preoperative risk factors for recurrent lumbar disk herniation in L5-S1. J Spinal Disord Tech. 2015;28:E571–E577. doi:10.1097/BSD.0000000000000041
29. Rainville J, Lopez E. Comparison of radicular symptoms caused by lumbar disc herniation and lumbar spinal stenosis in the elderly. Spine (Phila Pa 1976). 2013;38:1282–1287. doi:10.1097/BRS.0b013e31828f463e
Supplementary material
 | Table S1 List of participating centers and patient enrollment totals |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.