Back to Journals » Clinical Ophthalmology » Volume 14
Both Subjective Emotional Distress and Visual Handicap Correlate with Belin ABCD Classification in the Worse Eye as Measured with the “Keratoconus End-Points Assessment Questionnaire” (KEPAQ)
Authors Balparda K , Herrera-Chalarca T, Silva-Quintero LA , Torres-Soto SA , Segura-Muñoz L , Vanegas-Ramirez CM
Received 8 May 2020
Accepted for publication 10 June 2020
Published 30 June 2020 Volume 2020:14 Pages 1839—1845
DOI https://doi.org/10.2147/OPTH.S261785
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Kepa Balparda,1,2 Tatiana Herrera-Chalarca,3 Laura Andrea Silva-Quintero,4 Sneider Alexander Torres-Soto,4 Laura Segura-Muñoz,5 Claudia Marcela Vanegas-Ramirez6
1Department of Cornea and Refractive Surgery, Black Mammoth Surgical, Medellín, Colombia; 2Predoctoral Research Group, Universidad de Valladolid, Valladolid, Spain; 3Department of Clinical Research, Black Mammoth Surgical, Medellín, Colombia; 4Medicarte, Medellín, Colombia; 5School of Medicine, Universidad Pontificia Bolivariana, Medellín, Colombia; 6Department of Ophthalmology, Universidad Pontificia Bolivariana, Medellín, Colombia
Correspondence: Kepa Balparda Email [email protected]
Background: Keratoconus is a disease characterized by progressive corneal distortion and quality of vision. So far, no study using disease-specific scales has evaluated whether different stages of the disease correlate with higher quality of life (QoL) compromise.
Methods: A total of 114 patients with a confirmed diagnosis of Keratoconus were included in this retrospective study. All patients underwent a clinical and a Pentacam evaluation. They were also administered the “Keratoconus End-Points Assessment Questionnaire” (KEPAQ). Belin ABCD criteria were used for Keratoconus classification. “Better eye” was defined as the eye with the lowest maximum keratometry value. Spearman Rank Order Correlation was used to determine the correlation between the different Belin criteria and the KEPAQ scores in both subscales.
Results: Mean age was 28.13 ± 11.57 years, with 39.47% of patients being male. Mean score for the KEPAQ-E was 2.33 ± 3.40 Logit, while for the KEPAQ-F, it was 1.85 ± 3.61 Logit. Criteria A (anterior elevation), B (posterior elevation) and D (visual acuity) in the worse eye correlated significantly with a greater decrease in QoL (p < 0.05 for all correlations). No correlation could be found regarding the better eye.
Conclusion: A greater corneal distortion in the worse eye, as determined by Belin ABCD, is associated with a greater decrease in patient’s QoL. Surgical improvement of the worse eye should probably be performed before surgery of the better eye, as it may provide a better response regarding the quality of life improvement.
Keywords: Keratoconus, quality of life, vision ocular
Introduction
Keratoconus is the most common primary corneal ectasia worldwide. It is characterized by a progressive distortion of the corneal anatomy, associated with a significant decrease in visual quality. Although so far there is a considerable number of surgeries and optical aids aimed at improving the visual quality of patients with Keratoconus, subjects with the disease tend to show significant alterations in their ability to perform their daily tasks normally.
At present, Patient Reported Outcome Measurements (PROM) have gained great significance,1 as an effective and simple mechanism to collect information on the burden of disease from a patient’s point of view.2 This kind of instruments allows for a reliable determination of how much subjective alteration patients feel about their quality of life (QoL), according to the disease they suffer. This approach is especially important considering that visual alteration is a highly subjective experience, and that visual disturbance referred by the patient is not necessarily associated with the anatomical alteration or with other elements directly measurable by the physician.
To date, no paper studying whether corneal distortion correlated with Keratoconus QoL as measured by a disease-specific PROM. All studies have used general PROMs which render “inadequate”3 results in Keratoconus patients.
This paper studies whether corneal distortion as measured with the Belin ABCD classification correlates with QoL scores as measured with the Keratoconus End-Points Assessment Questionnaire (KEPAQ), a previously validated disease-specific scale.4 This is important not only because it will demonstrate construct validity for the scale but also because it will give good insight as to how different stages of the disease cause greater affections in visual and emotional distress from the patient’s point of view.
Methods
This is a retrospective analytical study, using Rasch Methodology and correlation analysis, seeking to determine whether KEPAQ scores in both subscales correlate in any way with corneal anatomical parameters, including Belin ABCD classification. It included patients with a prior diagnosis of Keratoconus based on an altered corneal curvature (especially posterior one), coupled with corneal protrusion and thickness reduction, associated with a decrease in visual acuity.
Ethical Aspects
This research adhered to the tenets of the Helsinki’s declaration and proper ethical approval was obtained at the “Comité de Ética en Investigación” from Clínica de Oftalmología Sandiego (Ref. Num. Keratoconus – 01). According to Colombian law, being a retrospective study, no written informed consent was necessary and was not advised by the ethical committee. All patient data accessed complied with relevant data protection and privacy regulations.
Sample Size and Study Population
As the main objective of this study included a correlation between KEPAQ scores and Belin ABCD Keratoconus classification, a sample size was calculated accordingly. University of California San Francisco’s sample size calculator for correlation (available at http://www.sample-size.net/correlation-sample-size) was used to calculate the minimum sample size for the requirements of the investigation. A two-tailed alpha value of 0.05 and a ß value of 0.20 were determined to be adequate. As there are no prior studies regarding the correlation of Keratoconus-specific questionnaires with corneal values, an arbitrary expected correlation value of r = 0.26 was considered to be clinically important. With these values, a sample size of 114 patients was determined to be required.
Study population was comprised of patients with a confirmed diagnosis of Keratoconus in at least one of their eyes.
Belin ABCD Classification
Belin ABCD Classification has been recently described as a better way of classifying anatomic y functional compromise in Keratoconus. It is comprised of a total of four criteria which evaluate different aspects of the cornea and vision. A stands for Anterior Elevation (elevation in the anterior wall of the cornea), while B stands for Back Elevation (elevation in the posterior wall of the cornea). C stands for Corneal Thickness while D stands for Distance Visual Acuity. All criteria but D are taken directly from the Pentacam.
Pentacam software version was 1.22r05 (Build 8353).
KEPAQ Scale
The KEPAQ is a self-administered, Keratoconus-specific scale, recently developed and validated by our group. It consists of a total of 16 questions divided into two sub-scales that measure different constructs. The first part of the scale consists of 7 questions, and evaluated the Emotional compromise of patients secondary to the disease (KEPAQ-E, Table 1). The second sub-scale consists of 9 questions revolving around the Functional compromise secondary to ectasia (KEPAQ-F, Table 2). Al questions are written in a clear and concise manner, and ask the patient about how much they feel the disease handicaps them in a number of different situations. All questions use a Likert-Like response system with a corresponding scoring system, as follows: “Not at all” = 3; “A little” = 2; “Quite a bit” = 1; “A lot” = 0. All patients are also given the possibility of marking “Not Applicable”, if they feel the question does not pertain to any situation in their daily lives. Then, the sum score in converted to a Rasch Derived Score using two tables developed by our group (article currently under peer review) and the subject is given a total of two scores, one for the KEPAQ-E (Table 3) and one for the KEPAQ-F (Table 4) with a higher score meaning less disability caused by disease. When clinicians have a significant number of patients they want to get scores for, they can also perform a Rasch Analysis themselves to get an exact score for their given sample.
 |
Table 1 Emotional Compromise Sub-Scale of the Keratoconus End-Points Assessment Questionnaire (KEPAQ-E) |
 |
Table 2 Functional Compromise Sub-Scale of the Keratoconus End-Points Assessment Questionnaire (KEPAQ-F) |
 |
Table 3 Table for Transforming KEPAQ-E Raw Score to Person Measure, Which Is the Value That Should Be Used for Epidemiological and Clinical Applications, According to Rasch Analysis Theory |
 |
Table 4 Table for Transforming KEPAQ-F Raw Score to Person Measure, Which Is the Value That Should Be Used for Epidemiological and Clinical Applications, According to Rasch Analysis Theory |
Study Protocol
All subjects underwent a clinical evaluation by the main author, and an OCULUS Pentacam (Oculus Optikgeråte GmbH; Wetzlar, Germany) was performed on both eyes in order to get corneal anatomy values, including Belin ABCD classification scores. Visual acuity for the “D” aspect of classification was obtained from the clinical evaluation performed before Pentacam. Application of the KEPAQ was performed in all patients.
Data Analysis
A Rasch Analysis was performed for both sub-scales in order to obtain an interval-level kind of score expressed in an arbitrary unit called “Logits” (as is customary in this kind of analysis). This converted score has been demonstrated to be much superior when compared to the mere sum score as has been previously used by studies using prior analysis methods. Although not the direct objective of this study, psychometric properties of the scale (such as Person Separation Index, among others) were evaluated to determine the adequate behaviour of the scale in the study sample. Rasch Analysis was performed in JMetrik version 4.1.1 (Psychomeasurement Systems LLC; Charlottesville, VA, United States) in a MacBook Air computer running MacOS Catalina Version 10.15.2 (Apple Inc; Cupertino, CA, United States) following the standard protocol for this kind of analysis.
Then, the following data were extracted from the Pentacam of every patient: flat anterior keratometry (K1), steep anterior keratometry (K2), mean keratometry (Km), maximum keratometry (Kmax), thinnest pachymetry, Index of Height Asymmetry (IHA), Index of Height Descentration (IHD), Index of Surface Variance (ISV), Index of Vertical Variance (IVA), Keratoconus Index (KI) and Belin ABCD classification. Eyes were separated into a “better eye” and a “worse eye”. The better eye was arbitrarily defined as the eye with the lowest Kmax value.
Correlation analysis included both Pearson’s or Spearman Correlation, where either one of them was applicable. For Pearson’s Correlation, all five described assumptions were checked. First, both variables were on a continuous-level (as assured by using a Rasch-derived score), and both variables were paired. The third assumption declares there should be a linear relationship between the variables, and this was checked by means of visual inspection of all the confrontation scatterplots. Fourth assumption states that there should be no significant outliers and this was checked and managed accordingly. Fifth assumption states that both variables should show normal distribution. This was checked by means of a Shapiro–Wilk test. In cases when at least one of the variables did not show a normal distribution, a Spearman’s Rank Order Correlation was used.
All descriptive and correlation analysis were performed through IBM SPSS Statistics version 23 (International Business Machines Corporation; Armonk, NY, United States) in a MacBook Air computer running MacOS Catalina Version 10.15.2 (Apple Inc; Cupertino, CA, United States).
Results
A total of 114 patients were included in the study, with 45 (39.47%) subjects being male. Mean age was 28.13 ± 11.57 years. Mean age at the time of ectasia diagnosis was 21.32 ± 9.97 years.
Rasch Analysis: KEPAQ-E
All patients answered the KEPAQ-E sub-scale, and none of them referred to have any problem understanding or answering the questions. Rasch Analysis demonstrated all items to be well-fitting, with Unweighted Mean Square (UMS) values between 0.58 and 1.27, and Weighted Mean Square (WMS) values between 0.96 and 1.14. All items showed adequate ordering as per Andrich’s Thresholds. Person Separation Index and Person Number of Strata were 2.74 and 3.98, respectively. Person Reliability (an analog to Cronbach’s Alpha) was 0.88. Upon evaluating the principal components analysis of standardized residuals, Eigenvalue for the first contrast was 1.48, suggesting a truly unidimensional sub-scale.
Mean Rasch Score for the KEPAQ-E was 2.33 ± 3.40 Logit (First Quartile –0.21 Logit; Median 2.22 Logit; Third Quartile 5.40 Logit). Shapiro–Wilk statistic suggested a non-normal distribution (p < 0.001).
Rasch Analysis: KEPAQ-F
All patients answered the KEPAQ-F sub-scale, and none of them referred to have any problem understanding or answering the questions. Rasch Analysis demonstrated all items to be well-fitting, with UMS values between 0.55 and 1.48, and WMS values between 0.44 and 1.40. All items showed adequate ordering as per Andrich’s Thresholds. Person Separation Index and Person Number of Strata were 3.33 and 4.78, respectively. Person Reliability was 0.91. Upon evaluating the principal components analysis of standardized residuals, Eigenvalue for the first contrast was 1.41, suggesting a truly unidimensional sub-scale.
Mean Rasch Score for the KEPAQ-F was 1.85 ± 3.61 Logit (First Quartile –1.03 Logit; Median 1.00 Logit; Third Quartile 5.46 Logit). Shapiro–Wilk statistic demonstrated a non-normal distribution (p < 0.001).
Worse Eye
For all patients, the “Worse Eye” was defined as that which had the highest Kmax value, correlating to the greater corneal steepness due to disease. For 60 (52.63%) subjects, the best eye was the left one.
For the Belin A criteria (anterior elevation), median value was 2.06 [Interquatile Range (IR) 1.61]. For B (posterior elevation) it was 2.80 (IR 1.77), while for C (corneal thickness) and D (visual acuity) it was 1.90 (IR 1.32) and 2.10 (IR 1.25), respectively. Shapiro–Wilk test demonstrated a non-normal distribution (p < 0.05) for all criteria except for D, which showed normal distribution (p = 0.063).
Upon analysis with the Spearman Rank Order Correlation, all criteria, except for Corneal Thickness (Criteria C) showed a significant inverse correlation with both sub-scales of the KEPAQ (Table 5), meaning that a higher classification value correlated with a lower KEPAQ score (meaning more subjective disability).
Better Eye
For all patients, the “Better Eye” was defined as that which had the lowest Kmax value, correlating to the lesser corneal steepness due to disease. For 60 (52.63%) subjects, the best eye was the right one.
For the Belin A criteria (anterior elevation), median value was 0.60 (IR) 1.98. For B (posterior elevation) it was 1.85 (IR 2.13), while for C (corneal thickness) and D (visual acuity) it was 1.20 (IR 1.10) and 1.30 (IR 1.27), respectively. Shapiro–Wilk test demonstrated a non-normal distribution (p < 0.05) for all criteria.
Upon analysis with the Spearman Rank Order Correlation, none of the Belin ABCD values correlated with the score of either sub-scale of the KEPAQ (Table 6).
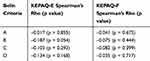 |
Table 6 Spearman Correlation Between the Belin ABCD Criteria in the Better Eye and the Score of Both Sub-Scales of the KEPAQ. No Statistically Significant Correlation Could Be Found |
Discussion
QoL is an inherently hard to define concept, as it includes a myriad of social, economic, and health-related elements. To date, the best way of measuring QoL in patients is by the use of PROMs;2 validated and standardised instruments that directly question the patient about their subjective experience in different realms of their daily lives. Although general-use PROM could be useful under certain circumstances,1 disease-specific PROMs will give a greater insight on the burden of certain conditions over general QoL from a patient’s perspective.2
To date, only two Keratoconus-specific PROMs have been validated: the Keratoconus Outcomes Research Questionnaire (KORQ) and the KEPAQ. The KORQ was developed and initially validated by Khadka et al,5 and its psychometric parameters were recently analyzed by Kandel et al.6 Both studies used Rasch Analysis, a method that has been demonstrated to be much superior when compared to Classical Test Theory methods, such as Principal Components Analysis. The KORQ has also been recently validated in the Colombian population by Balparda and collaborators.7 Nevertheless, a big drawback of the KORQ is that it completely ignores the emotional aspect of patients, a very important realm in QoL measurement. This is specially important as it has been demonstrated that Keratoconus patients have a higher proportion of depressive symptoms8 and psychological distress.9 Therefore, it would be much desirable to have a PROM that could measure emotional distress in a disease-specific manner. On the other hand, although the KORQ has been demonstrated to correlate to visual acuity and contrast sensitivity,5 no published study has demonstrated whether it correlates with corneal distortion, an important element to demonstrate construct validity.
So far, trough two previous studies (articles currently under peer review), Balparda et al. have demonstrated to KEPAQ to show excellent psychometric, reliability, and unidimensionality properties. Nevertheless, no study had ever demonstrated whether this disease-specific PROM correlates with corneal distortion as measured with the Belin ABCD classification.
In the present study, a group of Keratoconus patients was administered the KEPAQ and underwent corneal tomographic measurement with a Pentacam in order to classify their ectasia, in order to demonstrate whether both sub-scales of the scale correlated with corneal distortion and visual function. All correlations were performed trough a Spearman Rank Order Correlation as KEPAQ’s scores demonstrated to be non-normally distributed according to Shapiro–Wilk tests. No element in the better eye demonstrated to correlate with KEPAQ scores in either sub-scale. Nevertheless, A (anterior elevation), B (posterior elevation) and D (Distance visual acuity) in the worse eye all demonstrated to correlate significantly with KEPAQ scores in both sub-scales. The only criterion which did not show a correlation behaviour was C (corneal thickness).
These data demonstrates that corneal distortion and visual function in the patient’s worse eye correlates with both emotional distress and subjective functional handicap in Keratoconus patients. Corneal distortion in the better eye did not demonstrate to correlate, at least in the studied sample.
Although no other study has ever been published on the impact of corneal distortion on QoL as measured by a disease-specific questionnaire (such as the KEPAQ or the KORQ), data from this study could be compared to other publications with a similar design but using general PROMs. Saunier et al10 studied 550 French Keratoconus patients, showing that a corrected distance visual acuity worse than 20/40, a steep keratometry higher than 52.0D and a more severe Keratoconus according to the Amsler-Krumeich classification correlated with a significant reduction in QoL as measured by the National Eye Institute Visual Functioning Questionnaire-25 (NEI VFQ-25). Recently, Tan et al11 found that best-corrected visual acuity in the better eye had the strongest correlation with reading and mobility scores as measured by the Vision Impairment Questionnaire (IVI), while visual acuity in the worse eye correlated significantly with emotional scores. K2 and Kmax in the better eye also displayed significant associations with reading and mobility scores. Finally, Sahebjada et al12 found that vision in the better eye (but not the worse eye) correlated with a significant decrease in QoL as measured by the Vision and Quality of Life Index (VisQoL).
Although it may seem that these results contrast with those given by the present study, there is an important aspect that needs to be taken into account. These studies were performed using non-disease-specific PROMs, while the present study used a disease-specific scale designed for the Keratoconus patient. As has been highlighted in the past, general PROMs may be prone to erroneous measurement under certain conditions, and do not give the same level of insight as disease-specific questionnaires. Therefore, general PROMs cannot be expected to give the same results as those given by disease-specific scales such as the KEPAQ. This may explain the differences in results.
It is interesting that only data from the worse eye correlated with QoL decrease in Keratoconus patients. This may be explained because most ecstatic patients are young, and engage in highly visual-demanding activities, such as driving and going to the cinema. Visual function in the worse eye will greatly impair depth perception and overall visual comfort, therefore causing a greater strain in QoL. Even more, a greater visual handicap in the worse eye may cause more worry about the future and about their overall health on Keratoconus patients (something that is measured by the KEPAQ); therefore explaining findings in the present study.
Conclusions
Criteria A, B, and D from the Belin ABCD classification in the worse eye correlate with QoL affection as measured with the KEPAQ. No findings were demonstrated regarding the better eye.
In the light of these data, it could be suggested that interventions in the worse eye may provide a better improvement in patient’s QoL and therefore it should be the first eye to be operated on.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Miskala PH. Development, use, and interpretation of patient-reported outcomes for clinical decision making in ophthalmology. JAMA Ophthalmol. 2016;134(6):690–692. doi:10.1001/jamaophthalmol.2016.0820
2. Wallace S, Edmond J. In support of ophthalmology-specific patient-reported outcome measures. Ophthalmology. 2019;126(5):690–691. doi:10.1016/j.ophtha.2018.12.007
3. McAlinden C, Khadka J, de Freitas Santos Paranhos J, Schor P, Pesudovs K. Psychometric properties of the NEI-RQL-42 questionnaire in keratoconus. Invest Ophthalmol Vis Sci. 2012;53(11):7370–7374. doi:10.1167/iovs.12-9969
4. Balparda K, Herrera-Chalarca T, Silva-Quintero LA, Torres-Soto SA, Vanegas-Ramírez CM. Development and validation of the “Keratoconus End-Points Assessment Questionnaire” (KEPAQ), a disease-specific instrument for evaluating subjective emotional distress and visual function through Rasch Analysis. Clin Ophthalmol. 2020;14:1287–1296. doi:10.2147/OPTH.S254370
5. Khadka J, Schoneveld PG, Pesudovs K. Development of a Keratoconus-specific questionnaire using Rasch analysis. Optom Vis Sci. 2017;94(3):395–403. doi:10.1097/OPX.0000000000001035
6. Kandel H, Pesudovs K, Ferdi A, et al. Psychometric properties of the Keratoconus outcomes research questionnaire: a save sight Keratoconus registry study. Cornea. 2019.
7. Balparda K, Galarreta-Mira D, Vanegas-Ramírez CM. Traducción y validación del “Cuestionario para Investigación de Resultados en Queratocono” (KORQ) en población Colombiana [Translation and validation of the "Keratoconus Outcomes Research Questionnaire" (KORQ) in Colombian Population]. Arch Soc Esp Oftalmol. 2020. [En Prensa].
8. Moschos MM, Gouliopoulos NS, Kalogeropoulos C, et al. Psychological aspects and depression in patients with symptomatic Keratoconus. J Ophthalmol. 2018;2018:7314308. doi:10.1155/2018/7314308
9. Cingu AK, Bez Y, Cinar Y, et al. Impact of collagen cross-linking on psychological distress and vision and health-related quality of life in patients with Keratoconus. Eye Contact Lens. 2015;41(6):349–353. doi:10.1097/ICL.0000000000000129
10. Saunier V, Mercier AE, Gaboriau T, et al. Vision-related quality of life and dependency in French keratoconus patients: impact study. J Cataract Refract Surg. 2017;43(12):1582–1590. doi:10.1016/j.jcrs.2017.08.024
11. Tan JCK, Nguyen V, Fenwick E, Ferdi A, Dinh A, Watson SL. Vision-related quality of life in Keratoconus: a save sight Keratoconus registry study. Cornea. 2019;38(5):600–604. doi:10.1097/ICO.0000000000001899
12. Sahebjada S, Fenwick EK, Xie J, Snibson GR, Daniell MD, Baird PN. Impact of keratoconus in the better eye and the worse eye on vision-related quality of life. Invest Ophthalmol Vis Sci. 2014;55(1):412–416. doi:10.1167/iovs.13-12929
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

