Back to Journals » Open Access Emergency Medicine » Volume 9
Automated external defibrillation training on the left or the right side – a randomized simulation study
Authors Stærk M , Bødtker H, Lauridsen KG, Løfgren B
Received 22 April 2017
Accepted for publication 10 July 2017
Published 14 September 2017 Volume 2017:9 Pages 73—79
DOI https://doi.org/10.2147/OAEM.S140220
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Mathilde Stærk,1 Henrik Bødtker,1 Kasper G Lauridsen,1–3 Bo Løfgren,1,3,4
1Research Center for Emergency Medicine, Aarhus University Hospital, Aarhus, 2Clinical Research Unit, 3Department of Internal Medicine, Randers Regional Hospital, Randers, 4Institute of Clinical Medicine, Aarhus University, Aarhus, Denmark
Background: Correct placement of the left automated external defibrillator (AED) electrode is rarely achieved. AED electrode placement is predominantly illustrated and trained with the rescuer sitting on the right side of the patient. Placement of the AED electrodes from the left side of the patient may result in a better overview of and access to the left lateral side of the thorax. This study aimed to investigate if training in automated external defibrillation on the left side compared to the right side of a manikin improves left AED electrode placement.
Methods: Laypeople attending basic life support training were randomized to learn automated external defibrillation from the left or right side of a manikin. After course completion, participants used an AED and placed AED electrodes in a simulated cardiac arrest scenario.
Results: In total, 40 laypersons were randomized to AED training on the left (n=19 [missing data =1], 63% female, mean age: 47.3 years) and right (n=20, 75% female, mean age: 48.7 years) sides of a manikin. There was no difference in left AED electrode placement when trained on the left or right side: the mean (SD) distances to the recommended left AED electrode position were 5.9 (2.1) cm vs 6.9 (2.2) cm (p=0.15) and to the recommended right AED electrode position were 2.6 (1.5) cm vs 1.8 (0.8) cm (p=0.06), respectively.
Conclusion: Training in automated external defibrillation on the left side of a manikin does not improve left AED electrode placement compared to training on the right side.
Keywords: automated external defibrillator, pads, basic life support, training
Introduction
Every year, 275,000 people suffer from out-of-hospital cardiac arrest (OHCA) in Europe and survival is only ~10%.1 Defibrillation is a key element in the “chain of survival,” and early defibrillation within minutes improves survival following OHCA.2–5 Use of an automated external defibrillator (AED) reduces time to defibrillation and is therefore widely distributed in the public domain.6
An AED instructs the user through voice prompts and pictorial guidance and is claimed to be easy to use even for untrained laypeople.7 However, studies report that both laypeople and health care professionals do not place AED electrodes correctly, especially the left apicolateral AED electrode is often placed medially.8–10
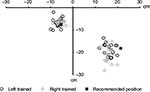
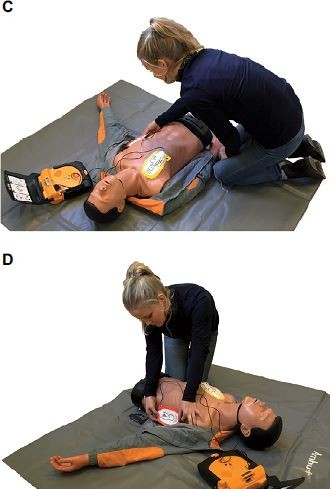
In teaching materials and guidelines from the European Resuscitation Council (ERC), a rescuer using an AED is consistently sitting on the right side of the patient.7,11 However, sitting on the left side of the patient may provide a rescuer easier access to and better overview of the left lateral side of the chest in order to place the left apicolateral AED electrode correctly (Figure 1). Moreover, the left arm of the patient may impede access to the left lateral side of the chest. The position of the rescuer may therefore affect AED electrode placement. No studies have investigated if applying AED electrodes from the left side of the patient improves AED electrode placement compared with application from the right side of the patient.
Accordingly, this study aims to investigate if training in automated external defibrillation on the left side of a manikin improves AED electrode placement compared with training on the right side of a manikin.
Methods
Study design
This is a randomized, controlled, superiority simulation study. Participants were randomized 1:1 to train and apply AED electrodes from the left or right side of a manikin.
Participants were randomized (in blocks to ensure an even number in each experimental group) by drawing a number to train on either the right or left side of the manikin. At the post-course test, participants were randomized by dice roll to start from the right or left side of the manikin.
Participants and ethics
Participants were recruited among laypersons attending basic life support (BLS)/AED courses. Participants holding a BLS/AED instructor certificate were excluded. Prior to study participation, all participants answered a questionnaire including information on gender, age, employment, education, previous BLS training, if holding a BLS/AED instructor certificate, and if participants ever used an AED in a real life emergency.
According to Danish law (Danish Act on Research Ethics, Review of Health Research Projects, Act number 593 of 14 July 2011 section 14 [2]), no ethical review committee approval was required. Verbal and written consents were obtained from all participants.
Data collection
BLS/AED courses had a duration of 4 hours with 8–19 participants per instructor. Both study arms had an equal participant:instructor ratio due to block randomization. BLS/AED instructors were all certified by the Danish First Aid Council and all had clinical experience as emergency medical technicians. During courses, participants trained in small groups of 2–3 persons per manikin. Study investigators ensured that participants were trained according to randomization during the entire course.
After completing the BLS/AED course, participants were asked to operate a training AED (Lifepak® CR-T AED Trainer, PhysioControl, Redmond, WA, USA) and place the AED electrodes on an anatomically realistic torso manikin with arms (AMBU® Man, AMBU, Ballerup, Denmark) identical to the equipment used during training. Participants were guided by AED voice prompt and pictorial guidance on the AED electrodes and did not receive any other help or feedback. Participants applied AED electrodes from both left and right side and were subsequently asked which side they preferred, if any.
Data analysis
A measure tape forming an X-Y coordinate system was placed on the manikin with the top at the jugular notch. AED electrode placement was digitally photographed and compared to the position recommended by the ERC resuscitation guidelines, ie, left apicolateral AED electrode in the left mid-axillary line, approximately level with the V6 electrocardiography electrode, and right sternal AED electrode to the right of the sternum, below the clavicle.12,13 We placed AED electrodes according to the recommendation by the ERC, and a placement of AED electrode by participants within 5 cm of this position was defined as correct, similar to previous studies.8,10,14 Digital data analysis was performed using ImageJ (version 1.46r), and distance from center of the AED electrode to the recommended position was calculated.
Outcomes
The primary outcome was distance from center of the left apicolateral AED electrode to the recommended position.12
Secondary outcomes were: 1) distance from center of the right sternal AED electrode to the recommended position, 2) number of participants who placed the left apicolateral AED electrode within 5 cm of the recommended position, 3) number of participants who placed the right sternal AED electrode within 5 cm of the recommended position, 4) number of participants who moved the manikin’s left arm, and 5) from which side participants preferred to apply AED electrodes.
Statistics
Data were analyzed for normality using histograms, QQ plots, and Shapiro–Wilk test. Variances were tested using standard deviation test. Normally distributed variables are reported as mean (SD). Categorical variables are expressed as number (%). Unpaired continuous data were compared using Student’s t-test. Placement of the right sternal AED electrode by the group trained left vs the group trained right was compared using unequal variance t-test. Paired continuous data were compared using paired t-test. Unpaired categorical data were compared using Fisher’s exact test. Paired categorical data were compared using McNemar’s exact test. No sample size calculation was performed, and it was decided to include 40 participants in this study. All data were analyzed using GraphPad Prism (version 6.01 for Windows; GraphPad Software, La Jolla, CA, USA, www.graphpad.com). A p-value of <0.05 was considered statistically significant.
Results
In total, 40 participants were included and randomized to AED training on the left (n=20) or the right (n=20) side of a manikin, and 39 participants (98%) were analyzed (Figure 2). Baseline characteristics were balanced between groups, except that the group applying AED electrodes from the left side had more previous BLS training. However, the BLS training was on average completed more than 15 years ago for both groups and is not believed to influence our results (Table 1). Data were collected from June 10, 2015 through September 17, 2015.
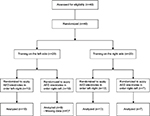  | Figure 2 Study flowchart. Note: aBy mistake no photograph of electrode attachment was recorded before removal of electrodes. Abbreviation: AED, automated external defibrillator. |
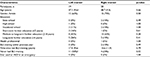  | Table 1 Participant characteristics Notes: Data are expressed as mean (SD) or n (%); adata missing for one participant. Abbreviations: AED, automated external defibrillator; BLS, basic life support. |
There was no significant difference in left apicolateral AED electrode placement (difference 1.0, 95% CI [–2.4 to 0.4), p=0.15] or right sternal AED electrode placement (difference 0.8, 95% CI [0.0 to 1.5], p=0.06) between participants trained and applying from the left or right side of the manikin (Figure 3).
There was no significant difference in the number of participants placing the left apicolateral AED electrode (trained and applied left: n=7 [37%], trained and applied right: n=5 [25%], p=0.50) or right sternal AED electrode (trained and applied left: n=17 [89%], trained and applied right: n=20 [100%], p=0.23) within 5 cm of the recommended position (Figure 4). Within group comparisons are shown in Table 2.
Only a small percentage of participants moved the manikin’s left arm in order to place the left apicolateral AED electrode (trained left side: n=7 [37%], trained right side: n=6 [30%], p=0.74). Moving the left arm did not improve participants’ placement of the left apicolateral AED electrode regarding distance to recommended position (trained left, p= 0.07; trained right, p=0.32).
There was no significant difference in which side participants preferred to apply AED electrodes from. Applying from the left side was preferred by 6 participants (32%) trained on the left side and 10 participants (50%) trained on the right side (p=0.33). Applying from the right side was preferred by 1 participant (5%) trained on the left side and 6 participants (30%) trained on the right side (p=0.09).
Discussion
We found no difference in the placement of AED electrodes when training and applying AED electrodes from the left side compared to the right side of a manikin. Overall, placement of the left apicolateral AED electrode was poor. Only a minor part of participants moved the manikin’s left arm when placing the left apicolateral AED electrode.
In teaching materials and BLS guidelines of the ERC, a rescuer using an AED is sitting on the right side of the patient.7,11 It may be easier to see an instructor demonstrating AED electrode placement when the instructor is sitting on the right side of the manikin. However, sitting on the left side of the patient may provide a better overview compared with sitting on the right side of the patient. Lack of overview may result in poor access to the mid-axillary line where the left apicolateral AED electrode should be placed. Moreover, the patient’s left arm may hinder access to the left lateral side of the patient’s chest and may contribute to incorrect placement of the left apicolateral AED electrode. In the current study, only a minor part of participants moved the manikin’s left arm when placing the left apicolateral AED electrode irrespective of whether AED electrodes were applied from the left or right side. Sitting on the left side of the patient may become a barrier for moving the left arm, as the left arm is “interlocked” between the rescuer and the patient. During the BLS/AED courses, there were no specific instructions to move the left arm. Many resuscitation manikins consist of a torso without arms and training on such manikins may affect the proportion of participants moving the manikin’s left arm. In our study, all participants were trained on manikins with arms.
Our finding of poor left apicolateral AED electrode placement is in accordance with previous studies.8,10,14 One study investigated the placement of different AED electrodes by laypeople and found that only 32% placed both AED electrodes within 5 cm of the recommended position.8 Other studies found that less than one-fourth of health care professionals placed AED electrodes10 and paddles14 within 5 cm of the recommended position. All the mentioned studies8,10,14 found that the left apicolateral AED electrode was most often placed medially compared with the recommended position, which is similar to our findings. In contrast to the poor placement of the left apicolateral AED electrode, placement of the right sternal AED electrode was generally correct in our study as well as the other studies.8,10,14 Importantly, none of the previous studies investigating AED electrode placement8,10,14–16 have reported from which side of the manikin electrodes were applied. In addition to the position of the rescuer, placement of the left apicolateral AED electrode may be affected by inadequate pictorial guidance on the AED electrodes,8 voice prompts, and general AED design.15,16
Ideally, AEDs should be easy to use by untrained rescuers. Implementation of public access defibrillation programs report that AEDs are infrequently used.17 This may be due to multiple factors, eg, poor identification of AEDs,18 fear of doing harm, and lack of self-confidence.19 Effective training may help overcome the barriers for public use of AEDs. Studies found only minor improvements in AED electrode placement following training.20,21 Lack of improvement in electrode placement after training underlines the need for increased focus and innovation on AED electrode placement during training.
In the future, AED training should further emphasize on the correct placement of AED electrodes, especially the left apicolateral AED electrode, by improving visual and verbal instructions including outlining the anatomical landmarks related to AED electrode placement. Furthermore, AED manufacturers should continue to improve pictorial guidance and voice prompts to facilitate effective AED use for trained and untrained users.
Limitations
This study only includes a small sample size. The definition of correct placement within 5 cm of the recommended position is used in accordance with previous studies.8,10,14 The exact influence of this distance on the success of defibrillation is unknown. However, a study investigated the effect of electrode placement and found that small variations (<3 cm) in electrode placement affect defibrillation success in swine.22 Participants placed AED electrodes on a manikin, and it is unknown if this is comparable to AED electrode placement on a human. It is unknown if participants were left- or right-handed and whether this could affect AED electrode placement. However, due to the randomization, we anticipate that left- and right-handed participants were equally distributed between the groups. Further, it seems there is no difference between left- or right-handed persons when performing clinical psychomotor skills.23
Conclusion
Training in automated external defibrillation on the left side of a manikin does not improve left apicolateral AED electrode placement compared to training on the right side. Placement of the left apicolateral AED electrode was poor and future training should emphasize on correct AED electrode placement.
Acknowledgments
All study participants are thanked for their participation in the study. The participant shown in Figure 1 provided written permission for the use of their image in this publication. The members of Life2Save are thanked for collaboration and providing BLS/AED training. Søren Rahbek and Lauge Vammen are thanked for their invaluable contribution to data collection. Camilla Hansen is thanked for her contribution to article figures.
The research received no specific grant from any funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
Atwood C, Eisenberg M S, Herlitz J, Rea T D. Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation. 2005; 67(1):75–80. | ||
BerdowskiJ, Blom MT, Bardai A, Tan HL, Tijssen JG, Koster RW. Impact of onsite or dispatched automated external defibrillator use on survival after out-of-hospital cardiac arrest. Circulation. 2011;124(20):2225–2232. | ||
Blom MT, Beesems SG, Homma PC, et al. Improved survival after out-of-hospital cardiac arrest and use of automated external defibrillators. Circulation. 2014;130(21):1868–1875. | ||
Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW, Hardman RG. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343(17):1206–1209. | ||
Hallstrom AP, Ornato JP, Weisfeldt M, et al. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351(7):637–646. | ||
Hansen CM, Lippert FK, Wissenberg M, et al. Temporal trends in coverage of historical cardiac arrests using a volunteer-based network of automated external defibrillators accessible to laypersons and emergency dispatch centers. Circulation. 2014;130(21):1859–1867. | ||
Perkins GD, Handley AJ, Koster RW, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 2. Adult basic life support and automated external defibrillation. Resuscitation. 2015; 95:81–99. | ||
Nurmi J, Castren M. Layperson positioning of defibrillation electrodes guided by pictorial instructions. Resuscitation. 2005;64(2):177–180. | ||
Mattei LC, McKay U, Lepper MW, Soar J. Do nurses and physiotherapists require training to use an automated external defibrillator? Resuscitation. 2002;53(3):277–280. | ||
Nurmi J, Rosenberg P, Castren M. Adherence to guidelines when positioning the defibrillation electrodes. Resuscitation. 2004; 61(2):143–147. | ||
Koster RW, Baubin MA, Bossaert LL, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2010;81(10):1277–1292. | ||
Deakin CD, Nolan JP, Sunde K, Koster RW. European Resuscitation Council Guidelines for Resuscitation 2010 Section 3. Electrical therapies: automated external defibrillators, defibrillation, cardioversion and pacing. Resuscitation. 2010;81(10):1293–1304. | ||
Soar J, Nolan JP, Bottiger BW, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation. 2015;95:100–147. | ||
Heames RM, Sado D, Deakin CD. Do doctors position defibrillation paddles correctly? Observational study. BMJ. 2001;322(7299):1393–1394. | ||
Mosesso V N, Jr, Shapiro AH, Stein K, Burkett K, Wang H. Effects of AED device features on performance by untrained laypersons. Resuscitation. 2009; 80(11):1285–1289. | ||
Andre AD, Jorgenson DB, Froman JA, Snyder DE, Poole JE. Automated external defibrillator use by untrained bystanders: can the public-use model work? Prehosp Emerg Care. 2004;8(3):284–291. | ||
Agerskov M, Nielsen AM, Hansen CM, et al. Public access defibrillation: great benefit and potential but infrequently used. Resuscitation. 2015;96:53–58. | ||
Aagaard R, Grove EL, Mikkelsen R, Wolff A, Iversen KW, Lofgren B. Limited public ability to recognise and understand the universal sign for automated external defibrillators. Heart. 2016; 102(10):770–774. | ||
Ong ME, Quah JL, Ho AF, et al. National population based survey on the prevalence of first aid, cardiopulmonary resuscitation and automated external defibrillator skills in Singapore. Resuscitation. 2013; 84(11):1633–1636. | ||
Beckers S, Fries M, Bickenbach J, Derwall M, Kuhlen R, Rossaint R. Minimal instructions improve the performance of laypersons in the use of semiautomatic and automatic external defibrillators. Crit Care. 2005;9(2):R110–R116. | ||
Mitchell KB, Gugerty L, Muth E. Effects of brief training on use of automated external defibrillators by people without medical expertise. Hum Factors. 2008;50(2):301–310. | ||
Esibov A, Chapman FW, Melnick SB, Sullivan JL, Walcott GP. Minor variations in electrode pad placement impact defibrillation success. Prehosp Emerg Care. 2016;20(2):292–298. | ||
Alnassar S, Alrashoudi AN, Alaqeel M, et al. Clinical psychomotor skills among left and right handed medical students: are the left-handed medical students left out? BMC Med Educ. 2016;16:97. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.