Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 12
"Anterior" chemabrasion for acne scars treatment
Authors Deprez P
Received 2 March 2018
Accepted for publication 18 June 2018
Published 20 February 2019 Volume 2019:12 Pages 141—149
DOI https://doi.org/10.2147/CCID.S167081
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Jeffrey Weinberg
Philippe Deprez
Research and Development, Skin Tech Pharm Group SL, Castelló d’Empúries, Spain
Abstract: Acne is one of the most prevalent skin conditions seen by dermatologists. Acne scars are a frequent complication of acne that may negatively impact on person’s physical, mental and social well-being, as although active acne can persist for a decade or more, acne scars may persist for a lifetime. Although a wide range of treatments are currently being used, there is a lack of high-quality evidence on which is the most effective treatment for acne scars, especially for those with huge severity. Therefore, based on personal experience of various clinical scenarios, the present study aimed to provide both patients and health care providers insights about the suitability of different new techniques for treating acne scars to better improve the quality of life of patients suffering from this condition.
Keywords: acne, scars, chemabrasion, TCA, chemical peeling
Introduction
A scar is the visible tip of a fibrotic reaction located deep under the skin; therefore, effective treatment is, by definition, a deep remodeling treatment. Acne scars have always been a difficult problem to solve.1 The arrival of high-performance lasers in the market has given rise to an excessive hope.2,3,10 The fact is that, in 2018, when it comes to the treatment of deep acne scars, only few doctors show excellent results associated with relatively safe and not too-expensive techniques. The renaissance of chemical peeling techniques is strong, now that acid solutions are considered as medical devices in Europe, which must undergo deep safety and efficacy controls (Regulation [EU] 2017/745). These controls protect the CE-certified chemical peels from approximated and unstable formulations; they allow for strict reproducibility of results.
It is known that any chemical peel induces a dermal reaction, increasing fibroblastic synthesis.4–6 This synthesis, however, often remains below the limit of what is needed for remodeling the skin with acne scars. What is needed in these cases is not only an increase in collagen synthesis but also a complete reshaping of the deep skin layers. Therefore, long-term repetition of superficial or medium chemical peels has no chance in remodeling the deepest skin layers; hence, there is no possibility of improving the appearance of acne scars, the depth of which is extreme. When it comes to deep peels, the first molecule that comes to mind is phenol. This molecule is known for its extraordinary results on photo aging and has also been used in the treatment of acne scars.3,7 Nevertheless, the author had several cases of resistance of acne scars to phenol peels due to the lack of penetration of the peeling solution into the bottom of deep scars (Figure 1). Another molecule that is widely used for medium depth chemical peels is trichloroacetic acid (TCA). TCA peels can easily reach papillary dermis without a significant risk for the skin.7 Nevertheless, when a deep reticular dermis remodeling is needed, as it is the case of treatment of acne scars, the total amount of TCA needed for reaching a sufficient concentration in deep dermis would be high and therefore very dangerous for the skin. The risk of scarring is evident when very high concentrations of TCA are used: concentrations as high as 50–80% w/w have been used with possible occurrence of worsening of scars.8 On the other hand, the classical chemabrasion method, consisting of applying a large amount of TCA followed by an abrasion, has been also responsible of scarring process, probably due to an excess of TCA more than to the abrasion itself. Other authors have suggested the use of a chemical peeling and dermabrasion combined technique, but always in the order of a peel followed by a dermabrasion. This technique is also known as “chemabrasion”.1 For a better understanding and in order to distinguish between these two techniques, the terms posterior chemabrasion could be used for a peel followed by a dermabrasion and anterior chemabrasion for the technique described in this article that consists of the application of a TCA peel performed after an abrasion.
Finally, this article also describes an evolution of the anterior chemabrasion that the author previously published for the successful treatment of deep stretch marks.8 Generally, a sand paper abrasion is performed followed by a topical anesthesia and the application of a CE-certified TCA containing medical device. At the end, an especially formulated post-peeling cream is applied to stop unwanted inflammation. In the same way as with phenol, the skin is then protected with a layer of bismuth subgallate powder, which is left for 1 week. The skin correctly rebuilds itself under the “scab” during this short period of healing.
Materials and methods
Methods
Inclusion criteria
Patients aged between 18 and 65 years (skin phototypes I–IV) with moderate-to-severe acne scars are included. Skin pre-peel conditioning is mandatory during the 3 weeks before procedure for melano-sedation. Anti-herpes pre-peel prevention is also performed if needed.
Exclusion criteria
People with bleeding diathesis, presence of visible active acne lesions, predisposition to keloid, any deep procedure on the skin to be treated 3 months before treatment (deep lasers, surgery, etc), active herpes, HIV and/or HBV infection, oral retinoic acid use 6 months prior to the procedure, diabetes mellitus type 1 (insulin dependent) or collagen or vascular diseases were excluded. Pregnant or lactating women and those with phototypes higher than IV were also excluded from this study due to the risk of post-inflammatory hyperpigmentation.
Materials
From week –3 and up to peeling date, a pre-peel conditioning was performed as follows: daily cleaning of the skin using a cleanser foam (pH 5.0; SkinTech Cleanser; Skin Tech Pharma Group SL, Castelló d’Empuries, Spain); application of a depigmenting serum (Aclaranse; Aesthetic Dermal, Skin Tech Pharma Group SL) in the morning and application of a depigmenting cream (Blending Bleaching Cream; Skin Tech Pharma Group SL) in the evening for melanocyte sedation. A sun protection is mandatory during the pre-peel period; hence, application of a facial sunscreen SPF 30 up to 50+ (Melablock HSP; Skin Tech Pharma Group) at 9 am and 1 pm was also performed. In the cases where the treatment involved lips or any other region already having suffered from herpes infection, herpes prevention was done using valacyclovir tablets 500 mg (Valtrex; GlaxoSmithKline plc, London, UK) with two tablets/day for 3 days before and 3 days after the peeling. The sandpaper used was a little piece of P220 Wetordry™ Sheet (3M™, USA) that has been previously cleansed and sterilized by gamma rays.
The peeling used was “Easy TCA® classic” (Skin Tech Pharma Group SL), a certified class IIa medical device. This peeling consisted of1 a peeling solution containing TCA at 15% w/w, associated with AHAs and antioxidants, and2 a post-peel mask cream that has to be applied once by the MD, immediately at the end of the peeling. The post-peel mask is not a neutralizing cream but an active cream with a high concentration of vitamins C, E and H; tretinoin precursors; phytic acid, anti-free-radical agents, selenium, methionine, tyrosinase inhibitors, trace elements, fatty acids and various other actives. Note that another form of Easy TCA peel called Easy TCA Pain Control (Skin Tech Pharma Group SL) exists. This solution is not recommended for an application after abrasion since it contains a tiny quantity of phenol, which is responsible for the painless application as claimed in the patent EP2926867A1. No study and no experience sustain the application of phenol after an abrasion; the cardiac risk linked with a too fast increase in phenolaemia leads to its careful recommendation of not using this solution after abrasion.9
Description of the anterior chemabrasion technique
The anterior chemabrasion technique has been developed by the author for the treatment of facial acne scars. This technique represents an evolution of the technique already described for the treatment of stretch marks by the author.8 The results on moderate acne scars can be considered as excellent or even surprising after one session only. In case of pike or box scars, successful results would be achieved by repeating few times the procedure, at 6 weeks distance at least. In the opinion of the author, results seem to be as good or even better than the ones described in medical literature using other methods.
The anterior chemabrasion technique is performed as follows. The patient should have correctly followed the pre-peel regimen prescribed, and no contraindication should be noted. No active papules or pustules are noted on the skin. Next, the skin is strongly rubbed with a gauze soaked in a mixture of acetone and 70° alcohol, at 50/50 proportion, to disinfect and degrease the treatment area. Usually no anesthesia is necessary prior abrasion, since the technique is not painful. Eventually, a tablet of a painkiller (paracetamol 1 g) could be given to the patient half an hour before the procedure. Nerve blocks could also be performed progressively, but the author never used it since the first pain sensation is an important marker for the practitioner, who must stop the abrasion at this moment. Reducing the level of pain with any kind of anesthesia could allow the practitioner to do a too deep abrasion, increasing hence the risk of scarring. Abrasion was performed using a sandpaper rolled around a 10 mL glass vial (Figure 2). Abrasion should be soft and uniform. The pressure to be applied on the skin is a “scratching pressure”, which is the pressure that one applies on his or her hand and fingers for having a sensation of scratching himself or herself.
  | Figure 2 Picture of the method of abrasion used in the present technique. Note: Courtesy of Dr Nenad Stankovic, Serbia. |
The use of little circular movements is recommended for increasing uniformity of abrasion. The end point of abrasion is reached when confluent pinpoints of bleeding appear on the abraded area. With bleeding comes the pain, due to abrasion of the most upper nervous terminations. The abrasion should imperatively be uniform since irregularities would allow a differential acid penetration and irregular results or side effects (Figure 3A). This physical resurfacing makes the skin appear smoother after abrasion.
Abrasion is the first step of the procedure, but before applying any acid or before deepening abrasion of local very deep pike scars, an anesthesia is now needed. A gauze soaked in adrenalinated 2% lidocaine is applied on the abraded area, immediately after, and never before, the patient claims that treatment becomes painful (Figure 3B). Adrenalinated 2% lidocaine application directly on the dermis after abrasion might be felt as a slight burning during few seconds. The topical adrenalinated anesthetic solution creates a vasoconstriction in parallel with a topical numbness, when applied after abrasion. Indeed, abrasion removes the full epidermis, and the anesthetic solution is then applied directly on nervous terminations and superficial blood vessels. The solution is covered by a cling film for avoiding evaporation. How long should the solution stay under occlusion before applying the acid is an interesting question. The main mistake is usually to allow a too long occlusion (say 15 minutes) that lets the anesthetic solution to be fully absorbed. In this case, the peeling is very painful. Anesthetic solution penetrates very quickly after epidermal abrasion, in few minutes. The way to control the onset of numbness is to visually check the appearance of a vasoconstriction that comes together with the anesthetic effect. It is therefore impossible to give a controlled duration for the anesthetic solution contact. The best way is to permanently check the appearance of a vasoconstriction and apply the TCA peel right at this moment. Two problems can appear:1 the occlusion time is too long and the anesthetic solution has been absorbed or the abrasion has been done too superficially and the anesthetic solution cannot penetrate through the residual epidermis. In both cases, the application of TCA is very painful for the patient. A perfect abrasion depth and an application of the acid as soon as vasoconstriction appears are the two controls we can have on this phase of the treatment (Figure 3C).
Now that the skin is ready, the peeling is applied on the whole face. Like normal peelings, only one coat of the Easy TCA solution triggers pure white or even gray–white frosting when applied on the abraded area. The Easy TCA solution penetrates to the reticular dermis (Figure 3D). Occlusion is not needed, as this is a nonocclusive technique. Finally, after obtaining the desired frosting, the post-peel mask cream is generously applied. Yellskreen® (bismuth subgallate powder) is applied on the post-peel mask on which it sticks to form a protective scab. This scab should be left in place during 7 days (Figure 3E). The yellow scab needs no renewing, removing or any other maintenance; it just stays on the skin during 6 days. At days 3 and 6, the patient is controlled to check if an infection developed. Eventual infection appears as red dots around the yellow crust that should never be removed. In case of infection, the patient should be given an oral antibiotic therapy that should solve the problem in very few days. At day 6, the patient himself or herself applies a thick coat of sterile white Vaseline that is impermeable to transepidermal water loss (TEWL). TEWL accumulates under the yellow scab that is not water soluble and unsticks the yellow powder scab at day 7. Evidently, the presence of the yellow scab induces a limitation in everyday activities of the patient as would do any kind of bandage or scabs occurring after any deep dermal procedure.
Use of other methods for removing the epidermis, before applying the peeling solution
Pixelized lasers (fractional lasers, ablative and non-ablative) have been used immediately before application of Easy TCA peel.11 This procedure called pixel peel is more painful when the laser is used compared to a dermaroller or a “dermapen microperforation”. The result of a skin pixelization prior to an Easy TCA peel is comparable if laser or not laser skin perforation is used. Globally, a “pixel peel” is much less efficient than an anterior chemabrasion. In the author’s opinion, the difference of results between a skin focal pixelization (dermaroller, dermapen, stamps) and a full skin abrasion (sandpaper) could be compared to the difference of results between a laser deep dermal full-face resurfacing and a fractional laser.
Ablative lasers could be used for removing uniformly the epidermis before application of the Easy TCA, but the technique would be much more painful and would need anesthesia that would modify the clinical symptoms and the security of the procedure. In addition, a sand paper, correctly manipulated, allows to remove epidermis exactly up to the grenz zone, thanks to the fact that there is no vascularization inside the epidermis. Appearance of the first blood droplets, and the pain, is a strict indicator that the sandpaper overpasses the epidermis. Moreover, lasers could induce a collateral thermal damage to the cells that are supposed to regenerate the skin after procedure, slowing down the skin healing and increasing the risk of side effects.
Treatment of severe scars: “double” anterior chemabrasion technique
Some acne scars on thick skin really represent a challenge: acne scars are large and deep. At first sight, we would say to the patient that the peeling option has to be discarded and that several surgical procedures should be used for softening the aspect of the skin: fat transfer, punch, lift, etc. Figures 4 and 5 show patients with severe acne scars; nevertheless, the author used for these patients another deeper technique consisting of the “classical” anterior chemabrasion described here, followed by a focal diamond drill abrasion for deeper and larger acne scars. This technique was performed following these steps: first of all, before abrasion using a sandpaper (P220 Wetordry), disinfect (alcohol or chlorhexidine) and degrease (acetone) the area. Such an abrasion is not painful as long as the area of basal layer of the epidermis is not touched. The pain usually appears at the same moment as the first pinpoints of bleeding. After abrasion, a gauze soaked in adrenalinated 2% lidocaine is applied on the abraded area and covered by a cling film for avoiding evaporation. Anesthesia appears at the same time the bleeding stops. Now, sandpaper abrasion can continue up to the end point: surface bleeding. Then, another topical anesthesia is applied again. After the second anesthesia is considered as efficient, by a focal diamond drill abrasion is carefully performed on the deeper scars, not on the whole area; therefore, a “bullet”-type abrasion head is used. In Figure 5B, the end point of second abrasion is shown. MD and assistant should wear a protection on clothes, hands, face and eyes for performing this technique; a mask is also necessary. Diamond drill abrasion could intensively spray blood all around.
At the end of the diamond drill abrasion, a gauze soaked in adrenalinated 2% lidocaine is again applied on the abraded area to stop the pain and bleeding and to prepare the Easy TCA application. Several minutes after, anesthesia is effective and only one coat of Easy TCA is uniformly applied on the full face. When passing on the recently abraded areas, a gray frosting appears immediately. When abrasion and Easy TCA application are over, a thick coat of post-peel mask cream is applied on the skin. Yellskreen (bismuth subgallate) powder is stacked directly on the post-peel mask exactly on the abrades areas; it will build a protective scab that stays in place during 7 days. Therefore, the patient leaves the clinic wearing the powder. Under the Yellskreen (non-water-soluble scab), healing is usually very fast.
Figure 6 shows the treatment to be followed depending on the severity of the scars. In both single and double anterior-chemabrasion techniques, the recommended post-peel care is summarized in Figure 7.
  | Figure 6 Diagram depicting the procedure to apply depending on the severity of the acne scars. Abbreviation: TCA, trichloroacetic acid. |
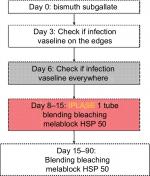  | Figure 7 Post-peel care summary after treating scars with the anterior chemabrasion technique. |
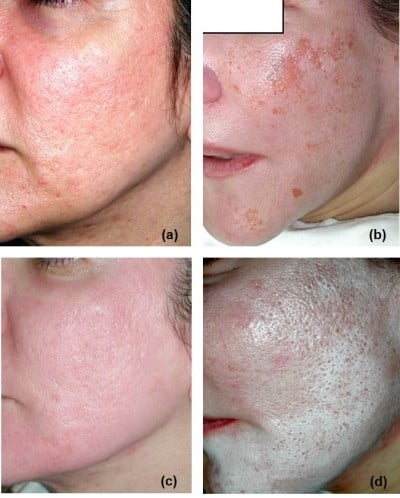
Results
During the last 20 years, several patients have been treated using both single and double anterior chemabrasion techniques, and the results provided herein by different practitioners show the suitability of these procedures for the treatment of moderate and severe acne scars. Figures 8 and 9 show results of the single anterior chemabrasion technique with Easy TCA on facial moderate acne scars, while Figures 4, 5, 10 and 11 show results of the double anterior chemabrasion technique. Single anterior chemabrasion technique using Easy TCA showed good results with an easy and safe post-peel period.
It is interesting to note some aspects related to the double anterior chemabrasion technique. 1) Usually, skin diamond drilling is performed only in the operating theater and under general anesthesia. Nevertheless, this technique shows that a diamond drill abrasion is possible without general anesthesia. A “sequential” topical anesthesia, as described in the article, is absolutely effective. 2) At day 7, skin is basically healed, and inflammation level is very low. This is much faster as could be foreseen with such a deep treatment. Notwithstanding, the double anterior chemabrasion is a difficult and potentially dangerous technique that should be done only by duly trained practitioners. The technique itself is in reality not very difficult: the only real concern is to perform a uniform abrasion and not apply a too large volume of acid. Uniformity is the key word.
Side effects and risks
The main risks of this procedure are pigment disorders, scarring, infections, insufficiency of results, mistakes in indications and procedure application. Surprisingly, when the procedure is realized in good conditions, by a trained practitioner, the rate of side effects is extremely low. Nevertheless, the strict respect of every step is essential. For example, a usual mistake is the use of an anesthetic cream previously to the peel that modifies the semiology and increases the risk. The use of other type of acids, other formulations and/or other concentrations is potentially linked with a higher risk of scarring or pigmentation problems. The non-respect of pre-peel conditioning or post-peel treatment is also a risk of increasing side effects. The use of a thicker or a thinner sandpaper (different than P220) could give irregular or insufficient results.
Discussion
Acne scars treatment has always been a difficult goal to achieve. Hereby, the author presents an innovative and daring technique, made possible by the release of new chemical medical devices. This technique can be subdivided into three stages: 1) “simple anterior chemabrasion”, intended for treating of moderate scars, 2) “anterior chemabrasion followed by a dermapen microperforation” intended for medium and deep acne scars, and 3) double anterior chemabrasion, intended for deep or very deep acne scars.
This nonsurgical procedure is therefore sensitive and practitioner dependent. However, the strict respect of the treatment rules is the best way to help our patients and give them a new hope for a skin with scars much less visible. The procedure has also been applied on traumatic or surgical scars with success in a very little number of cases.
Conclusion
Chemical peels are a useful tool for treating active acne, but they were not considered as an effective treatment for severe acne scars. However, the present study has demonstrated that performing a skin abrasion prior to the application of a chemical peeling (Easy TCA) is a good alternative for treating these skin problems. The present study describes different and novel techniques for the treatment of moderate and severe acne scars considering multiple advantages and excellent results obtained.
Acknowledgments
Some patient pictures were kindly provided by Dr Helen Shuba and Dr Nenad Stankovich. All patients provided written informed consent.
Disclosure
The author reports no conflicts of interest in this work.
References
Andre P, Haneke E, Marini L, Payne CR. Cosmetic Medicine and Surgery. Vol. 822. CRC Press; 2017. | ||
Magnani LR, Schweiger ES. Fractional CO2 lasers for the treatment of atrophic acne scars: a review of the literature. J Cosmet Laser Ther. 2014;16(2):48–56. | ||
Abdel HR, Shalaby K, Zaher H, et al. Interventions for acne scars. Cochrane Database Syst Rev. 2016;3(4):CD011946. | ||
Small R, Hoang D, Linder J. A practical guide to chemical peels microdermabrasion and topical products. Lippincott Williams Wilkins. 2012;208:111–128. | ||
Peters W. The chemical peel. Ann Plast Surg. 1991;26(6):564–571. | ||
Omi T, Sato S, Numano K, Kawana S. Ultrastructural observations of chemical peeling for skin rejuvenation (ultrastructural changes of the skin due to chemical peeling. J Cosmet Laser Ther. 2010;12(1):21–24. | ||
Kontochristopoulos G, Platsidaki E. Chemical peels in active acne and acne scars. Clin Dermatol. 2017;35(2):179–182. | ||
Deprez P. Textbook of Chemical Peels. Superficial, Medium, and Deep Peels in Cosmetic Practice. 2nded ed. CRC Press; 2017:152–181. | ||
Landau M. Cardiac complications in deep chemical peels. Dermatol Surg. 2007;33(2):190–193. | ||
Xu Y, Deng Y. Ablative fractional CO2 laser for facial atrophic acne scars. Facial Plast Surg. 2018;34(2):205–219. | ||
Connolly D, Hl V, Mariwalla K, Saedi N, Scarring-Pathogenesis A. Evaluation, and treatment options. J Clin Aesthet Dermatol. 2017;10(9):12–23. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.








