Back to Journals » Clinical Ophthalmology » Volume 15
Anatomical and Functional Recovery Kinetics After Epiretinal Membrane Removal
Authors Vingopoulos F , Koulouri I, Miller JB , Vavvas DG
Received 12 June 2020
Accepted for publication 14 September 2020
Published 15 January 2021 Volume 2021:15 Pages 175—181
DOI https://doi.org/10.2147/OPTH.S264948
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Filippos Vingopoulos,* Ismini Koulouri,* John B Miller, Demetrios G Vavvas
Retina Service, Department of Ophthalmology, Massachusetts Eye and Ear, Harvard Medical School, Boston, MA, USA
*These authors contributed equally to this work
Correspondence: Demetrios G Vavvas
Retina Service, Department of Ophthalmology, Massachusetts Eye and Ear, Harvard Medical School, 243 Charles St, Boston, MA 02114, USA
Email [email protected]
Purpose: To investigate the nature of anatomical and functional recovery kinetics after epiretinal membrane (ERM) removal.
Methods: The records of 42 patients (45 eyes) with idiopathic ERM treated with pars plana vitrectomy and surgical peeling of the ERM performed by a single surgeon at Massachusetts Eye and Ear between 2012 and 2017 were retrospectively reviewed. Outcome measures included spectral domain optical coherence tomography-measured central macular thickness (CMT) pre-operatively and at post-operative day 1, week 1, months 1, 3, 6, 12 and 24 as well as best-corrected visual acuity (BCVA). Correlations between baseline or early values and final anatomical and functional outcomes were investigated.
Results: Improvement in CMT was statistically significant after 1 week, 1, 3, 6, 12 and 24 months (p < 0.01). BCVA improvement was statistically significant after 1, 6, 12 and 24 months follow-up (p< 0.01). The improvement of BCVA and CMT with time was found to be logarithmic (R2 =0.96, R2 =0.84) suggesting that early (< 30 days) post-operative functional and anatomical changes may be predictive of long-term outcomes. Preoperative BCVA and CMT revealed a weak positive correlation with the respective BCVA and CMT at 24 months (R2=0.13 and R2=0.16). When plotted as a percentage of the fellow normal eye CMT, first week proportional improvement in CMT from pre-operative baseline was found to be correlated with final CMT proportional decrease (R2=0.72) suggesting that first week postoperative CMT could be predictive of final CMT.
Conclusion: There is a logarithmic improvement in CMT and BCVA after ERM peel with BCVA improvement following the CMT improvement. Early (less than 30 days) post-operative anatomical changes can be predictive of long-term anatomical outcomes.
Keywords: epiretinal membrane, recovery kinetics, prognosticators, early optical coherence tomography
Introduction
Idiopathic epiretinal membrane (ERM) affects about 11% of the general population aged 49 years or older.1 It is characterized by the growth of fibrocellular tissue on the internal limiting membrane (ILM), the basement membrane of the Muller cells.2,3 Treatment of symptomatic ERM remains pars plana vitrectomy (PPV) with surgical peeling of the ERM which results in very good outcomes with 80% of patients improving by more than two lines of vision.4
Despite fairly universal surgical approaches, both anatomic and functional outcomes can be quite variable. Many studies have tried to find predictors of final outcomes, but they have focused predominantly on pre-operative findings. These previous studies have examined duration of symptoms, preoperative best corrected visual acuity (BCVA), pre-operative metamorphopsia, as well as optical coherence tomography (OCT) parameters, such as central macular thickness (CMT), ellipsoid zone (EZ) integrity and ganglion cell–inner plexiform layer thickness as potential prognosticators of both final BCVA and anatomic improvements.4–27
To our knowledge, very few studies have reported on early (less than 30 days) visual and anatomical changes after ERM removal and no study has attempted to understand the kinetics of anatomical and functional changes in this early postoperative period. Hence, we herein present a retrospective study on early and late kinetics of spectral domain optical coherence tomography (SD-OCT) and functional findings after ERM removal without intentional ILM peeling and correlate these with outcomes.
Methods
Patient Selection
The medical records of patients with idiopathic ERM who underwent PPV with surgical removal of an idiopathic ERM between January 2012 and June 2017 under the care of a single surgeon (DGV) were reviewed. Inclusion criteria included patients who had performed SD-OCT before the surgery and after the 1st day, 1st week and 1st month. Patients with concurrent macular holes, macular disease, venous or arterial occlusion, diabetic retinopathy, retinal tear, retinal detachment, endophthalmitis or trauma were excluded. This study was conducted in accordance with the tenets of the Declaration of Helsinki and received approval from the Institutional Review Board of Massachusetts Eye and Ear Human Studies Committee (title: 1,351,674-2, protocol:1,351,674-2/(18-172H)) prior to its commencement. Patient consent was waived due to the retrospective nature of this study and Health Insurance Portability and Accountability Act (HIPPA) compliance was maintained throughout.
Surgical Procedure and Post Surgical Care
All surgical procedures were performed in a teaching hospital with surgical fellows under the supervision of a single surgeon (DGV) using standard 3 port vitrectomy (25g or 27g) and no intentional ILM peeling. No dye was used to investigate if ILM was inadvertently peeled with the ERM. Triamcinolone acetonide staining of ERM was used for the majority of these cases. Post operative care included routine antibiotic drops for a week as well as topical steroids and non-steroidal medications for 4–6 weeks post op.
Anatomical and Functional Outcomes
SD-OCT was performed using Cirrus HD-OCT (Carl Zeiss Meditec AG, Jena, Germany) or Spectralis SD-OCT (Heidelberg Engineering GmbH, Heidelberg, Germany) pre-operatively and post-operative on day 1, week 1, months 1, 3, 6, 12 and 24. ETDRS BCVA was measured on the respective follow-up dates and converted to the logarithm of the minimum angle of resolution (logMAR) for statistical analysis. Outcomes included anatomical changes based on CMT and functional changes based on BCVA. Proportional early CMT and BCVA changes form the pre-operative baseline values were also evaluated as a percentage of the final respective values at 24 months follow-up and as a percentage of the healthy fellow eye CMT and BCVA.
Statistics
Statistical analysis was performed using the statistical software STATA (College Station, TX, USA). Spearman correlation coefficient (r) was used to investigate strength and direction (positive or negative) of linear relationships between paired variables. Paired t-test analysis was performed with p values <0.05 considered as an indication of statistically significant results.
Results
Out of 200 patients (213 eyes) that underwent ERM removal between 2012 and 2017 in our clinic, seventy nine (79) eyes of 71 patients had 1st day and 1st week SD-OCT, 35 eyes were excluded due to concurrent macular hole (n= 20), diabetic retinopathy (7), branch venous occlusion (3), retinal tear (2), retinal detachment (1), or history of endophthalmitis (1). After these exclusions, there were 45 eyes of 42 patients that were included for analysis in this study, 22 male and 20 female, with a mean age of 73 ± 13.4 years and a mean follow-up of 20 months. Thirty eyes had at least 12 months follow up and 26 eyes had at least 24 months follow-up. In terms of lens status at the time when ERM was removed, 25 eyes were pseudophakic and 20 phakic. Of the 20 phakic eyes, 15 became pseudophakic during the follow-up period. Baseline characteristics are shown in Table 1.
 |
Table 1 Baseline Characteristics |
Mean CMT was 475 ± 129.7 preoperatively improving to 445 ± 110.3 at 1st day, 408 ± 106.4 at 1st week, 381 ±72.0 at 1st month, 361± 58.6 at 3 months, 365 ± 75.2 at 6 months, 356 ± 59.2 at 12 months and 346 ± 57.3 at 24 months post-operatively. Improvement in CMT was statistically significant after the 1st week (p=0.005), 1st month (p<0.001), 3 months (p=0.001), 6 months (p=0.001), 12 months (p < 0.001) and 24 months (p < 0.001) Proportional decrease of CMT compared to the baseline pre-operative values as a percentage of the final CMT reached at 24 months was 24% at 1st day, 54% at 1st week, 74% at 1st month, 88% at 3 months, 92% at 6 months and 95% at 12 months. When plotted, the improvement of CMT was found to be logarithmic with time, with an R2 of 0.96 (Figure 1).
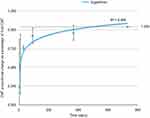 |
Figure 1 Proportional decrease of CMT values as a percentage of the final CMT at 24 months was found to be logarithmic with time. |
Mean BCVA was 0.49 ± 0.43 (Snellen equivalent of 20/60) pre-operatively and 0.80 ± 0.56 (20/125) at 1st day, 0.40 ±0.24 (20/50) at 1st week, 0.33 ± 0.26 at 1st month (20/40), 0.26 ± 0.21 (20/36) at 3 months, 0.28 ± 0.25 at 6 months (20/38), 0.22 ± 0.20 (20/32) at 12 months and 0.25 ± 0.23 (20/35) at 24 months. BCVA was significantly worse at 1st day post-operatively (p=0.003), not significantly different from the pre-operative values at 1st week (p=0.085), significantly improved at 1st month (p=0.018), 6 months (p=0.006), 12 months (p=0.0001) and at 24 months (p=0.00082) post-operatively.
When plotted over time, the improvement of CMT and BCVA were found to be logarithmic (R2 = 0.84 and R2 = 0.96 respectively) suggesting that early (less than 30 days) post-operative structural and functional changes may be predictive of long-term outcomes (Figure 2).
Preoperative BCVA revealed a weak positive correlation with BCVA at 12 and 24 months. (R2= 0.12, r=0.348 and R2=0.13, r=0.36 respectively with p<0.05) (Figure 3A). Likewise, there was only a weak positive correlation between preoperative CMT and CMT measurements at 12 and 24 months (R2= 0.19, r=0.44 and R2=0.16, r=0.40 respectively with p<0.05) (Figure 3B).
When proportional decrease of CMT compared to the baseline pre-operative values was plotted as a percentage of the fellow normal eye CMT, the respective values were 14.7% at 1st day, 32% at 1st week, 50% at 1st month, 64% at 3 months, 63% at 6 months, 62% at 12 months and 68.9% at 24 months post-operatively. When plotted, the improvement of CMT was found to be logarithmic with time, with an R2 of 0.94 (Figure 4).
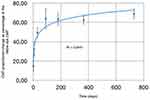 |
Figure 4 Proportional decrease of CMT values as a percentage of the fellow normal eye CMT was found to be logarithmic with time. |
Of note, although CMT decreased significantly after ERM removal, it never reached the CMT of the normal fellow eye, which is in accordance with previous studies.28–30
When plotted as a percentage of the fellow normal eye CMT, first week proportional improvement in CMT from pre-operative baseline was found to be correlated with final CMT proportional decrease (R2= 0.72, r= 0.85, p<0.001) (Figure 5). Hence, it appears that early postoperative CMT could be predictive of final CMT, more so than preoperative baseline CMT. (r=0.846 vs r=0.405) Our study was found to be underpowered in detecting a similar relationship between early postoperative and final BCVA or between CMT and BCVA (sample size needed N= 66 and N=91 respectively).
Of interest, when CMT and BCVA scatter-plots with time are over-layered, the logarithmic improvement in BCVA seems to follow the logarithmic decrease in CMT. The worsening in 6-month mean BCVA is attributed to four patients developing cataract and was eliminated by cataract extraction and IOL placement by the 12th month of our follow-up (Figure 2).
In the phakic cohort, mean pre-operative CMT was significantly higher than in the pseudophakic cohort (p<0.05). CMT of the two cohorts was not found to be significantly different at any of the follow-up time points. Similarly, proportional decrease of CMT as a percentage of the preoperative CMT was not found to be significantly different at any of the follow-up time points either. Of note, in our cohort of 45 eyes that underwent ERM removal without intentional ILM peeling, there were no recurrences noted at 24 months of follow-up.
Discussion
To our knowledge, this is the first study reporting on the early (less than 30 days) kinetic functional and anatomical changes after ERM removal as prognosticators of final outcomes. Our study reports on proportional decrease in CMT compared to pre-operative baseline values as a percentage of the final CMT, in order to account for any differences between the pre-operative baseline values.
Several studies have attempted to correlate BCVA and CMT values at various post-operative time-points mostly rendering poorly correlated anatomical and functional results.6,8,10,11 Our early postoperative kinetics analysis revealed a logarithmic improvement in BCVA over time that appears to follow the logarithmic decrease in CMT. As described above, following ERM removal, the CMT reached 24% of the final CMT at 1st day, 54% at 1st week, 74% at 1st month, 88% at 3 months, 92% at 6 months and 95% at 12 months. The logarithmic improvement of CMT with time (R2 = 0.84) suggest that early (less than 30 days) post-operative anatomical changes appear to be predictive of long-term outcomes. To date, only two studies have reported on early (less than 30 days) OCT changes after ERM removal with intentional ILM peeling; none reported on early CMT changes. The first study Clark et al31 reported on RNFL changes at 1 week post op, with 31% of patients having swelling of the arcuate nerve finer layer (SANFL). In the second study, Scupola et al32 analyzed the RNFL changes identified in 39 out of 46 eyes (84.8%) at 14 days post-op.
In terms of functional results, in our study following ERM removal, the logMAR VA decreased on average to 0.8 (from 0.49 pre-operatively) on the 1st day, and improved to 0.4 at 1st week, 0.33 at 1st month, 0.26 at 3 months, 0.28 at 6 months, 0.22 at 12 months and 0.25 at 24 months. The logarithmic improvement of BCVA with time (R2 = 0.96) suggest that early (less than 30 days) post-operative functional changes appear to be predictive of long-term outcomes for our cohort of patients but not necessarily for an individual patient. These results are in accordance with those of Scupola etal's study that found rapid improvement of the BCVA during the 1st postoperative month.
Of the parameters previously studied as potential final BCVA prognosticators, baseline preoperative BCVA4–6,11,13–15,20,22,23 and baseline preoperative CMT14,15,21 have been widely suggested to be well correlated with the final visual outcome. In this study, preoperative BCVA and CMT only revealed a weak positive correlation with final BCVA and CMT (R2= 0.13 and R2=0.16) (Figure 3A and B) while early postoperative CMT was predictive of final CMT, more so than preoperative baseline CMT (R2=0.72 vs R2=0.16). Pre-operative ellipsoid zone integrity (formerly called IS/OS junction) has also been proposed as a prognosticator for final BCVA by several studies9–11,13,17–19 while other studies found no significant correlation.21,33,34 In accordance with our findings, Kim et al12 among other factors suggested first postoperative month CMT as a good prognosticator of final BCVA at 12 months.12 In terms of lens status, Pesin et al6 reported the presence of preoperative pseudophakia to be associated with significantly greater BCVA improvement at 6 months compared to baseline phakic eyes. Lastly, recent evidence suggests that macular ganglion cell–inner plexiform layer (GC-IPL) thickness may also be correlated with postoperative visual outcomes after ERM peeling,35 yet with conflicting evidence on whether decreased GC-IPL thickness is positively16,25,27 or negatively24,26 correlated with BCVA improvement and final BCVA.
A limitation of this study apart from its retrospective nature is that it does not report on SD-OCT-based overall macular volume, as readings differ between the two SD-OCT devices that were used, Heidelberg and Cirrus. Another limitation of this study is that staining was not performed following each procedure to ascertain in how many cases the ILM was or was not spontaneously peeled along with the ERM.
Conclusion
Early postoperative kinetics analysis revealed a logarithmic improvement in BCVA over time that appears to follow the logarithmic decrease in CMT. More than 50% of the improvement occurs in the first week, 75% by the 1st month and almost 90% by the 3rd month.
Early (less than 30 days) post-operative anatomical and functional changes appear to be predictive of long-term outcomes. Incorporating first week post-ERM peeling SD-OCT in the clinical practice may help offer the patient valuable information about their final outcome.
Funding
No funding sources.
Disclosure
John Miller reports personal fees from Alcon, Zeiss, Heidelberg, Allergan, Sunovion, and Genentech and grants from Lions International, outside the submitted work. The authors report no other potential conflicts of interest for this work.
References
1. Mitchell P, Smith W, Chey T, et al. Prevalence and associations of epiretinal membranes: the Blue Mountains Eye Study, Australia. Ophthalmology. 1997;104(6):1033–1040.
2. Hiscott P, Sheridan C, Magee RM, Grierson I. Matrix and the retinal pigment epithelium in proliferative retinal disease. Prog Retin Eye Res. 1999;18(2):167–190.
3. Wollensak G, Spoerl E, Grosse G, Wirbelauer C. Biomechanical significance of the human internal limiting lamina. Retina. 2006;26(8):965–968.
4. Wong JG, Sachdev N, Beaumont PE, Chang AA. Visual outcomes following vitrectomy and peeling of epiretinal membrane. Clin Experiment Ophthalmol. 2005;33(4):373–378.
5. Rice TA, De Bustros S, Michels RG, et al. Prognostic factors in vitrectomy for epiretinal membranes of the macula. Ophthalmology. 1986;93(5):602–610.
6. Pesin SR, Olk RJ, Grand MG, et al. Vitrectomy for premacular fibroplasia: prognostic factors, long-term follow-up, and time course of visual improvement. Ophthalmology. 1991;98(7):1109–1114.
7. Massin P, Allouch C, Haouchine B, et al. Optical coherence tomography of idiopathic macular epiretinal membranes before and after surgery. Am J Ophthalmol. 2000;130(6):732–739.
8. Asaria R, Garnham L, Gregor ZJ, Sloper JJ. A prospective study of binocular visual function before and after successful surgery to remove a unilateral epiretinal membrane. Ophthalmology. 2008;115(11):1930–1937.
9. Mitamura Y, Hirano K, Baba T, Yamamoto S. Correlation of visual recovery with presence of photoreceptor inner/outer segment junction in optical coherence images after epiretinal membrane surgery. Br J Ophthalmol. 2009;93(2):171.
10. Suh MH, Seo JM, Park KH, Yu HG. Associations between macular findings by optical coherence tomography and visual outcomes after epiretinal membrane removal. Am J Ophthalmol. 2009;147(3):473–480.e473.
11. Falkner-Radler CI, Glittenberg C, Hagen S, Benesch T, Binder S. Spectral-domain optical coherence tomography for monitoring epiretinal membrane surgery. Ophthalmology. 2010;117(4):798–805.
12. Kim J, Rhee KM, Woo SJ, et al. Long-term temporal changes of macular thickness and visual outcome after vitrectomy for idiopathic epiretinal membrane. Am J Ophthalmol. 2010;150(5):701–709.e701.
13. Inoue M, Morita S, Watanabe Y, et al. Preoperative inner segment/outer segment junction in spectral-domain optical coherence tomography as a prognostic factor in epiretinal membrane surgery. Retina. 2011;31(7):1366–1372.
14. Kunikata H, Abe T, Kinukawa J, Nishida K. Preoperative factors predictive of postoperative decimal visual acuity ≥ 1.0 following surgical treatment for idiopathic epiretinal membrane. Clin Ophthalmol. 2011;5:147–154.
15. Shimada Y, Sakurai S, Naito K, et al. Multifocal electroretinogram and optical coherent tomography: prediction of visual outcome after epiretinal membrane removal. Clin Exp Optom. 2011;94(3):296–301.
16. Koo H, Rhim W, Lee E. Morphologic and functional association of retinal layers beneath the epiretinal membrane with spectral-domain optical coherence tomography in eyes without photoreceptor abnormality. Graefes Arch Clin Exp Ophthalmol. 2012;250(4):491–498.
17. Kim JH, Kim YM, Chung EJ, et al. Structural and functional predictors of visual outcome of epiretinal membrane surgery. Am J Ophthalmol. 2012;153(1):103–110.e101.
18. Shimozono M, Oishi A, Hata M, et al. The significance of cone outer segment tips as a prognostic factor in epiretinal membrane surgery. Am J Ophthalmol. 2012;153(4):698–704.e691.
19. Cobos E, Arias L, Ruiz-Moreno J, et al. Preoperative study of the inner segment/outer segment junction of photoreceptors by spectral-domain optical coherence tomography as a prognostic factor in patients with epiretinal membranes. Clin Ophthalmol. 2013;7:1467–1470.
20. García-Fernández M, Castro Navarro J, González Castaño C, et al. Epiretinal membrane surgery: anatomic and functional outcomes. Archivos de la Sociedad Española de Oftalmología. 2013;88(4):139–144.
21. Kim JH, Kang SW, Kong MG, Ha HS. Assessment of retinal layers and visual rehabilitation after epiretinal membrane removal. Graefes Arch Clin Exp Ophthalmol. 2013;251(4):1055–1064.
22. Shiono A, Kogo J, Klose G, et al. Photoreceptor outer segment length: a prognostic factor for idiopathic epiretinal membrane surgery. Ophthalmology. 2013;120(4):788–794.
23. Dawson SR, Shunmugam M, Williamson TH. Visual acuity outcomes following surgery for idiopathic epiretinal membrane: an analysis of data from 2001 to 2011. Eye (Lond). 2014;28(2):219–224.
24. Lee E, Yu H. Ganglion cell-inner plexiform layer thickness after epiretinal membrane surgery: a spectral-domain optical coherence tomography study. Ophthalmology. 2014;121(8):1579–1587.
25. Pierro L, Iuliano L, Gagliard M, et al. Role of ganglion cell complex in visual recovery following surgical internal limiting membrane peeling. Graefes Arch Clin Exp Ophthalmol. 2015;253(1):37–452.
26. Park S, Byon I, Kim H. Analysis of the ganglion cell layer and photoreceptor layer using optical coherence tomography after idiopathic epiretinal membrane surgery. Graefes Arch Clin Exp Ophthalmol. 2015;253:207–214.
27. Song S, Yong M, Smiddy W. Ganglion cell layer thickness and visual improvement after epiretinal membrane surgery. Retina. 2016;36(2):305–310.
28. Lee J, Kim I. Outcomes of idiopathic macular epiretinal membrane removal with and without internal limiting membrane peeling: a comparative study. Jpn J Ophthalmol. 2010;54:129–134.
29. Pournaras C, Emarah A, Petropoulos I. Idiopathic macular epiretinal membrane surgery and ILM peeling: anatomical and functional outcomes. Semin Ophthalmol. 2011;26:42–46.
30. Ripandelli G, Scarinci F, Piaggi P. Macular pucker: to peel or not to peel the internal limiting membrane? A microperimetric response. Retina. 2015;35:498–507.
31. Clark A, Balducci N, Pichi F, et al. Swelling of the arcuate nerve fiber layer after internal limiting membrane peeling. Retina. 2012;32(8):1608–1613.
32. Scupola A, Grimaldi G, Abed E, et al. Arcuate nerve fiber layer changes after internal limiting membrane peeling in idiopathic epiretinal membrane. Retina. 2018;38(9):1777–1785.
33. Kinoshita T, Imaizumi H, Okushiba U, et al. Time course of changes in metamorphopsia, visual acuity, and OCT parameters after successful epiretinal membrane surgery. Invest Ophthalmol Vis Sci. 2012;53(7):3592–3597.
34. Brito PN, Gomes NL, Vieira MP, et al. Possible role for fundus autofluorescence as a predictive factor for visual acuity recovery after epiretinal membrane surgery. Retina. 2014;34(2):273–280.
35. Jonna G, Thompson I, Mendel T, Kim S. Five-year functional outcomes after epiretinal membrane surgery: a prospective, controlled study. Retina. 2019;39(12):2326–2331.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.