Back to Journals » Clinical Interventions in Aging » Volume 13
AKI in the very elderly patients without preexisting chronic kidney disease: a comparison of 48-hour window and 7-day window for diagnosing AKI using the KDIGO criteria
Received 17 January 2018
Accepted for publication 22 March 2018
Published 20 June 2018 Volume 2018:13 Pages 1151—1160
DOI https://doi.org/10.2147/CIA.S162899
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Qinglin Li,1 Meng Zhao,2 Xiaodan Wang1
1Department of Health Care, Nanlou Division, Chinese PLA General Hospital, National Clinical Research Center for Geriatric Diseases, Beijing, China; 2Department of Clinical Data Repository, Chinese PLA General Hospital, Beijing, China
Objectives: To compare the differences between the Kidney Disease Improving Global Outcomes (KDIGO) criteria of the 48-hour window and the 7-day window in the diagnosis of acute kidney injury (AKI) in very elderly patients, as well as the relationship between the 48-hour and 7-day windows for diagnosis and 90-day mortality.
Patients and methods: We retrospectively enrolled very elderly patients (≥75 years old) from the geriatrics department of the Chinese PLA General Hospital between January 2007 and December 2015. AKI patients were divided into 48-hour and 7-day groups by their diagnosis criteria. AKI patients were divided into survivor and nonsurvivor groups by their outcomes within 90 days after diagnosis of AKI.
Results: In total, 652 patients were included in the final analysis. The median age of the cohort was 87 (84–91) years, the majority (623, 95.6%) of whom were male. Of the 652 AKI patients, 334 cases (51.2%) were diagnosed with AKI by the 48-hour window for diagnosis, while 318 cases (48.8%) were by the 7-day window for diagnosis. The 90-day mortality was 42.5% in patients with 48-hour window AKI and 24.2% in patients with 7-day window AKI. Kaplan–Meier curves showed that 90-day mortality was lower in the 7-day window AKI group than in the 48-hour window AKI group (log rank: P<0.001). Multivariate analysis by the Cox model revealed that 48-hour window for diagnosis hazard ratio (HR=1.818; 95% CI: 1.256–2.631; P=0.002) was associated with higher 90-day mortality.
Conclusion: The 90-day mortality was higher in 48-hour window AKI than in 7-day window AKI in very elderly patients. The 48-hour KDIGO window definition may be less sensitive. The 48-hour KDIGO window definition is significantly better correlated with subsequent mortality and is, therefore, still appropriate for clinical use. Finding early, sensitive biomarkers of kidney damage is a future direction of research.
Keywords: acute kidney injury, AKI diagnosis time, very elderly, short-term mortality
Introduction
Acute kidney injury (AKI), previously termed acute renal failure (ARF), is a common clinical critical disorder among elderly patients.1 AKI has been recognized as a surrogate marker of the severity of illness. This complex acute syndrome is closely associated with both short- and long-term mortality and length of hospital stay, and it is a predictor of chronic kidney disease (CKD).2–5 There has been no uniform standard for the definition and diagnosis of AKI since 10 years ago,6 resulting in great discrepancies in the reported incidences of AKI. This heterogeneity of the data has made the comparison of various published studies focusing on AKI difficult and in many cases impossible. Since 2004, at least three proposals have been put forth to define and stage AKI. The RIFLE (Risk, Injury, Failure, Loss, and End-Stage Renal Disease [ESRD]) criteria,7 the first consensus definition, have been studied in a number of settings and have been validated by showing that a stepwise relationship exists between AKI severity and mortality. The Acute Kidney Injury Network (AKIN) criteria modified RIFLE by incorporating an absolute increase in serum creatinine (SCr) after the finding that small increases in SCr of as little as 0.3 mg/dL (26.5 μmol/L) and a time constraint of 48 hours for the diagnosis of AKI were of prognostic significance.8 By considering the changes in SCr values over the first 48 hours, the sensitivity and specificity to detect AKI were increased in the AKIN criteria. However, AKIN criteria could still underestimate AKI in patients for whom the increase in SCr is slow. The current definition by Kidney Disease Improving Global Outcomes (KDIGO) is similar to the AKIN definition, but the time frame is extended from 48 hours to 7 days.9 An elevation of the SCr level exceeding 26.5 μmol/L within 48 hours, an increase in SCr to 1.5 times the baseline value, which is known or presumed to have occurred within 7 days before, or a urine volume of <0.5 mL·kg−1·h−1 for 6 hours was defined as AKI. The KDIGO criteria evaluate baseline SCr and, therefore, can detect AKI in patients with slow increases in SCr. These criteria provide a simple standardized method of categorizing AKI, and they have been assessed in several investigations.10–14 However, the clinical implications of a 48-hour or 7-day window for diagnosing AKI in very elderly patients are unknown.
Therefore, the goals of the present study were as follows: 1) compare the rates using 48-hour and 7-day windows for diagnosis of AKI; 2) address the key clinical differences between the 48-hour or 7-day diagnostic window AKI; and 3) examine the effects of 48-hour and 7-day window diagnosis of AKI on short-term mortality.
Patients and methods
We retrospectively analyzed clinical data from very elderly patients (≥75 years of age) who were admitted to the Geriatrics Department of the Chinese PLA General Hospital in Beijing, China, between January 1, 2007, and December 31, 2015. The study design was approved by the Clinical Ethics Committee of the Chinese PLA General Hospital, and each patient provided informed written consent. AKI patients were divided into 48-hour and 7-day diagnostic window groups based on the KDIGO criteria. The patients were divided into survivor and nonsurvivor groups by their outcomes within 90 days after AKI diagnosis.
AKI was diagnosed only by the SCr criterion of the 2012 KDIGO criteria.9 Stage 1 was defined by an increase in SCr of 50%–100% within 7 days or to 26.5 μmol/L or even greater than baseline within 48 hours; stage 2 was defined by an increase of SCr in 100%–200% from baseline; and stage 3 was defined by a 200% or more increase in SCr, an increase to 353.6 μmol/L or more, or initiation of renal replacement therapy. We noted that the analyzed variables included baseline data and laboratory data. The baseline SCr level was the most recent stable measurement obtained within 3 months prior to admission with AKI.15,16 The peak SCr was the highest SCr level reached during the episode. Estimated glomerular filtration rates (eGFRs) were calculated by the Chronic Kidney Disease Epidemiology Collaboration.17 Oliguria was defined as urinary output <400 mL/24 hours.
We excluded patients younger than 75 years, those with previously diagnosed CKD,18 those who stayed in the hospital for <48 hours, those who underwent fewer than two SCr examinations, those with missing or incomplete medical histories, and those who died early within 48 hours after admission.
Statistical analysis
Continuous variables were presented as mean ± SD, or the median (25%–75% interquartile range), depending on the variable distribution. Discrete variables are presented as counts or percentages. Statistical analyses were performed using SPSS version 17.0 for Windows (SPSS Inc., Chicago, IL, USA). Between-group comparisons were made using Student’s t-tests or Mann–Whitney U-test for continuous variables and with Pearson’s chi-squared or Fisher’s exact tests for categorical variables. Survival curves were estimated by the Kaplan–Meier product-limit method and compared by the Mantel (log-rank) test. Prognostic factors of survival were identified by the use of the Cox proportional hazards regression model. A P-value <0.05 was considered to reflect statistical significance.
Results
Study population
Between January 2007, and December 2015, a total of 3,464 very elderly patients were admitted to the Geriatrics Department, and 668 developed AKI during hospitalization.
Of these patients, 10 were excluded for hospital stays <48 hours and six for missing the data required for this study, resulting in 652 AKI patients who were suitable for the final evaluation. According to the KDIGO definition, 51.2% (334/652) of the elderly patients diagnosed as having AKI met the 26.5 μmol/L absolute increase criterion, whereas 48.8% (318/652) of the AKI cases were diagnosed based on a 50% increase in SCr over 7 days without meeting the 26.5 μmol/L absolute increase criterion. The overall 90-day mortality was 33.6% (219/652). The study flow chart is presented in Figure 1.
  | Figure 1 Flow chart of patient inclusion and exclusion. |
Demographic characteristics of AKI patients
The baseline characteristics of the 652 AKI patients are shown in Table 1. The median age of the cohort was 87 years. The median baseline SCr level was 73.0 μmol/L, and the baseline eGFR was 78.4 mL/min/1.73 m2. Using the KDIGO criteria, 308 patients (47.2%) had stage 1 AKI, 164 (25.2%) had stage 2, and 171 (26.2%) had stage 3. The predominant comorbidities were coronary disease in 505 (77.5%), hypertension in 485 (74.4%), COPD in 454 (69.6%), and diabetes mellitus in 234 (35.8%). Overall, 35 (5.4%) had oliguria, and 9 (1.4%) of the stage 3 patients required acute dialysis.
Clinical characteristics associated with 48-hour or 7-day diagnostic window AKI
As shown in Table 1, comparison of the elderly patients with 48-hour or 7-day diagnostic window AKI indicated no significant differences in age (median age: 87 vs 87 years, P=0.388) or gender (94.3% vs 96.9%, P=0.115). Similarly, no significant differences were found for preexisting comorbidities (coronary disease P=0.488, hypertension P=0.328, COPD P=0.942, and diabetes mellitus P=0.069) or body mass index (BMI) level (23.0±3.2 kg/m2 vs 23.1±3.1 kg/m2, P=0.715). The median SCr level (70 μmol/L vs 76 μmol/L, P<0.001) and eGFR (80.1 mL/min/1.73 m2 vs 77.2 mL/min/1.73 m2, P<0.001) at baseline were significantly different between the two groups. Patients with 48-hour window AKI were more frequently treated surgically (9.3% vs 4.4%, P=0.014) and suffered less often from nephrotoxicity (6.6% vs 17.6%, P<0.001). They also had significantly higher peak SCr (152.1 μmol/L vs 139.4 μmol/L, P=0.017) levels, as well as higher BUN (13.9 mmol/L vs 11.5 mmol/L, P=0.005) at the time of AKI diagnosis, compared with patients with 7-day window AKI. Accordingly, patients with 48-hour window AKI were more likely to require mechanical ventilation (MV, 45.5% vs 27.7%, P<0.001) and to have the presence of low mean arterial pressure (MAP, 77±15 mmHg vs 80±13 mmHg, P=0.007) and oliguria (7.2% vs 3.5%, P=0.035). Lower prealbumin levels (168 vs 197 g/L, P<0.001) and hypoalbuminemia (33.5±5.3 g/L vs 35.3±5.5 g/L, P<0.001) were more common in patients with 48-hour window AKI. Patients with 48-hour window AKI presented higher mortality rates (42.5% vs 24.2%, P<0.001) and more frequently exhibited stage 2 and 3 AKI (25.7% vs 24.5%, 35.6% vs 19.2%); there were fewer patients with stage 1 AKI (38.6% vs 56.3%, P<0.001; Figure 2).
  | Figure 2 Forty-eight-hour window and 7-day window AKI at different KDIGO stages in patients with AKI. |
Influence of 48-hour or 7-day window AKI on patient short-term outcomes
As shown in Table 1, the 90-day mortality was 42.5% for patients with 48-hour window AKI and 24.2% for patients with 7-day window AKI (P<0.001). Dialysis was necessary in 2.1% of the 48-hour window AKI patients, compared to 0.6% of the 7-day window AKI (P=0.204) patients. Kaplan–Meier curves showed significant differences in 90-day mortality between the two groups (log rank P<0.001; Figure 3). Within the AKI groups, the 90-day mortality was better in the 7-day window AKI group than in the 48-hour window AKI group (log rank P<0.001; Figure 3). The separation of the curves continued throughout the follow-up period, with an increased probability of death during the follow-up with increasing days of AKI diagnosis (Figure 4).
  | Figure 3 Kaplan–Meier survival curves according to 48-hour window and 7-day window AKI (log-rank test: P<0.001). |
  | Figure 4 Kaplan–Meier survival curves according to different time windows for diagnosis of AKI (log-rank test: P<0.001). |
Table 2 also shows the relationships between the AKI stage and the short-term outcomes: increasing AKI severity was associated with significantly higher 90-day mortality – 8.7% in stage 1, 30.1% in stage 2, and 61.2% in stage 3. Advanced AKI stage was associated with worse health outcomes among patients (P<0.001 for the three stages).
For both classification systems, 90-day mortality increased in accordance with staging (both log rank P<0.001; Figures 5 and 6). For the 48-hour time window AKI group, 8.5% (12/142) had stage 1, 28.2% (40/142) had stage 2, and 63.4% (90/142) had stage 3; for the 7-day window AKI group, 9.1% (7/77) had stage 1, 33.8% (26/77) had stage 2, and 57.1% (44/77) had stage 3 (data not shown). Accordingly, the prevalence of 48-hour window AKI was significantly higher in the death group (64.8% vs 35.2%, P<0.001; Table 2).
Multivariate analysis by the Cox model revealed that AKI diagnosis time (≤48 hours) was associated with higher 90-day mortality (Table 3). The other independent risk factors for 90-day mortality included low BMI (HR=0.928; 95% CI: 0.886–0.973; P=0.002), low MAP (HR=0.969; 95% CI: 0.959–0.979; P<0.001), low prealbumin level (HR=0.948; 95% CI: 0.920–0.977; P<0.001), low albumin level (HR=0.962; 95% CI: 0.930–0.995; P=0.025), infection (HR=1.374; 95% CI: 1.027–1.840; P=0.033), oliguria (HR=2.069; 95% CI: 1.341–3.192; P=0.001), BUN level (HR=1.027; 95% CI: 1.015–1.038; P<0.001), magnesium level (HR=2.485; 95% CI: 1.351–4.570; P=0.003), and more severe AKI stage (stage 2: HR=4.035; 95% CI: 2.381–6.837; P<0.001; stage 3: HR=7.184; 95% CI: 4.301–11.997; P<0.001).
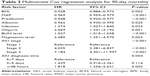  | Table 3 Multivariate Cox regression analysis for 90-day mortality |
Discussion
In our study, we performed a retrospective cohort study of elderly patients to describe the epidemiology of 48-hour and 7-day time windows for diagnosing AKI and the associated outcomes. Although the KDIGO criteria evaluate baseline SCr, and the diagnostic window was increased to 48 hours to enhance sensitivity and can detect AKI in patients with a slow increase in SCr within 7 days, there is no information regarding the incidence and clinical significance of the 48-hour or 7-day window for diagnosing AKI in very elderly patients. Whether AKI patients with the 7-day window for diagnosis were associated with short-term prognosis or not has not yet been reported.
ARF and AKI have traditionally been used to describe an abrupt decrease in renal function. Many clinical studies of AKI have been published using different criteria for the diagnosis and classification of AKI (KDIGO, RIFLE, and AKIN).10,14,15 The use of the three systems is an improvement from the previous use of >30 different classification systems.6 Recently, Fujii et al reported the epidemiology of AKI in hospitalized patients using the KDIGO definition and compared it with the two other previous consensus definitions in a single-center, retrospective, observational study.10 Here, we additionally report a study comparing the two sets of criteria in very elderly patients. In our population, more than half of the measurements were performed with intervals of <48 hours (51.2%), which was close to the value reported in the work by Fujii et al (51.0%).10 Additionally, we found that a 48-hour window for diagnosing AKI was associated with higher 90-day mortality (P=0.002), which was not observed in a previous report.10
The greater sensitivity of the KDIGO classification might allow AKI episodes to be recognized earlier and might make a reduced nonrecognition rate of AKI possible.9 The KDIGO criteria define AKI based on changes in SCr “calling for at least two measurements over a 48-hour period” or when “presumed to have occurred within the prior 7 days”. However, in real clinical settings, not all patients undergo routine daily SCr measurements because many clinicians rely on blood tests as needed and not daily. The proportion of patients with two or more SCr measurements during hospitalization ranged from 25% to 30% in previous reports, which is much lower than the figure reported in developed countries (63.2%–67.6%).19–21 Even for patients with two SCr examinations in 7 days, AKI would be missed in 48% of the patients.20 Therefore, some patients with AKI could be misclassified as not having AKI.22 One explanation might be the definition of AKI, which is neither uniformly known nor accepted in the non-nephrologic community. Although the KDIGO criteria provide a 48-hour or 7-day window for diagnosis, these criteria are not commonly used in real clinical settings.
In this study, nearly 49% of the measurements were performed with intervals of more than 48 hours by baseline SCr values, so determining baseline SCr values was important for diagnosing AKI and determining AKI staging.23,24 In most studies, there was no baseline SCr available prior to admission – a requirement for accurately defining AKI. Several methods have been proposed to address this conundrum.9 1) The use of admission SCr value has been proposed because many patients already have AKI before admission, and the method of using SCr level at hospital admission could have been modified by the acute illness prompting hospitalization and is unlikely to be representative of the true baseline state. In addition, admission SCr values might be affected by the hemodynamics or metabolic status at the time of presentation; thus, it is inappropriate to consider this level a baseline for renal function for study patients.25 2) The lowest SCr level measured during the hospital stay also has a number of disadvantages. First, this measurement is, by definition, a retrospective baseline (the patient’s hospitalization must have ended to identify the nadir value; therefore, this measurement cannot be used in daily clinical practice). Second, the nadir SCr value is likely to be less than the true baseline level, thereby overestimating the incidence of AKI, especially for elderly patients with malnutrition.26 3) A back-calculation of baseline creatinine using the Modification Diet in Renal Disease equation, assuming a baseline eGFR of 75 mL/min/1.73 m2, could be considered. However, such an assumption might be at risk of overestimating the AKI incidence, especially for patients with preexisting CKD, which would be common in elderly patients.27 4) Finally, premorbid SCr values measured longer than 7 days before events could be useful. We opted to use premorbid SCr measurements within 3 months before AKI to enhance the accuracy of detecting AKI in this elderly cohort. Multiple studies have validated the utility of this approach. Chao et al found that SCr measured 90 days before admission exhibited a very high degree of agreement with reference baseline SCr values.16
In this study, the two diagnostic criteria for AKI patients’ 90-day mortality were 42.5% for patients with 48-hour window diagnosis of AKI and 24.2% for patients with 7-day window diagnosis of AKI. Multivariate analysis by Cox showed that early and small changes in SCr (48-hour window for diagnosis) were independent risk factors for 90-day mortality in the elderly, and an SCr increase of more than 26.5 μmol/L was associated with a hazard ratio for death of 1.818 (95% CI: 1.256–2.631). The possible explanations are as follows: including the adverse effects of decreased renal function, such as volume overload, anemia, uremia, acidosis, electrolyte disturbances, and increased risk of infections.9 Other possible reasons in the very elderly include MV-related complications, poor nutritional status, and more patients in KDIGO stage 3.22 1) MV is a common and important intervention in the elderly. MV affects systemic and renal blood flow and can cause hypotension and fluid reactive shock, affecting renal perfusion by decreasing GFR and reducing cardiac output and stimulating hormonal and sympathetic pathways, causing or promoting the development of AKI.28,29 2) AKI stage is associated with worse prognosis of AKI patients,12,20,30 SCr increase is a marker for the disease severity, and an acute increase in SCr within 48 hours can indicate more loss of renal function, whereas more severe AKI stages suggest a worse prognosis, which can indicate that, although the patient received active treatment earlier, if the severity of elderly AKI still progresses to KDIGO stage 3, mortality would increase significantly. 3) Malnutrition (low serum albumin and low prealbumin) is a common problem in elderly patients. Several studies of the association between mortality and nutritional status have found that preexisting malnutrition is associated with poor outcomes in AKI patients.31,32 A study of serum prealbumin in elderly patients with AKI found that the proportion with serum prealbumin <200 g/L with 90-day mortality was 48.9%, and the mortality with ≥200 g/L was only 19.7%.33 4) Although the time of the 48-hour window for diagnosis is earlier than the 7-day window, it does not mean that kidney injury occurs early because the SCr level alone is a relatively late and imprecise biomarker of kidney dysfunction, which can also lead to a delayed diagnosis, especially in the elderly population. Therefore, finding early, sensitive, and reliable biomarkers of kidney injury is a future direction of research.34
Strengths and limitations
Strengths of this study include the elderly age of the sample, the use of a consensus definition for AKI diagnosis and stages, and baseline SCr, being available in the entire sample of included patients. On the other hand, limitations of this study should be noted. First, this was a single-center retrospective work, so the results may not be immediately applicable to other hospitalized patients. Second, we analyzed data from a veteran’s hospital, and because most patients were retired elderly males and fewer females are treated in our hospital. Thus, biased results may be unavoidable. Third, the definition of AKI in our analysis was based on SCr levels. We chose not to use the urine output criteria because these data were incomplete.
Conclusion
The 90-day mortality was higher in 48-hour window AKI than in 7-day window AKI in very elderly patients. The 48-hour KDIGO window definition may be less sensitive. The 48-hour KDIGO window definition is significantly better correlated with subsequent mortality and is, therefore, still appropriate for clinical use. Currently, SCr combined with urine output remains the cornerstone for diagnosing and classifying AKI; neither of them is perfect as an index for both defining and classifying AKI because cell damage occurs earlier than the increase in SCr and decrease in urine output. Therefore, finding early, sensitive, and reliable biomarkers of kidney injury is a future direction of research.
Acknowledgments
This manuscript was edited for English language by American Journal Experts (AJE). This study was funded by grants from the National Natural Science Foundation of China (No. 81370452).
Disclosure
The authors report no conflicts of interest in this work.
References
Yokota LG, Sampaio BM, Rocha E, Balbi AL, Ponce D. Acute kidney injury in elderly intensive care patients from a developing country: clinical features and outcome. Int J Nephrol Renovasc Dis. 2017;10:27–33. | ||
Pannu N, James M, Hemmelgarn B, Klarenbach S; Alberta Kidney Disease Network. Association between AKI, recovery of renal function, and long-term outcomes after hospital discharge. Clin J Am Soc Nephrol. 2013;8(2):194–202. | ||
Chawla LS, Kimmel PL. Acute kidney injury and chronic kidney disease: an integrated clinical syndrome. Kidney Int. 2012;82(5):516–524. | ||
Rewa O, Bagshaw SM. Acute kidney injury-epidemiology, outcomes and economics. Nat Rev Nephrol. 2014;10(4):193–207. | ||
Nisula S, Kaukonen KM, Vaara ST, et al; FINNAKI Study Group. Incidence, risk factors and 90-day mortality of patients with acute kidney injury in Finnish intensive care units: the FINNAKI study. Intensive Care Med. 2013;39(3):420–428. | ||
James M, Bouchard J, Ho J, et al. Canadian society of nephrology commentary on the 2012 KDIGO clinical practice guideline for acute kidney injury. Am J Kidney Dis. 2013;61(5):673–685. | ||
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P; Acute Dialysis Quality Initiative Workgroup. Acute renal failure – definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8(4):R204–R212. | ||
Mehta RL, Kellum JA, Shah SV, et al; Acute Kidney Injury Network. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11(2):R31. | ||
Eknoyan G, Lameire N, Eckardt K, Kasiske B. Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:1–138. | ||
Fujii T, Uchino S, Takinami M, Bellomo R. Validation of the kidney disease improving global outcomes criteria for AKI and comparison of three criteria in hospitalized patients. Clin J Am Soc Nephrol. 2014;9(5):848–854. | ||
Bastin AJ, Ostermann M, Slack AJ, Diller GP, Finney SJ, Evans TW. Acute kidney injury after cardiac surgery according to risk/injury/failure/loss/end-stage, Acute Kidney Injury Network, and kidney disease: improving global outcomes classifications. J Crit Care. 2013;28(4):389–396. | ||
Zeng X, McMahon GM, Brunelli SM, Bates DW, Waikar SS. Incidence, outcomes, and comparisons across definitions of AKI in hospitalized individuals. Clin J Am Soc Nephrol. 2014;9(1):12–20. | ||
Machado MN, Nakazone MA, Maia LN. Acute kidney injury based on KDIGO (Kidney Disease Improving Global Outcomes) criteria in patients with elevated baseline serum creatinine undergoing cardiac surgery. Rev Bras Cir Cardiovasc. 2014;29(3):299–307. | ||
Luo X, Jiang L, Du B, Wen Y, Wang M, Xi X; Beijing Acute Kidney Injury Trial (BAKIT) workgroup. A comparison of different diagnostic criteria of acute kidney injury in critically ill patients. Crit Care. 2014;18(4):R144. | ||
Pan HC, Chien YS, Jenq CC, et al. Acute kidney injury classification for critically ill cirrhotic patients: a comparison of the KDIGO, AKIN, and RIFLE classifications. Sci Rep. 2016;6:23022. | ||
Chao CT, Tsai HB, Wu CY, et al. The severity of initial acute kidney injury at admission of geriatric patients significantly correlates with subsequent in-hospital complications. Sci Rep. 2015;5:13925. | ||
Levey AS, Stevens LA, Schmid CH, et al; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. | ||
Levin A, Stevens PE. Summary of KDIGO 2012 CKD guideline: behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014;85(1):49–61. | ||
Yang L, Xing G, Wang L, et al; ISN AKF 0by25 China Consortiums. Acute kidney injury in China: a cross-sectional survey. Lancet. 2015;386(10002):1465–1471. | ||
Xu X, Nie S, Liu Z, et al. Epidemiology and clinical correlates of AKI in Chinese hospitalized adults. Clin J Am Soc Nephrol. 2015;10(9):1510–1518. | ||
Lu R, Mucino-Bermejo MJ, Armignacco P, et al. Survey of acute kidney injury and related risk factors of mortality in hospitalized patients in a third-level urban hospital of Shanghai. Blood Purif. 2014;38(2):140–148. | ||
Li Q, Zhao M, Wang X. The impact of transient and persistent acute kidney injury on short-term outcomes in very elderly patients. Clin Interv Aging. 2017;12:1013–1020. | ||
Thongprayoon C, Cheungpasitporn W, Srivali N, Ungprasert P, Kittanamongkolchai W, Kashani K. The impact of fluid balance on diagnosis, staging and prediction of mortality in critically ill patients with acute kidney injury. J Nephrol. 2016;29(2):221–227. | ||
Thongprayoon C, Cheungpasitporn W, Kittanamongkolchai W, et al; Spring Clinical Meetings. Optimum methodology for estimating baseline serum creatinine for the acute kidney injury classification. Nephrology (Carlton). 2015;20(12):881–886. | ||
Choi JS, Kim YA, Kim MJ, et al. Relation between transient or persistent acute kidney injury and long-term mortality in patients with myocardial infarction. Am J Cardiol. 2013;112(1):41–45. | ||
Siew ED, Matheny ME, Ikizler TA, et al. Commonly used surrogates for baseline renal function affect the classification and prognosis of acute kidney injury. Kidney Int. 2010;77(6):536–542. | ||
Pickering JW, Endre ZH. Back-calculating baseline creatinine with MDRD misclassifies acute kidney injury in the intensive care unit. Clin J Am Soc Nephrol. 2010;5(7):1165–1173. | ||
Broden CC. Acute renal failure and mechanical ventilation: reality or myth? Crit Care Nurse. 2009;29(2):62–75; quiz 76. | ||
Koyner JL, Murray PT. Mechanical ventilation and lung-kidney interactions. Clin J Am Soc Nephrol. 2008;3(2):562–567. | ||
Sutherland SM, Byrnes JJ, Kothari M, et al. AKI in hospitalized children: comparing the pRIFLE, AKIN, and KDIGO definitions. Clin J Am Soc Nephrol. 2015;10(4):554–561. | ||
Joannidis M, Wiedermann CJ; Springer Berlin Heidelberg. Hypoalbuminemia as a risk factor for acute kidney injury. Annu Update Intensive Care Emerg Med. 2011;1:233–241. | ||
Wiedermann CJ, Wiedermann W, Joannidis M. Hypoalbuminemia and acute kidney injury: a meta-analysis of observational clinical studies. Intensive Care Med. 2010;36(10):1657–1665. | ||
Wen J, Cheng Q, Zhao J, et al. Hospital-acquired acute kidney injury in Chinese very elderly persons. J Nephrol. 2013;26(3):572–579. | ||
Chao CT, Tsai HB, Lin YF, Ko WJ. Acute kidney injury in the elderly: only the tip of the iceberg. J Clin Gerontol Geriatr. 2014;5(1):7–12. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.