Back to Journals » Patient Preference and Adherence » Volume 11
Adherence to treatment and evaluation of disease and therapy knowledge in Lebanese hypertensive patients
Authors Abbas H , Kurdi M, Watfa M , Karam R
Received 23 May 2017
Accepted for publication 12 October 2017
Published 28 November 2017 Volume 2017:11 Pages 1949—1956
DOI https://doi.org/10.2147/PPA.S142453
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Johnny Chen
Hanine Abbas,1 Mazen Kurdi,1 Myriam Watfa,2 Rita Karam1–3
1Department of Chemistry and Biochemistry, Faculty of Science, Lebanese University, 2Quality Assurance of Pharmaceutical Products Department, Lebanese Ministry of Public Health, 3Pharmacology Department, Faculty of Medical Sciences, Lebanese University, Beirut, Lebanon
Background: Adherence to treatment, healthy lifestyle, physical activities, smoking, diet, and salt intake are important factors to control for an effective decrease in blood pressure (BP) values for patients diagnosed with essential hypertension (HT). The aim of this work was to study the adherence to antihypertensive treatment and factors predicting this behavior in Lebanese patients. In addition, we evaluated the extent of patient’s knowledge and perceptions about HT, risk factors, and medication side effects.
Methods: The cross-sectional study was conducted between May and September 2015 among 249 participants randomly recruited from community and hospital pharmacies (56.6%), private cardiology clinics (37%), and outpatient clinics located in hospitals (6.4%) in Baabda region of Lebanon. The questionnaire was prepared after reviewing published literature. Data were collected by trained and certified interviewers and analyzed by Statistical Package for the Social Sciences program. p-value less than 0.05 was considered to determine the statistical significance.
Results: Among the 249 patients interviewed, 48% were females with a mean age of 62±17.2 years. Overweight and obesity was declared in 42.2% and 35.3%, respectively. Only 52.6% of participants reported visiting their physicians for regular checkups, and 72% claimed checking their BP routinely at home. Awareness of complications related to HT was very high (97%). However, our results showed that 89.2% of the participants were found to be adherent to treatment, and forgetfulness was cited as the main reason for non-adherence to therapy. Only health coverage showed statistical significance (p=0.01) between adherent and non-adherent participants.
Conclusion: A better communication between patients and their physicians, the use of a special container for medication packaging, and reminder to refill prescriptions are important parameters to enhance adherence to treatment. HT can be better managed if an educational system is implemented to increase awareness.
Keywords: Lebanon, hypertension, treatment, compliance, adherence, awareness
Introduction
High blood pressure (BP) is estimated to cause 7.5 million deaths worldwide, about 12.8% of the total deaths, and it accounts for 57 million disability-adjusted life years (DALYS), or 3.7% of the total DALYS.1 The overall prevalence of increased BP in people 25 years or older was about 40% in 2008.1 In Lebanon, a population-based study conducted in 2005 revealed that the overall prevalence of declared hypertension (HT) was 23.1%.2 In a more recent study conducted in 2015, the prevalence, awareness, treatment, and control (among treated hypertensive) rates of HT were 36.9%, 53%, 48.9%, and 54.2%, respectively. Overall, only 27% of patients with HT had their BP under control.3 Based on recommendations of the Joint National Committee 8, HT is defined as systolic blood pressure (SBP) of 140 mmHg or higher, or diastolic blood pressure (DBP) of 90 mmHg or higher.4 The first approach in treating HT is through lifestyle modifications. A Dietary Approach to Stop Hypertension (DASH) diet is highly recommended. BP control with the DASH diet involves more than just the traditional low salt or low sodium diet advice.5 It is based on a dietary intake plan proven to lower BP, which is rich in fruits, vegetables, and low-fat or nonfat dairy. The plan emphasizes whole grains and contains less refined grains compared with a typical diet and is rich in potassium, magnesium, calcium, and fiber.5 Moreover, healthy lifestyles such as a reasonably balanced diet intake, undertaking regular physical exercise, and non-smoking are among the most important preventive measures.6
Despite the availability of effective treatments, studies have shown that in many countries less than 25% of patients treated for HT achieve optimum BP.6 In a study conducted in 20153 among treated hypertensive patients, the authors conclude that HT is prevalent in Lebanon and its overall control is low.3 Suboptimal or poor adherence has been identified as the main cause of failure to control HT. It also reduces the effectiveness of medications and has been highlighted as a significant obstacle in achieving the optimal clinical benefit.7
The participants at the World Health Organization Adherence Meeting held in June 2001 adopted the following definition of adherence to long-term therapy: “The extent to which a person’s behavior-taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider”.8
Although there is no golden standard for measuring adherence behavior, there are various methods for assessing adherence to medications. The most frequently used methods include patient self-report or questionnaire.9 The economic evaluation of non-adherence requires the recognition of the associated costs and outcomes. Non-adherence implies a cost due to the occurrence of the undesired effects that the suggested regimen tries to minimize. In terms of outcomes, non-adherence results in increased clinical risk and therefore in increased morbidity and mortality.10 Based on this, our study aims to evaluate the antihypertensive medication adherence in Lebanese hypertensive patients using a well-structured questionnaire and the factors predicting this behavior and to assess the extent of patient’s knowledge and perceptions about the disease, risk factors, and medication side effects.
Methods
The cross-sectional study was conducted between May and September 2015 among a sample of 249 adults with HT. The participants were recruited randomly from patients visiting outpatient clinics located in hospitals, community and hospital pharmacies and from private cardiology clinics located in Baabda, in the Governorate of Mount Lebanon. Eligible participants were Lebanese adults diagnosed with primary (essential) HT treated with at least one antihypertensive medication. The study excluded patients with secondary HT, pregnant women, patients with a psychiatric illness or mental impairment, or patients unable to give informed consent. In addition, untreated hypertensive patients taking no medication and non-Lebanese subjects were also excluded.
The study protocol was reviewed and approved by the Institutional Review Board of Lebanese University. All participants were provided with clear and easy to understand information about the research project in order to allow them to make an informed and voluntary decision about whether or not to participate. In accordance with the privacy rule of the Health Insurance Portability and Accountability Act and the declaration of Helsinki, a written consent form was signed by each participant to indicate agreement to participate in this study. The data was collected by interviewers who had passed an exam offered by the National Institutes of Health office for extramural research related to the Protection of Human Research Participants. Standardized materials along with identical equipment were used by all trained interviewers. Telephone appointments were scheduled with cardiologists for the purpose of interviewing hypertensive patients.
A well-structured questionnaire was used to address the study objective. Information pertaining to demographic, education, lifestyle, medication and adherence, awareness, BP measurement, and family history of HT was collected for each subject.
BP readings were measured using an automated BP machine (Omron HEM-RML 31) while the participants were in the resting state for 8 minutes and in seated position. Height was measured to the nearest 0.1 cm with a non-stretchable measuring tape. Weight was measured to the nearest 0.1 kg with a digital scale (Omron HBF-500). Height and weight were measured with clothing on, but no shoes. Body mass index (in kg/m2) was calculated based on height and weight readings.
The survey was conducted in Baabda south of Beirut where the population was estimated at 500,000 inhabitants. A minimum sample size of 249 participants is required to give a 95% confidence level with a confidence interval of 6.2%. These data were entered and analyzed by Statistical Package for the Social Sciences program version 20. Qualitative data were represented in frequency and percentage, while quantitative data were represented as mean ± standard deviation. Bivariate analysis of different variables with the adherence to medication was performed using the chi-square test. A value of p<0.05 was considered statistically significant.11
Results
Sociodemographic characteristics
Baseline demographic criteria of enrolled participants are reported in Table 1. The mean age of participant was 62±17.2 years. The study involved 129 (51.8%) males and 120 (48.2%) females with no significant age difference between males and females (p=0.797). Randomly selected, 141 (56.6%) participants were from pharmacies, 92 (37%) from private cardiology clinics, and 16 (6.4%) from hospitals. Survey respondents were predominantly married (214 [85.54%]) and only 20.5% of the sample population were employed. Eighty percent of the participants did not reach high school (Table 1).
  | Table 1 Sociodemographic characteristics |
BP and body dimensions
The mean SBP was 138.95±18.35 mmHg and DBP was 87.2±7.13 mmHg showing an uncontrolled BP among participants.
The mean weight of participants was 80.94±14.95 kg and the mean height was 168.18±8.907 cm. Overweight and obesity were declared in 42% and 35.3%, respectively (Table 2).
  | Table 2 Blood pressure and body dimensions |
General health information and illness perception
Among the participants analyzed, 37% reported that they were first diagnosed with HT within the past 5 years. In addition, 84.7% of participants knew their BP reading when they were diagnosed with HT for the first time, and the SBP in 75% of them ranged between 160 and 200 mmHg. Knowledge of the underlying cause for the high BP was reported in 73% of the participants. It is revealing to know that 61% of the participants were hospitalized for uncontrolled BP. HT was accompanied with other cardiovascular comorbidities in 35.74% of cases, among which 20.5% appeared before being diagnosed with HT (Table 3).
  | Table 3 General health information and illness perceptions |
Medication information and adherence patterns
Sixty-seven percent of the participants were on combination treatment for HT. The most widely prescribed type of antihypertensive medication was beta-blocker, which was used alone or in combination by 53% of the participants. It is noted that 48% of the participants declared changing their antihypertensive medications during the last year of treatment for uncontrolled BP and for non-tolerated side effects in 53% and 41% of the cases, respectively. Surprisingly, only 11.6% of participants were self-medicated mainly with non-steroidal anti-inflammatory drugs. Regarding the alternative HT treatment, 68% of the participants were supplement users. Among this group, 42% used OMEGA-3, co-Q10, and vitamin D for controlling HT, and 37% used DASH diet, which is considered as a new supplement food type. However, physical activities were reported by only 11% of participants.
With regard to adherence, 85% of the participants were taking their antihypertensive medications as prescribed by their doctors. Thirty-seven (15%) participants did not adhere to the prescribed medications. Among these participants, 33 (89.2%) related non-adherence to mere forgetfulness (Table 4).
  | Table 4 Medication information and adherence patterns |
BP information and awareness
More than half of the participants (52.6%) reported visiting their physicians for regular checkups, and 28% visited their doctors every 3–6 months for follow-up. As recommended by their physicians, 72% checked their BP at home. The last BP readings ranged between 150 and 180 mmHg in 35% of participants, which is considered high, and 48.6% of the participants stated that their last BP reading was done 2 weeks earlier. In addition, 41.4% of participants claimed to have occasional headaches as a symptom of uncontrolled BP. The study also showed that 97% of the participants were aware that non-compliance may affect their health status. However, 96.4% of the study group did not use a special container for medication packaging, and 98% did not receive a reminder from their physician or pharmacist to refill their prescription (Table 5).
  | Table 5 Awareness, blood pressure information, and relationship with healthcare provider |
Factors associated with medication adherence
Two hundred thirty-three (93.5%) participants who adhered to the prescribed medications were covered by health insurance, which shows a significant association (p=0.01), between health coverage and adherence. In addition, 97.6% of participants visit cardiologist (p=0.807), 84.7% of them knew the reading of their BP when diagnosed with HT for the first time (p=0.093), 73.1% admitted that they knew the underlying cause of their disease (p=0.645), 72% measure their BP at home (p=0.205), 68% take supplements for HT treatment (p=0.746), 80% were hospitalized for high BP (p=0.168). All these findings show no significant difference between adherent and non-adherent participants (Table 6).
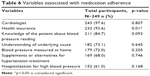  | Table 6 Variables associated with medication adherence |
Discussion
When BP is too high for too long, it damages the blood vessels and low-density lipoprotein cholesterol begins to accumulate along tears in the artery walls. This increases the workload of the circulatory system while decreasing its efficiency. As a result, high BP puts the patient at greater risk for the development of life-changing and potentially life-threating conditions.12 The study was carried out to examine the prevalence of adherence to antihypertensive treatment and the extent of patient’s knowledge about the disease, risk factors, and medication side effects. Stress, limited physical activity, and unhealthy diet emerged as the perceived most important risk factors of HT. The study also demonstrates that 85% of the participants were found to be adherent to their treatment. This percentage is greater than the rate of adherence (77.6%) in a study conducted in Beirut in 2015,13 and reported from Germany (56%),14 Ethiopia (64.6%),15 Saudi Arabia (53%),10 China (65.1%),16 Malaysia (44.2%),17 Pakistan (57%),18 and Gambia 27%.19 However, this percentage is lower than that demonstrated by a study conducted in Scotland (91%).20 The percentage of 85% seems to be biased as participants were unaware about the exact definition of adherence, despite the efforts made by the trained interviewers. The results could be explained by the low educational level observed in 80% of the participants. The results are also supported by the following findings: 52.6% of the participants did not follow regular checkups with their healthcare providers; 48.6% did not check their BP for more than 2 weeks; 41.4% suffered from headache due to uncontrolled BP; and 61% were hospitalized for uncontrolled BP. In addition, 93.5% of the study group, which showed a significance association with adherence, had a health coverage that eliminated the cost factor, which is considered as one of the most common barriers to medication adherence. Consequently, as hospitalization is costly in developing countries suffering from limited resources, healthcare providers and payers should focus on interventions to improve medication adherence. The Ministry of Public Health in Lebanon covers hospital inpatient expenditures of uninsured patients, which are estimated to be half of the Lebanese population. Medication adherence is a growing concern to clinicians, healthcare systems, and other stakeholders (eg, payers) in the majority of countries. Such concern is due to the mounting evidence that non-adherence is prevalent and is associated with adverse outcomes and higher costs of care.21 These findings emphasize the importance of raising awareness and promoting the knowledge about adherence definition and behavior to hypertensive patients.
The results of our study show that there is no significant association between HT knowledge and medication adherence as reported by 85% of the participants. These results are consistent with a study performed in patients recruited from a health maintenance organization in United States, which showed no significant effects between compliance to medications and the knowledge regarding HT. Our study also showed that 73.1% of the participants knew the underlying cause of the disease and that no significant difference was demonstrated between adherence and non-adherence, although learning about HT and its underlying causes may be helpful in improving adherence.22
The Nigerian’s study shows that patients attending the cardiology clinic had at least a higher level of medium medication adherence than those attending general outpatient clinic.23 In our study, there was no significant difference between physician specialty and medication adherence. This can be explained by the confidence and satisfaction perceived by patients choosing to visit either generalist or specialized physician.
A Japanese questionnaire-based study24 found that 49% of patients reported adverse effects with their antihypertensive medicines, and a statistically significant relationship between the number of reported adverse effects and non-adherence. These results are consistent with our study, which demonstrates that 41% of participants had changed their antihypertensive medications during the last year because of medication non-tolerated side effects. Physicians should tell the patients about the adverse effects of the prescribed drugs and the risk of rebound effect related to antihypertensive drugs’ abrupt discontinuation.
Poor memory was the most commonly reported barrier to medication adherence as 89.5% of non-adherent participants in our study referred their practice to mere forgetfulness. This finding is in line with that of a study from Pakistan, which reported that 56.8% of the participants missed doses due to forgetfulness.25 Moreover, our data demonstrate that only 3.6% of the treating physicians recommend the use of special container for medication packaging, and that 2% of the pharmacists or physicians remind their patients to refill their prescription. Appropriate measures should be taken to enhance patient memory, including planning to take medications in conjunction with certain activities, such as eating meals, and recommending the use of pill boxes that organize the process of medication intake.
A substantial portion of patients with HT in our study (42%) used complementary and alternative medicine (CAM) in addition to prescribed medications to help control their BP, compared to 26.5% in a study conducted in Louisiana.26 Based on this, it can be said that the use of CAM may be an important modifiable barrier or a signal of other barriers (eg, side effects and costs of medications) to antihypertensive medication adherence and subsequent BP control.
In addition, our study shows that 37% of the participants are following a DASH diet, which reflects an aspect of a management plan that adherers complied with, in addition to taking medication. A study conducted in the United States shows that compared with the control diet of high sodium level, the DASH diet with a low sodium level led to a mean SBP that was 11.5 mmHg lower in participants with HT.27 Another study shows that BP in the DASH group fell from 146/85 to 134/82 mmHg.28 This probably indicates that HT management is an integrated plan where the pharmacological treatment is complementary to the non-pharmacological one.
In our study, 41% of participants presented with HT for more than 10 years. Our finding is consistent with a study conducted in Nigeria, which found that the duration of HT was the highest (11.4 years) in the high adherence group.29 Similarly, a study conducted in China14 shows that patients with longer duration of antihypertensive agents used over 10 years reported better adherence than patients with shorter duration of 5 years or less. Based on such findings, it may be concluded that a history of HT can be related to adherence level. In fact, these participants are likely to have more information about the disease and established stronger patient-physician relationship than those with a shorter history of HT.
The interaction with participants completing the questionnaire survey revealed that the majority considered the relationship with their physician to be of great importance. It was demonstrated that 48% of the participants did not get the necessary counseling on the risk of non-adherence from their health care providers. Interestingly, the study of Degli Esposti et al shows that younger doctors tended to have more adherent patients.30 Ren et al have also found that patients treated by nurses or physicians’ assistants were more likely to be compliant than patients treated by physicians.31 Distant and formal physician-patient relationship could compel the patient to go to another treating physician and lead to non-adherence.
Conclusion
This study presents important findings about the need for more informed knowledge about the disease, risk factors, and medication side effects in order to enhance adherence to treatment. The study also highlights many factors that may impact adherence levels, and confirms the importance of cognitive and communication status.
We therefore conclude that chronic disorders such as HT can be better managed if it is provided together with the provision of qualitative health education aimed at improving medication adherence at the community level, reducing the worldwide burden of cardiovascular disease associated with HT, and reducing healthcare cost in specific.
Acknowledgment
This project has been funded with support from Lebanese University.
Disclosure
The authors report no conflicts of interest in this work.
References
Global Health Observatory (GHO) data. Raised blood pressure: situation and trends. World Health Organization. 2014. Available from: http://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence_text/en/. Accessed January 10, 2017. | ||
Matar D, Frangieh AH, Abouassi S, et al. Prevalence, awareness, treatment, and control of hypertension in Lebanon. J Clin Hypertens (Greenwich). 2015;17(5):381–388. | ||
Tohme RA, Jurjus AR, Estephan A. The prevalence of hypertension and its association with other cardiovascular disease risk factors in a representative sample of the Lebanese population. J Hum Hypertens. 2005;19(11):861–868. | ||
Joint National Committee 8 (JNC 8) guidelines for the management of hypertension in adults. Am Fam Physician. 2014;90(7):503–504. | ||
National Heart, Lung, and Blood Institute (NHLBI). DASH Eating Plan. 2014. Available from: https://www.nhlbi.nih.gov/health/health-topics/topics/dash. Accessed December 10, 2016. | ||
Sulbaran T, Silva E, Calmon G, Vegas A. Epidemiologic aspects of arterial hypertension in Maracaibo, Venezuela. J Hum Hypertens. 2000;14(Suppl 1):S6–S9. | ||
World Health Organization. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003. Available from: http://www.who.int/chp/knowledge/publications/adherence_introduction.pdf. Accessed December 10, 2016. | ||
World Health Organisation. Cardiovascular diseases (CVDs). Fact sheet [updated May 2017]. Available from: http://www.who.int/mediacentre/factsheets/fs317/en/. Accessed May 18, 2016. | ||
ABC Project. Ascertaining barriers for compliance: policies for safe, effective and cost-effective use of medicines in Europe. ABC Project. 2012. Available from: http://www.abcproject.eu/img/ABC%20FINAL.pdf. Accessed January 10, 2017. | ||
Khalil SA, Elzubier AG. Drug compliance among hypertensive patients in Tabuk, Saudi Arabia. J Hypertens. 1997;15(5):561–565. | ||
Surveysystem.com. Creative Research Systems. 2012. Available from: http://www.surveysystem.com/sscalc.htm | ||
AHA High Blood Pressure Web. Updated May 2017. Available from: http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/LearnHowHBPHarmsYourHealth/Health-Threats-From-High-Blood Pressure_UCM_002051_Article.jsp#.WdN5xPVrzDc | ||
Yassine M, Al Hajj A, Awada S, et al. Evaluation of medication adherence in Lebanese hypertensive patients. J Epidemiol Glob Health. 2016;6(3):157–167. | ||
Schmieder RE, Ott C, Schmid A, et al. Adherence to antihypertensive medication in treatment-resistant hypertension undergoing renal denervation. J Am Heart Assoc. 2016;5(2):e002343. | ||
Ambaw AD, Alemie GA, W/Yohannes SM, Mengesha ZB. Adherence to antihypertensive treatment and associated factors among patients on follow up at University of Gondar Hospital, Northwest Ethiopia. BMC Public Health. 2012;12(2):282. | ||
Lee GK, Wang HH, Liu KQ, Cheung Y, Morisky DE, Wong MC. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. PLoS One. 2013;8(4):e62775. | ||
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. | ||
Lennon C, Hughes CM, Johnston GD, McElnay JC. Identification of psychosocial factors which influence patient adherence with antihypertensive medication. Int J Pharm Pract. 2001;9(Suppl 1):R8. | ||
van der Sande MA, Milligan PJ, Nyan OA, et al. Blood pressure patterns and cardiovascular risk factors in rural and urban Gambian communities. J Hum Hypertens. 2000;14(8):489–496. | ||
Youssef RM, Moubarak II. Patterns and determinants of treatment compliance among hypertensive patients. East Mediterr Health J. 2002;8(4–5):579–592. | ||
Ammar W. Health beyond politics. World Health Organization Eastern Mediterranean Regional Office. Lebanon: Ministry of Public Health; 2009. | ||
Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17(7):504–511. | ||
Akintunde AA, Akintunde TS. Antihypertensive medications adherence among Nigerian hypertensive subjects in a specialist clinic compared to a general outpatient clinic. Ann Med Health Sci Res. 2015;5(3):173–178. | ||
Toyoshima H, Takahashi K, Akera T. The impact of side effects on hypertension management: a Japanese survey. Clin Ther. 1997;19(6):1458–1469. | ||
Almas A, Hameed A, Ahmed B, Islam M. Compliance to anti-hypertensive therapy. J Coll Physicians Surg Pak. 2006;16(1):23–26. | ||
Krousel-Wood MA, Muntner P, Joyce CJ, et al. Adverse effects of complementary and alternative medicine use on antihypertensive medication adherence: findings from the cohort study of medication adherence among older adults. J Am Geriatr Soc. 2010;58(1):54–61. | ||
Sacks FM, Svetkey LP, Vollmer WM, et al; DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N Engl J Med. 2001;344(1):3–10. | ||
Moore TJ, Conlin PR, Ard J, Svetkey LP. DASH (dietary approaches to stop hypertension) diet is effective treatment for stage 1 isolated systolic hypertension. Hypertension. 2001;38(2):155–158. | ||
Hyre AD, Krousel-Wood MA, Muntner P, Kawasaki L, DeSalvo KB. Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting. J Clin Hypertens (Greenwich). 2007;9(3):179–186. | ||
Degli Esposti E, Sturani A, Di Martino M, et al. Long-term persistence with antihypertensive drugs in new patients. J Hum Hypertens. 2002;16(6):439–444. | ||
Ren XS, Kazis LE, Lee A, Zhang H, Miller DR. Identifying patient and physician characteristics that affect compliance with antihypertensive medications. J Clin Pharm Ther. 2002;27(1):47–56. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
