Back to Journals » Patient Preference and Adherence » Volume 14
Adherence to Subcutaneous Anti-TNF Treatment in Chronic Inflammatory Rheumatism and Therapeutic Patient Education
Authors Fayet F, Fan A, Rodere M , Savel C, Pereira B , Soubrier M
Received 27 November 2019
Accepted for publication 28 January 2020
Published 24 February 2020 Volume 2020:14 Pages 363—369
DOI https://doi.org/10.2147/PPA.S240179
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Françoise Fayet,1 Angélique Fan,1 Malory Rodere,1 Carine Savel,1 Bruno Pereira,2 Martin Soubrier1
1Rheumatology Department, CHU Clermont-Ferrand, Clermont-Ferrand, France; 2Biostatistics Unit, CHU Clermont-Ferrand, Clermont-Ferrand, France
Correspondence: Françoise Fayet
Rheumatology Department, CHU Clermont-Ferrand, Place Henri Dunant, Clermont-Ferrand 63000, France
Email [email protected]
Objective: Poor patient adherence to anti-TNF treatment has proven to be a major roadblock to effective management. Therapeutic patient education (TPE) is now recognized as a crucial tool in managing conditions like chronic inflammatory rheumatism and in improving treatment adherence. This study aimed to assess whether different TPE programs might improve adherence to subcutaneous anti-tumor necrosis factor (anti-TNF) treatment in patients with rheumatoid arthritis (RA), ankylosing spondyloarthritis (AS), and psoriatic arthritis (PsA).
Methods: This was a retrospective, observational, monocentric study of current care practices. We included 193 patients (124 women; mean age 53.3 ± 14.8 years). All patients received subcutaneous anti-TNF treatment and one of three TPE models, delivered by a nurse, from 2009 to 2013. The cohort was grouped according to different educational models: M1: information (N=92); M2: individual TPE (N=80); and M3: individual and group TPE sessions (N=21). Adherence was assessed with the Morisky Medication Adherence Scale (MMAS-4™). Scores were rated as follows: good adherence (MMAS-4 = 4), moderate adherence (MMAS-4 = 2– 3), and poor adherence (MMAS-4 = 0– 1).
Results: The mean disease duration was 10 years [95% CI: 5 to 18]. The cohort comprised 113 patients with RA, 73 with AS, and seven with PsA. Overall, 146 (75.7%) patients displayed good adherence, 34 (17.6%) displayed moderate adherence, and 13 (6.7%) displayed poor adherence. The M3 group displayed less adherence than the M1 and M2 groups. Old age was the only factor correlated with good adherence (p=0.005). The level of knowledge had no significant impact on adherence.
Conclusion: This study demonstrated good adherence to anti-TNF treatment in patients that received TPE, particularly when it was delivered in individual sessions.
Keywords: chronic inflammatory rheumatism, subcutaneous anti-TNF, treatment adherence, therapeutic education
Introduction
Over the last few years, with the emergence of anti-tumor necrosis factor (anti-TNF) agents, treatment options have significantly increased for patients with chronic inflammatory rheumatism (CIR), including rheumatoid arthritis (RA), and ankylosing spondyloarthritis (AS). However, patient adherence to these treatments appears to be sub-optimal. In the Smolen study, the percentage of patients that demonstrated good adherence with an anti-TNF agent was 75% for those with RA, 68% for those with AS, and 70% for those with psoriatic arthritis (PsA).1 Poor patient adherence to treatments has proven to be a major roadblock to effective management.2 Treatment adherence is determined by the complex interactions of several factors: the disease, drug therapies, demographic and socioeconomic factors, treatment beliefs, the opinions of patients and their friends or family, and the other healthcare system services (advice, education, etc.).1,3,4
Therapeutic patient education (TPE) is now recognized as a crucial tool in managing conditions like CIR.5,6 Among the factors likely to improve treatment adherence, TPE has been the most extensively studied, and this approach is supported by the highest level of evidence.7–12 Consequently, we implemented a TPE program in our department, with the aim of encouraging patients to self-manage subcutaneous biotherapies. France’s national authority of health (Haute Autorité de Santé, HAS) recommended structuring TPE in four stages (educational diagnosis, educational objectives, education, and assessment) in individual consultations or group sessions.13 In the current nursing practice, this structure was complicated by organizational issues, and sometimes, only a brief individual informative consultation with a nurse could be delivered, without a previous educational diagnosis. A previous observational study, conducted by nurses,14 was designed to assess which educational model was the most effective for ensuring that patients with CIR could manage their subcutaneous anti-TNF treatments in the safest way possible. That study demonstrated that combining individual TPE consultations with group sessions resulted in higher knowledge and competence scores, compared to providing individual TPE alone or simply providing information to patients that required anti-TNF treatment.14
The primary endpoint of the present, ancillary study was to assess adherence to subcutaneous anti-TNF in patients with CIR (RA, AS, and PsA) that received TPE in different forms. We also aimed to study how knowledge about anti-TNF influenced adherence.
Patients/Methods
Study Design
This retrospective, observational, monocentric study of current care practices included all patients treated with subcutaneous anti-TNF that had received at least one TPE session, delivered by a nurse, between 2009 and 2013. The TPE sessions were categorized a posteriori, according to the following TPE models:15,16
Model 1 (M1): A brief individual consultation lasting approximately half an hour was provided that was informative in nature; ie, the pedagogical “behavioral model”, which is focused on information. The consultation was with a nurse, and it was not preceded by an educational diagnosis.
Model 2 (M2): At least two individual consultations were provided lasting approximately 1 hour, which included the following the four recommended stages: (1) educational diagnosis, (2) objectives, (3) education, and (4) assessment. This “constructive model” was a singular development model, based on the patient’s potential, resources, and relationship with his/her physician. An educational diagnosis was performed to develop an understanding of the patient, with the following questions: Who is the patient? What does he/she do, what does he/she know, and what does he/she believe? How does he/she live? What are his/her future plans? This diagnosis included a meeting between the nurse and patient to negotiate and prioritize goals; then a later meeting to assess those goals.
Model 3 (M3): Individual and group sessions that included all four stages; ie, the “social-constructivist model”. This social development model was based on group interactions and potential. All four recommended stages were provided via individual and group sessions. The two individual sessions for diagnosis and for evaluation lasted approximately 1 hour each. The group sessions lasted approximately 1 hour and included six to eight patients per group.
For all three educational models, the treatment benefits and risks were presented to each patient. In addition, patients learned risk prevention methods (eg, vaccinations, dental hygiene, etc.); safe injection conditions versus those considered unsafe (eg, infection symptoms or fever, wound, dentistry, surgery, pregnancy); and the proper subcutaneous injection technique.
Data Collection
Anti-TNF treatment adherence was assessed with the Morisky Medication Adherence Scale (MMAS-4™), which included four questions, or with a generic scale for evaluating treatment adherence behavior.17–19 The questions were (1) Do you ever forget to take your treatment? (2) Do you sometimes have difficulty remembering to take your treatment? (3) When you feel well, do you sometimes stop taking your treatment? (4) If you ever feel worse after taking your treatment, do you sometimes stop? The MMAS-4 was previously validated as a useful, reliable tool for treatment adherence. It was shown to have high sensitivity (0.81) and moderate specificity (0.44).17–19 Adherence was classed as follows: good (MMAS-4 = 4), moderate (MMAS-4 = 2–3), and poor (MMAS-4 = 0–1).
Each patient’s knowledge about anti-TNF treatment was assessed with the Biosecure self-completed questionnaire, which was developed and validated by the TPE section of the French Society for Rheumatology (Société française de Rhumatologie, SFR).20 This questionnaire featured 55 items (scored 0 to 100), which covered various capacity levels, such as managing infections, vaccinations, and everyday situations (eg, travel, surgery, or planned pregnancy). It also included 30 questions for evaluating knowledge (theoretical knowledge) and 25 questions that described seven hypothetical situations (practical knowledge). The patient selected one of three possible responses: yes/no/I do not know.
The Biosecure score was divided into different skill areas, including general knowledge, reaction when faced with infection or fever, reaction when faced with a wound, prevention of infection, vaccinations, dental hygiene, planned surgery, planned pregnancy, communication, and subcutaneous treatment. One of the questions and one hypothetical clinical setting specifically addressed subcutaneous biotherapies; thus, those items did not apply to patients that received intravenous biotherapies. Consequently, we assessed competence in two parts, one part included all patients that received either intravenous or subcutaneous biotherapy; and the second part only included patients that received subcutaneous biotherapy. Each correct answer received one point. The knowledge score was calculated as the total of all points received, out of 100. The higher the score, the better the knowledge.
The following social-demographic data were collected: date of birth, gender, marital status, socio-professional class, education, and the distance travelled to reach the clinics. The following clinical data were also collected: CIR diagnosis and year of diagnosis; the treatment year (the year the biotherapy was initiated and stopped); the number of consultations; the date of the last consultation; the type of management (in-hospital only or mixed); and the frequency of injections.
Study ethics approval was obtained on 30 June 2017 (CECIC Rhône-Alpes-Auvergne, Grenoble, IRB 5921), all patients provided written informed consent, and the study was conducted in accordance with the Declaration of Helsinki.
Statistical Considerations
All analyses were performed with Stata software (Version 13, StataCorp, College Station, TX). All analyses used a two-sided Type I error of α=5%. Patient characteristics are expressed as the mean ± standard-deviation (SD) or the median and interquartile range (IQR) for continuous data. The assumption of normality was assessed with the Shapiro–Wilk test. Categorical parameters are expressed as numbers and percentages. Quantitative variables were compared between independent groups with an ANOVA or a Kruskal–Wallis test, when ANOVA conditions were not met (normality and homoscedasticity, evaluated with the Bartlett test). When appropriate, post hoc tests were performed to account for multiple comparisons (Tukey–Kramer for the ANOVA and Dunn for the Kruskal–Wallis test). Comparisons between independent groups were performed with the Chi-square or Fisher’s exact test for categorical variables. When appropriate, a post hoc test was used (Marascuillo procedure).
To determine factors associated with observations that were considered a Class 3 variant, a multivariate polynomial ordinal regression model was performed with the stepwise approach (backward and forward). The covariates were fixed according to univariate results (p <0.05) and clinical relevance. Particular attention was paid to the study of multicollinearity and interactions between covariates: 1) we studied the relationships between the covariates and 2) we evaluated the impact of adding or deleting variables on the multivariate model. Results are expressed as relative risk ratios (RR) and 95% confidence intervals (95% CI).
Results
This study included 193 patients. The cohort included 124 women and the mean population age was 53.3 ± 14.8 years. The mean CIR duration was 10 years [5; 18]. Patients were diagnosed with RA (n = 113), AS (n = 73), and PsA (n = 7). Among the 193 patients, injections were administered once per week (n = 108; 60%), once every 15 days (n =68; 35%), or once per month (n = 17; 5%). We found good compliance in 146 (75.7%), moderate compliance in 34 (17.6%), and poor compliance in 13 (6.7%) patients.
The M1, M2, and M3 models were followed by 92, 80, and 21 patients, respectively. Characteristics of patients according to their educational model were presented in Table 1. Patients attended on median 1 [1;1] session in group M1, 2 [1;3] in group M2 and 4 [4;5] sessions in group M3. The median number of TPE session attended by patients was 2 [1;3] and was no different according to medication adherence (p=0.46).
 |
Table 1 Characteristics of Patients According to Their Educational Model |
The M3 group (TPE given in group and individual consultations) displayed significantly worse anti-TNF adherence compared to the other two groups (p=0.04) (Figure 1). The proportions of patients that showed good anti-TNF adherence were significantly different between M1 and M3 (p=0.049) and between M2 and M3 (p=0.04); in contrast, no difference was found between M1 and M2 (p=0.70; Figure 1).
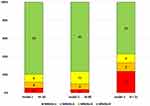 |
Figure 1 Morisky Medication Adherence Scale (MMAS-4) scoring for the three therapeutic patient education models (models 1–3). MMAS-4 scores are color-coded; adherence was categorized as follows: MMAS=1: poor; MMAS=2 or 3: moderate; MMAS=4: good. Notes: Adapted with permission from Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74.17 Use of the MMAS is protected by US and International copyright and Trademark laws. Permission for use is required. A license agreement is available from Donald E. Morisky, MMAS Research (MORISKY), 294 Lindura Court, Las Vegas, NV 89138-4632 [email protected]. |
Table 2 presents the study of relationships between medical adherence and potential influencing factors, categorized by patient characteristics. In univariate analysis, only age of patients was associated with good adherence, ie, older patients showed better adherence than younger patients: 50.5±16.7 for poor adherence, 45.9±15.2 for moderate adherence and 55.3±14.0 for good adherence (p=0.005). These findings, including association between medical adherence and TPE models, were confirmed by multivariable analysis, adjusted for age, gender, and the time interval before commencing treatment. For age, relative risk (RR) was 0.95 [0.91; 0.99] (p=0.042) between poor and good adherence. For TPE models, the M3 group (TPE given in group and individual consultations) displayed significantly worse anti-TNF adherence (between poor and good adherence) compared to the other two groups (vs M1: RR=9.10 [1.79; 46.3] (p=0.008); vs M2: RR=11.0 [2.06; 58.9] (p=0.005)). In multivariable analysis, no relation with medical adherence was highlighted for gender RR=0.42 [0.08; 2.08] (p=0.286) and for time before treatment initiation RR=1.18 [0.96, 1.45] (p=0.119).
 |
Table 2 Anti-TNF Adherence According to Patient Characteristics |
Discussion
We found that a majority (75.7%) of patients with CIR displayed good adherence to anti-TNF treatment after receiving TPE. This finding was consistent with the good adherence level reported by Smolen et al (70.6–74.1%), in a study of 3390 patients (RA: n=1943; AS: n=812, PsA: n=635), based on the Morisky MMAS-4© questionnaire.1 However, Smolen et al did not report whether those patients benefitted from TPE. We found that anti-TNF adherence did not differ between patients with different types of CIR; this finding contrasted with the findings of Smolen et al, who demonstrated identical anti-TNF adherence in patients with RA and PsA, but worse adherence in patients with AS.1 In our study, adherence was not impacted by the disease duration or to the number of sessions attended by the patient. However, adherence was better in older subjects than in younger subjects, consistent with Smolen et al. In addition, that study showed that anti-TNF adherence was improved among patients that believed the treatment would be effective, compared to those that worried about the inherent risks of treatment, based on the Beliefs about Medicine Questionnaire.21
We tested three different education models. Of these, we found that anti-TNF adherence was worse in patients that received both individual and group TPE sessions, compared to those that received either an individual consultation only or information only. No other studies are available in the literature for comparing our findings; however, the Stockl study demonstrated the value of implementing an individual TPE program delivered by pharmacists and nurses. They found that an individual TPE program improved patient adherence to biotherapy, compared to current care practices.12 Similarly, individual TPE sessions were effective in improving adherence in patients with RA that underwent conventional long-term treatments. Indeed, Ravindra et al reported better adherence to conventional long-term treatments in 64 patients that had received two individual TPE sessions with doctors, compared to a control group that received typical care.8 Telephone-based TPE, provided by pharmacists, was also shown to have a significant impact on treatment adherence in various types of chronic disease, including RA.9 In contrast, Bruce and Helliwell found, in two randomized studies, that group TPE sessions did not impact adherence to long-term conventional treatments in RA22,23 compared to subjects managed with current clinical practices. In that study, the TPE comprised four to six group sessions covering patient understanding of the disease, treatments, and their beliefs.22,23
The present study also found that anti-TNF adherence was not associated with knowledge, which was assessed with the Biosecure score. We speculated that the group TPE sessions in our study might have generated false beliefs, brought up by certain patients, which then gave rise to an inverse correlation between fear of treatment and treatment adherence in CIR (1). Regardless of whether that was true, our findings, combined with those in the literature, should encourage Rheumatology departments to improve anti-TNF adherence by offering patients individual TPE consultations, rather than group TPE sessions, when subcutaneous anti-TNF treatment is required. However, our findings require confirmation in future studies.
Conclusion
This study demonstrated good adherence to anti-TNF treatment in patients that received TPE, particularly when it was delivered in individual sessions.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Smolen JS, Gladman D, McNeil HP, et al. Predicting adherence to therapy in rheumatoid arthritis, psoriatic arthritis or ankylosing spondylitis: a large cross-sectional study. RMD Open. 2019;5:e000585. doi:10.1136/rmdopen-2017-000585
2. Bluett J, Morgan C, Thurston L, et al. Impact of inadequate adherence on response to subcutaneously administered anti-tumour necrosis factor drugs: results from the biologics in rheumatoid arthritis genetics and genomics study syndicate cohort. Rheumatology (Oxford). 2015;54:494–499. doi:10.1093/rheumatology/keu358
3. Haynes R, Taylor D, Sackett D, editors. Compliance in health care. In: Compliance in Health Care. Baltimore: Johns Hopkins University Press; 1979:1–15.
4. Sabaté E, World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. Geneva: World Health Organization; 2003:198.
5. Gaujoux-Viala C, Gossec L, Cantagrel A, et al. Recommendations of the French Society for Rheumatology for managing rheumatoid arthritis. Joint Bone Spine. 2014;81:287–297. doi:10.1016/j.jbspin.2014.05.002
6. Zangi HA, Ndosi M, Adams J, et al. EULAR recommendations for patient education for people with inflammatory arthritis. Ann Rheum Dis. 2015;74:954–962. doi:10.1136/annrheumdis-2014-206807
7. Hill J, Bird H, Johnson S. Effect of patient education on adherence to drug treatment for rheumatoid arthritis: a randomised controlled trial. Ann Rheum Dis. 2001;60:869–875.
8. Ravindran V, Jadhav R. The effect of rheumatoid arthritis disease education on adherence to medications and followup in Kerala, India. J Rheumatol. 2013;40:1460–1461. doi:10.3899/jrheum.130350
9. Clifford S, Barber N, Elliott R, Hartley E, Horne R. Patient-centred advice is effective in improving adherence to medicines. Pharm World Sci. 2006;28:165–170. doi:10.1007/s11096-006-9026-6
10. Zhang X, Tian Y, Li J, Zhao X. Effect of targeted nursing applied to SLE patients. Exp Ther Med. 2016;11:2209–2212. doi:10.3892/etm.2016.3173
11. Fields TR, Rifaat A, Yee AMF, et al. Pilot study of a multidisciplinary gout patient education and monitoring program. Semin Arthritis Rheum. 2017;46:601–608. doi:10.1016/j.semarthrit.2016.10.006
12. Stockl KM, Shin JS, Lew HC, et al. Outcomes of a rheumatoid arthritis disease therapy management program focusing on medication adherence. J Manag Care Pharm. 2010;16:593–604. doi:10.18553/jmcp.2010.16.8.593
13. French National Authority for Health. Structuring a therapeutic patient education program in the field of chronic diseases - Methodological Guide; June 2007. (pages consultées le 05/ 03/2015), [en ligne]. Available from: http://www.has-sante.fr/portail/upload/docs/application/pdf/etp_-_comment_elaborer_un_programme_-_recommandations_juin_2007.pdf.
14. Fayet F, Rodere M, Savel C, Pereira B, Soubrier M, Couderc M.Education models and acquisition of biotherapies safety skills in chronic inflammatory rheumatism. Ther Patient Educ.2019;11:10206. doi:10.1051/tpe/2019004
15. Eymard C. From Models of Education and Health to Therapeutic Education Activity. Therapeutic Patient Education: Models, Practice and Evaluation. Saint-Denis: Inpes; 2010:39–53. [book in french].
16. D’Ivernois JF, Gagnayre R. Learning to Educate the Patient: Pedagogical Approach (4th Edition). Paris: Maloine; 2011:28–90. [book in french].
17. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi:10.1097/00005650-198601000-00007
18. Morisky DE, Malotte CK, Choi P, et al. A patient education program to improve adherence rates with antituberculosis drug regimens. Health Educ Q. 1990;17:253–267. doi:10.1177/109019819001700303
19. Morisky DE, DiMatteo MR. Improving the measurement of self-reported medication nonadherence: response to authors. J Clin Epidemiol. 2011;64:255–257. doi:10.1016/j.jclinepi.2010.09.002
20. Gossec L, Fautrel B, Flipon É, et al. Safety of biologics: elaboration and validation of a questionnaire assessing patients’ self-care safety skills: the BioSecure questionnaire. An initiative of the French Rheumatology Society Therapeutic Education section. Joint Bone Spine. 2013;80:471–476. doi:10.1016/j.jbspin.2012.11.009
21. Robert H, John W, Maittew H. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14(1):1–24.
22. Brus HL, van de Laar MA, Taal E, Rasker JJ, Wiegman O. Effects of patient education on compliance with basic treatment regimens and health in recent onset active rheumatoid arthritis. Ann Rheum Dis. 1998;57:146–151. doi:10.1136/ard.57.3.146
23. Helliwell PS, O’Hara M, Holdsworth J, Hesselden A, King T, Evans P. A 12-month randomized controlled trial of patient education on radiographic changes and quality of life in early rheumatoid arthritis. Rheumatology (Oxford). 1999;38:303–308. doi:10.1093/rheumatology/38.4.303
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
