Back to Journals » Risk Management and Healthcare Policy » Volume 13
A Descriptive Cross-Sectional Study on Awareness and Belief of People About Cancer in Southern Ethiopia: Special Focus on Breast and Cervical Cancers
Authors Labisso WL , Leka Y, Leka Y, Haileselassie W
Received 11 June 2020
Accepted for publication 14 October 2020
Published 19 November 2020 Volume 2020:13 Pages 2655—2668
DOI https://doi.org/10.2147/RMHP.S267207
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Marco Carotenuto
Wajana Lako Labisso,1 Yishak Leka,2 Yohannes Leka,3 Werissaw Haileselassie4
1Department of Pathology, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 2Department of Pathology, College of Health Sciences and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia; 3Department of Medical Microbiology, College of Health Sciences and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia; 4Department of Reproductive Health and Health Service Management, School of Public Health, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Wajana Lako Labisso
Department of Pathology, School of Medicine, College of Health Sciences, Addis Ababa University, Ethiopia
Tel +251966334092
Email [email protected]
Background: The general population’s lack of awareness, limited knowledge, myths and misconceptions about breast and cervical cancers (CCs) is considered as a serious public health problem.
Objective: This study was intended to assess the status of awareness and beliefs of people about cancer and breast and CCs in particular.
Methods: A descriptive community-based cross-sectional survey was conducted on 345 study participants in Southern Ethiopia. A pretested, structured questionnaire that contained demographics and questions on the variables of exposure to biological and chemical carcinogenic agents, lifestyle and personal behavior was administered. Frequency distribution and proportions were used to describe the study population in relation to major variables.
Results: The mean age of study participants was 25.19 (Range 15– 58). More than a third of the study participants heard about cancer from Mass Media followed by schools (28.5%) and treating physicians (6.7%). The proportion of study participants that knew about the association between smoking, alcohol intake and cancer development was 38.6% and 51.5%, respectively. Only 48% and 24.2% of the study participants heard about breast and CCs, respectively. The fact that 69.4% of the study participants had limited knowledge about the mode of transmission of the causative agents of CCs indicates that the study groups are at risk of acquiring the agent. Additionally, only 4.7% of the study participants were screened for CC and have poor breast self-examination experiences, indicating poor awareness and knowledge about the importance of screening programs.
Conclusion: Comprehensive awareness and knowledge about cancer in general and breast and CCs in particular is lacking in southern Ethiopia. Early sexual debut, limited knowledge about the diseases and unfavorable lifestyle are the risk factors to be addressed in public health education.
Keywords: cervical cancer, breast cancer, southern Ethiopia, cancer awareness
Introduction
Cancer is still one of the leading public health burdens in both high and low income countries. More than half of all cancer morbidities and mortalities in 2018 occurred in low and middle income countries (LMICs).1,2 While the rate of mortality from cancer is significantly declining in most high income countries (HICs), this is not true in LICs. Statistical estimation by the World Health Organization (WHO) indicated that of 12 million expected new cases and 7.6 million mortality by the year 2030, about three-fourth are expected to occur in LMICs, which are not well-prepared to combat their growing cancer burdens.2,3 Moreover, a fourth of cancer deaths in these countries is attributed to infectious agents. Cancers associated with pathogens are of paramount importance for LMICs as these countries are persistently challenged by infectious diseases.3,4 Of course, most forms of cancers are linked with the lifestyles of people like smoking, obesity, lack of physical activity and feeding habits. Even though the burden of cancer is strikingly increasing from year to year in LMICs, there exists limited national and regional strategies to combat the impact of cancer in these countries. In addition, adequate cancer research centers, standard diagnostic and treatment centers and well-structured prevention strategies are lacking in these countries.5,6
Cancer is not a curse where only certain individuals or groups are affected, rather it is a disease for which anybody can have the chance to be exposed during her/his life. There are myths and misconceptions about cancer by many societies; particularly in less advanced countries.6–10 This could be one of the barriers to overcome the devastating effects of cancer in the society. The myths and misconceptions can only be ended through awareness development by training the communities that cancer is not contagious and not a curse.9–11 In the contemporary era, people do have good awareness about HIV/AIDS, tuberculosis, malaria, sexually transmitted diseases (STD) or other infectious diseases because of unlimited efforts of the government and nongovernmental organizations in LMICS. On the contrary, only a few organizations and individuals are working on cancer, particularly in low income countries, like Ethiopia.12 Most of the people in these countries consider cancer as a communicable disease and have no idea how people acquire cancer and what the risk factors for cancer are.10,11,13 Obviously, cancer is not contagious and it is possible to prevent cancer and cure if it is identified at an early stage. According to the literature more than 40% of cancer cases can be evaded by working on awareness and helping people avoid the risk factors.14–16 Particularly in LMICS, cancer is usually diagnosed at advanced stage where treatment cannot curb the situation.13–16 Taken together, the awaiting big public health challenges in the arena of cancer prevention in LMICs are lack of awareness and deep-rooted wrong beliefs of the people about the occurrence of cancer, their attitude towards the victims and inaccessibility and poor quality of cancer service centers.17–20 Particular studies in Ethiopia show that there is extremely limited awareness and inadequate cancer service provisions in the country.21,22 However, early breast and cervical cancer detections require awareness of breast cancer risk factors, signs and symptoms using different screening techniques. On the other hand, cancer is one of the major causes of morbidity and mortality and emerging public health problems in this country.20–24 Even though there is no national cancer registry in Ethiopia, hospital records indicate that there are more than 250,000 new cancer cases per year, where cervical and breast cancers are the top two leading cancer incidences in the country.23,24 More than 60,000 patients visit Tikur Anbessa Specialized Hospital (TASH), which is the only public radiotherapy center owning hospital in the country. Less than 1% of the referred cancer patients per year could receive complete treatment services mainly because of inadequacy of treatment facilities in the hospital, high cost and inaccessibility of drugs and lack of places to stay during treatment follow-ups.19–24 Therefore, more than 80% of cancer patients already suffer from advanced and incurable stages of the disease at the time of diagnosis and treatment.22–25 This indicates that prevention and early detection will be the most affordable and effective ways to save lives and overcome the impact of cancer in the whole country. To our knowledge, the status of awareness and belief of people about cancer in Wolaita zone, in southern parts of Ethiopia, is not investigated properly. Thus, this study was intended to explore the scope of awareness and belief of people about cancers in general, and breast and cervical cancers in particular, in southern Ethiopia, Wolaita zone.
Materials and Methods
Study Area
This study was conducted in Wolaita zone, which is one of the 13 zonal administrations in Southern Nations and Nationalities and Peoples’ Region (SNNR). Wolaita Zone has 12 weredas: Boloso Bombe, Damot Sore, Diguna Fango, Kindo Koysha, Kido Didaye, Offa, Boloso Sore, Damot Gale, Humbo, Sodo Zuria, Damot Pulasa and Damot Weydie, of which the last 6 were included in this study. The map showing the location of Wolaita administrative zone is shown in Figure 1.
 |
Figure 1 Administrative map of Wolaita Zone. |
Study Design, Population and Sampling Techniques
A community-based crossectional study design was employed. Multistage cluster sampling technique was applied to select 6 weredas from the administrative zone under study. The total sample size was allocated between the kebeles (villages) in the selected weredas using non proportional allocation method. Further simple random sampling technique was employed to select specific kebeles (villages). Then, simple random sampling was applied to include study participants in this survey. In addition to individuals with a communication barrier, those that were absent and critically ill at the time of the survey were excluded from the study. The study population was sexually active youth group from the general population, with age 15 and above. The total sample size was allocated proportionally between the selected villages in the 6 woredas. Finally, the required number of study subjects for each stratum was selected randomly using sampling frame obtained from their respective administrative units.
Sample Size Determination
Single population proportion formula was used to calculate the sample size using proportion of women who were knowledgeable about cervical cancer (31%), 95% confidence level and marginal error of 5%.26 Accordingly, the following formula was used to determine the sample size:
The following assumptions were taken to determine the sample size
N = the number of participants to be interviewed
(Z α/2)2 = standardized normal distribution value for the 95% CI, =1.96
P = Proportion of knowledgeable women about cervical cancer P= 31%
d = margin of error taken as 5%
Using the above formula, the calculated sample size turned out to be 329. Adding the 5% non-response rate resulted in the final sample size of 345.
Data Collection
Data was collected from March 10 to April 20, 2019 using a predesigned, structured questionnaire. We have adapted the exiting questionnaire from the cancer prevention questionnaire of the American Cancer Society.27 The English version of the questionnaire was translated into local language by an independent professional and the translated questionnaire was back translated into English by another language professional to ensure the accuracy of translation. Six male and six female nurses were recruited and trained for one week on data collection instrument. Pretest was done on 5% of the total sample size on a different population from the study subjects but with the same socio-economic characteristics. All of the study participants were interviewed using a structured questionnaire containing demographic, health information, and socioeconomic questions. Moreover, the questionnaire included questions on the variables of exposure to some biological and chemical carcinogenic agents, lifestyle and personal behavior. These data included age, age of sexual debut, smoking status, marital status, birth place, ethnic group, sexual behavior, income, occupation (including prostitution), use of contraceptive pills, prior sexually transmitted infections (STI) and number of births. The study was performed by a group of professionals with different backgrounds namely microbiologist, pathologist, public health specialist and cancer biologist. The principal investigator and four public health officers supervised the data collection process to ensure the completeness, accuracy and consistency of the gathered information.
Statistical Analysis
All data were entered into Excel sheet and then exported to SPSS version 24.0 statistical software (IBM SPSS, Chicago, IL). Data cleaning was performed using frequency and tabulation to check for accuracy, consistency and missed values. Frequency distribution, proportions and summary statistics were used to describe the study population in relation to major variables of the study. For all of the statistical tests used in this study, the significant level was set at p-value of less than 0.05.
Data Quality Management
The data collection instrument was tested on a different population from the study subjects but with similar sociodemographic characteristics in a site which is far away from the study area to avoid information contamination prior to the actual study. Accuracy of responses, clarity of questions, error in formulating questions in the questionnaire, user friendliness of the questionnaire and the time it took were assessed and necessary adjustments were made. Moreover, completeness of questionnaire and consistency of information was checked on the spot by field supervisors daily. Regarding data collection process, checkups and daily supervisions were done by the principal investigator and the supervisors. Besides, experienced and trained data collectors were used for data collection activities.
Ethical Consideration
The study protocol was reviewed and verbal informed consent was approved by the Institutional Review Board of the School of Medicine and Health Sciences at Wolaita Sodo University (Ref Nr. WSU/11/23/230). The study was conducted in accordance with the Declaration of Helsinki and verbal informed consent was obtained from all study participants. Parental informed consent was obtained verbally for study participants under 18. Moreover, anonymity and confidentiality of the information obtained was strictly maintained throughout the research process. Woreda and Kebele (Village) administrators were communicated with through formal letter written from College of Health Sciences, Wolaita Sodo University to get permission to conduct the research.
Results
Socio-Demographic and General Characteristics of Study Participants
Out of the total study participants, 95.64% were from Wolaita ethnic group. All of the participants were in the working (economically productive) age group with a mean age of 25.19. More than half and 47.3% of the study subjects were males and females, respectively. The proportion of health professionals among respondents is the same as to that of office workers with a percentage of 11.1. The details of socio-demographic characteristics of the study populations are illustrated in Table 1.
 |
Table 1 Socio-Demographic and General Characteristics of the Study Participants |
Comprehensive Knowledge of People About Cancer
A remarkable proportion (87.2%) of the study participants had information about cancer. More than a third (34.6%) of them heard about cancer from Mass Media (MM), followed by schools (28.5%) and health professionals (6.7%) (Figure 2).
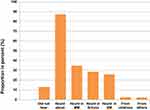 |
Figure 2 Study participants who have heard about cancer and the source of information in Wolaita Zone, Ethiopia. |
Most (72.8%) of the respondents mentioned that they felt frightened when they heard about cancer for the first time. Around 62.1% of the respondents believed that cancer affects anyone while 14.8% of them believed that cancer is a communicable disease. Among the total study participants, 65.4% of them thought that cancer is curable if detected and treated early. About half of the study participants responded that they feared cancer because they believed that cancer has no cure whereas 24.2% of the respondents reported that they developed fear towards cancer due to lack of awareness (Figure 3).
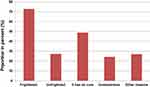 |
Figure 3 Proportion of study participants frightened when heard about cancer and the reasons of the fear in Wolaita Zone, Ethiopia. |
Close to two-thirds of the study participants believed that cancer is preventable while 44.1% of the participants considered that cancer has drugs for treatment (Figure 4). About half of the study participants knew the location of cancer treatment centers in the country whereas 22.5% had no idea where the treatment is provided. More than a third of the study participants heard about the treatment centers from MM. Around 47% of participants think that the prevalence of cancer is increasing in Ethiopia whereas 43.6% of them had a lack of knowledge about its prevalence. Only 7% of the participants perceived that the reason for the increased prevalence is lack of awareness. Less than half (38.6%) of the participants related the risk of cancer with diet. Slightly above half of the participants knew that cancer is related with smoking and alcohol intake. An interesting proportion (64.8%) of the study participants did not know about the availability of non-governmental and governmental associations that work on combating cancer. A significant proportion (89.9%) of the participants mentioned their willingness to work with cancer combating associations in the future. More than half (59.7%) of the respondents reported that they have relatives or friends who died from cancer while 38.6% of the participants mentioned that the cause for the death was breast cancer.
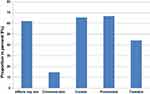 |
Figure 4 Belief of study participants about cancer in Wolaita Zone, Ethiopia. |
The Status of Knowledge and Awareness About Breast and Cervical Cancer
With respect to breast and cervical cancer, only 48% and 24.2% of the study participants heard about breast and cervical cancers, respectively. Similarly, 43.3% of the participants believed that the most common cancer in Ethiopia is breast cancer. A considerable percent of the study participants (38.8%) perceived that breast cancer is caused by infectious agents. Moreover, 49% of the study participants believed that a female can survive after having breast cancer while 41.3% believed that one cannot survive from breast cancer. More than a third (36.6%) of the participants knew a person who had breast cancer whereas 12.3% and 10.3% of the participants knew a person who developed lung and cervical cancers, respectively.
Only 36.2% of the participants believed that cervical cancer is caused by viruses. On the other hand, 28.9% and 14.1% of the study participants believed that it is caused by bacteria and fungi, respectively. Interestingly, 47.3% of the respondents believed that cervical cancer causing agents are transmitted from person to person; of which 18.8% believed that the causative agent is sexually transmitted. Our survey indicated that 76.5% of the study participants believed that cervical cancer is curable if detected and treated early. Interestingly, 66.8% believed that cervical cancer is preventable. Around 56.7% of the participants believed that one can prevent cervical cancer by early screening while 12.1% of them believed that it can be prevented by avoiding unsafe sex. A very small percentages (4.7%) of the participants were screened for cervical cancer. A significant proportion (39.6%) of the respondents had never encountered any illness around the cervix. Only 6.7% of the participants were informed about cervical cancer by their physicians. Regarding the signs and symptoms of cervical cancer, only 4.7% of the participants knew about the signs and symptoms of cervical cancer (Figure 5).
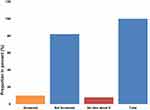 |
Figure 5 Experiences and awareness of study participants about cervical cancer screening in Wolaita Zone, Ethiopia. |
Sexual Characteristics and the Use of Contraceptives
The sexual characteristics of the study subjects were also explored in this study. According to this survey, 49% of the study participants had been sexually active. Out of those who had encountered sex 37.7% experienced their first sexual intercourse at the age ranging from 20–25 followed by those who had been exposed to sexual intercourse as young as 16–20 years, which accounts for 29.5% of the total study population. Concerning current sexual status, the majority (59.9%) had one sexual partner while 37.4% abstained from sexual intercourse. Only 11.9% of the respondents reported having multiple sexual partners. Out of the total study participants, 62.4% had no child. Only 10.8% of those who had children gave their first birth at an age of less than 18 years (Figure 6).
 |
Figure 6 Current sexual characteristic of the study participants. |
The experiences of the study subjects about birth control methods were also assessed. Forty percent of the study participants responded that they had no experiences of using any of the birth control methods. A small proportion of the study participants used injection and condom (18.1% and 15.1%, respectively) as their preferred means of contraceptives (Figure 7).
 |
Figure 7 Practice of the study participants about the common contraceptives in Wolaita Zone, Ethiopia. |
One of the risk factors for cervical cancers is other sexually transmitted diseases (STDs). Thus, the awareness status of study participants about these diseases was surveyed. The results showed that more than half (65.1%) of the study participants had awareness about STDs whereas 34.6% did not have any awareness about such disease. Among those who had awareness, 31.9% were found to have awareness about HIV. Significantly high proportion (90.6%) of the total study participants had never experienced STDs in their life time. Among those who developed STDs, 28.5% and 14.3% of them reported to have gonorrhea and HIV, respectively.
Physical Activity, Smoking Status and Cancer
More than half of the study participants had never done physical exercise and absence of enough time and appropriate place were mentioned as a reason for not doing physical exercise. Moreover, most (66.1%) of the study participants did not know the association between physical exercise and cancer prevention. Interestingly, 98.1% of the study participants had never smoked cigarette. Interestingly, 98.3% of the study participants reported that their spouses had also never smoked cigarette. However, only 66.7% of the respondents knew about smoking related health problems. Moreover, only 46.8% of them mentioned lung cancer as a smoking related health problem (Figure 8).
 |
Figure 8 Proportion of study participants with smoking practice in Wolaita Zone, Ethiopia. |
Discussion
A significant proportion of cancer morbidity and mortality is preventable if people elude the avoidable risk factors and preclude cancer related-infections.13–15 Nearly a third of cancer–related mortality in low income countries (LICs) is assumed to be preventable.28 On the contrary, most of LICs’ cancer patients, including Ethiopians, are presented at advanced stages of the disease where it is difficult to curb the situation. The late presentation of cancer patients is partly attributed to lack of awareness and knowledge, myths and misconceptions of the people about cancer.18,20,21 The myths and misconceptions can only be ended through awareness development by educating society that cancer is neither contagious, a death sentence nor a curse. Thus, the current study was aimed at investigating the awareness and knowledge status of people about cancers and breast and cervical cancers in particular in Wolaita zone, in southern parts of Ethiopia.
The findings from the current study indicated that there existed a modest level of awareness of cancer among the study participants. A similar descriptive, cross-sectional study conducted on 437 Nigerian civil servant women indicated that 55.4% of the study participants knew about cervical cancer.29 Our finding showed that more than a third (34.6%) of the study participants heard about cancer from Mass Media (MM) followed by schools (28.5%) and treating physicians (6.7%). This was also reflected in a study conducted on 120 girls in 6 public schools in Kenya. They showed that schools and MM were predominant sources of information about cervical cancer.30 MM play a key role in the publics’ understanding of health issues, including cancer risks. However, it is important to consider the proportion of the general population of LICs who has access to MM. In addition, the access and availability of college and basic formal schools is also limited in such countries. As a limitation, the current study was also conducted on a population in the working/economically productive age groups with a mean age of 25.19. The increased level of awareness about cancer by the study subjects is partly attributed to their educational status and easy access to MM.31–34 An intensive review conducted by Schliemann et al and original findings therein revealed that educational level of people and access to the MM and small media has a direct impact on the level of awareness and knowledge of people about cancers.35 This study showed limited involvement and role of the frontline health care workers in fighting cancer. Primary care clinicians face competing demands, conflicting guidelines, and lack of systems that support provision of preventive services. However, they are the most trusted people to educate the general population to increase awareness and combat myths and misconceptions of people about cancers.36
Surprisingly, more than half of the study participants (70%) mentioned that they were frightened when they heard about cancer for the first time. This type of unconditional fear about cancer is commonly observed even in advanced countries.37 Cancer is reported to be a disorder that arouses powerful emotions of fear, uncertainty and hopelessness in the general population in many parts of the world.37,38 The views of society and patients about cancer have great impact on the psychosocial status of the patients, in addition to determining the time of presentation and adherence to the treatment.37–39 Our study also indicated that about half of the study participants responded that they feared cancer because they believed that cancer has no cure. Yet, 27.2% of the study participants responded that they developed fear towards cancer due to lack of awareness, indicating the critical importance of educating the general population about cancer. Studies indicated that early presentation and adherence to cancer treatments is partly determined by the status of awareness and knowledge of people about the disease.17,20 More striking is that 14.8% of the study participants believed that cancer is a communicable disease. This has serious negative impact in the outcome of the fight against cancer. It can increase stigma and other psychosocial impressions on patients, their families and attendants. However, it is noteworthy to mention that though cancer itself is not contagious, some viruses and bacteria are contagious and can lead to the development of cancer.13,14
Ethiopia is the second most populous country in Africa, with a population of more than 110 million. The health institution with cancer specialty is scant in the country. Thus, one important awareness area is to increase the knowledge of people about where to go when they need any help concerning cancer. The current study showed that over half (67.4%) of the study participants knew that cancer treatment is available in Ethiopia and nearly the same proportion of the study participants thought that cancer is curable if detected and treated early. Our finding is in contrary to other studies that showed that people have many myths and misconceptions about cancer.40,41 Some of the African studies show that people do not believe in the orthodox treatment; instead they prefer to go to the traditional and religious centers.41 Interestingly, we showed in previous study that most of the cancer patients in Black Lion Specialized Hospital prefer to go to traditional healers and religious centers when they develop cancer.20 Still a large number of people (22.5%) did not have any idea about the place where cancer treatment is provided in the country. Unlike other non-communicable diseases, some patients with cancer are curable through access to earlier and more accurate diagnosis, specialist consultation and appropriate therapeutic means. In addition to the current poor referral systems in the health sectors, different cultural barriers, limited access to the treatment centers and lack of knowledge for the whereabouts of the treatment centers in the country plays crucial role for the outcome of the patients.
The level of awareness of the study participants about the role of smoking and alcohol intake in cancer development was also surveyed. Most of the study participants were naïve about smoking and alcohol intake as attributable factors for cancer development. The proportion of study participants that knew about the association between smoking, alcohol intake and cancer development were 38.6% and 51.5%, respectively. This is a very important area to consider in future study as significant proportion of global cancer epidemiology is attributed to smoking and alcohol intake. In addition to lung cancer, tobacco use increases the risk of developing of at least 14 more types of cancers.15 In addition, more than a quarter of all cancer mortality and 87% of lung cancer deaths are directly or indirectly linked with smoking. In line with our report, national representative household survey of 9765 study participants in Nigeria indicated that the level of awareness of the adverse effects of smoking was low and differed from region to region.42 Alcohol intake has a long history to be associated with many cancers, including breast and cervical cancers.43,44 Recently, a case-control study on more than 2000 cases and control groups in Nigeria, Cameroon and Uganda indicated positive relationship between alcohol consumption and breast cancer risks.45 Another cross-sectional study on 3967 teenagers in 20 high schools in urban and rural Ethiopia showed high prevalence of alcohol consumption.46 Taken together, the present report indicated the potential area of awareness creation for avoidable cancer risk factors in Ethiopia.
Likewise in other African countries, the majority of breast and cervical cancer cases in Ethiopia are detected at advanced and symptomatic stages, where it is less likely to curve the problem. While shortage of diagnostic and treatment services is an important cause of continually high morbidity of cervical and breast cancers in the region, lack of knowledge and awareness about the diseases are playing greater role.20,21 Despite all these facts, our study showed that only 48% and 24.2% of the study participants heard about breast and cervical cancers, respectively. More than a third (36.6%) of the study participants knew a person who had breast cancer whereas only 10.3% of the participants knew a person who developed cervical cancers. In addition, the productive groups of people in this particular study site had poor knowledge about the risk factors and outcomes of breast and cervical cancers. More than 95% of cervical cancers are caused by high risk human papilloma viruses (HRHPV), for which there are globally accepted vaccines and prevention strategies.13–15 The morbidity and mortality from cervical cancer is significantly decreased in high income countries owing to introduction of vaccination, screening programs and advanced awareness of the general population.1,2 On the contrary, cervical cancer is still one of the deadlier cancers in low income countries, including Ethiopia. The fact that only 36.2% of the study participants believed that cervical cancer is caused by HRHPV indicates that public health education and aggressive awareness campaign about cervical cancer is urgently needed in the study area. Primary prevention of cervical cancer with the introduction of the vaccines is one of the incomparable means to reduce morbidity and mortality. But it is also important to indicate that the vaccine and screening uptakes were dependent on the status of awareness and knowledge of people about the causative agents of the diseases.47,48 More striking is that 69.4% of the current study participants had limited knowledge about the mode of transmission of the causative agents of cervical cancer. This has also great public health importance since HPV is mostly transmitted by sexual contacts. Of the study participants that perceived that HPV is transmittable from person to person, only 18.8% believed that it is sexually transmitted. This is still very crucial as far as majority of our study participants had sexual debut in the second decade of their life.
In addition to vaccination for HPV, screening is one of the forefront mechanisms of reducing cervical and breast cancers morbidity and mortality.48 In light of this, the highly decreased morbidity and mortality of breast and cervical cancers in HICs is due to well established screening programs for both cancers.49,50 Of course, the screening and vaccination programs are at infant stages in many parts of low income countries, including Ethiopia.51,52 Our study also showed that only 4.7% of the study participants were screened for cervical cancer. This is partly due to lack of awareness about the importance of screening programs by the study participants. This survey also revealed that the contribution of physicians in informing about cervical and breast cancers is minimal. As a result, only 4.7% of the study participants reported that they knew about the signs and symptoms of cervical cancer. This is similar to the findings of Birhanu and his colleagues that showed very low awareness of cervical cancer existed in the community in south western parts of Ethiopia.7
In addition, sexual behavior of an individual has direct and or indirect association with certain forms of cancer development.53 Thus, the sexual characteristics of the study participants were also explored in this study. From the total study participants, about 49% had reported to be sexually active. From the sexually active individuals, 37.7% had experienced their first sexual intercourse at the age ranging from 20–25. The proportion of sexually active individuals with sexual debut of age between 16–20 years was 29.5%. This is interesting as early age sexual intercourse is one of the important risk factors for the development of cervical cancers.54 Early sexual activity exposes a female to persistent infection with high risk human papillomavirus that cannot be cleared within 2 years. As a result a woman develops different stages of cervical neoplasm in her early age.53,54 The result of the current study also showed that 10.8% of those who had children gave their first birth at the age of less than 18 years, which is also another risk factor for development of cervical cancer.25 Strikingly, more than a third of study participants did not have awareness about sexually transmitted diseases. Among those who had awareness about sexually transmitted disease, only 31.9% of the respondents were found to have awareness about HIV. Fortunately, 90.6% of the study participants had never experienced sexually transmitted disease in their lifetime. This is also crucial from a public health point of view as acquiring sexually transmitted diseases is another risk factor for developing cervical cancers.54 Taken together, an orchestrated prevention strategy involving awareness creation in the general population, building the capacity of the health system and the professionals, enhancing screening and vaccination programs is extremely needed in low income settings, like Ethiopia.
Conclusion and Recommendations
Many reproductive age groups of people in Wolaita zone have limited awareness about cancer in general and cervical and breast cancers in particular. The health professionals in the study area are not acting as the forefront leaders in the battle against cancers. In addition to the introduced HPV-vaccines for school girls in the country, we recommend aggressive actions by the governmental and nongovernmental institutions to raise public awareness about the role of HPV vaccines and cancer screening for reducing mortality and morbidity from cancer. Finally, educating the general population with local language, including the school girls, about cervical and breast cancers will have great impact on curbing the current cancer epidemics in the country. Including cancer education in the curriculum of primary and secondary schools will have profound effect.
Acknowledgment
The authors are grateful to study participants and the data collectors.
Disclosure
We declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
1. Shah SC, Kayamba V, Peek RM, Heimburger D. Cancer control in low- and middle-income countries: is it time to consider screening? J Glob Oncol. 2019;1–8. doi:10.1200/JGO.18.00200
2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics, 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi:10.3322/caac.21492
3. Fitzmaurice C, Allen C, Barber RM, et al.; Global Burden of Disease Cancer Collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3(2):534–548.
4. Bray F. Transitions in human development and the global cancer burden. In: Stewart BW, Wild CP, editors. World Cancer Report 2014. Lyon: IARC Press; 2014:42–55.
5. Bray F, Colombet M, Mery L, et al. Cancer Incidence in Five Continents. Vol. XI (electronic version). Lyon: International Agency for Research on Cancer; 2017.
6. Jha P. Avoidable global cancer deaths and total deaths from smoking. Nat Rev Cancer. 2009;9:655–664. doi:10.1038/nrc2703
7. Ololade KO, Alabi A, Fadipe B, Adegboyega B. The ‘evil arrow’ myths and misconceptions of cancer at Lagos University Teaching Hospital, Nigeria. S Afr J Oncol. 2019;3:a49. doi:10.4102/sajo.v3i0.49
8. Birhanu Z, Abdissa A, Tefera B, et al. Health seeking behavior for cervical cancer in Ethiopia: a qualitative study. Int J Equity Health. 2012;11:83. doi:10.1186/1475-9276-11-83
9. Kishore J, Ahmad I, Kaur R, Mohanta PK. Beliefs and perceptions about cancers among patients attending radiotherapy OPD in Delhi, India. Asian Pac J Cancer Prev. 2008;9(1):155–158.
10. Saeed S, Khan JA, Iqbal N, Irfan S, Shafique A, Awan S. Cancer and how the patients see it; prevalence and perception of risk factors: a cross-sectional survey from a tertiary care centre of Karachi, Pakistan. BMC Public Health. 2019;19:360. doi:10.1186/s12889-019-6667-7
11. Belglaiaa E, Souho T, Badaoui L, et al. Awareness of cervical cancer among women attending an HIV treatment centre: a cross-sectional study from Morocco. BMJ Open. 2018;8:e020343. doi:10.1136/bmjopen-2017-020343
12. Ruff P, Al-Sukhun S, Blanchard C, Shulman LN. Access to Cancer Therapeutics in Low- and Middle-Income Countries. ASCO Educational Book; 2016.
13. Gilani SJ, Khurram M, Mazhar T, et al. Knowledge, attitude and practice of a Pakistani female cohort towards breast cancer. J Pak Med Assoc. 2010;60:205–208.
14. Plummer M, de Martel C, Vignat J, et al. Global burden of cancers attributable to infections in 2012: a synthetic analysis. Lancet Oncol. 2016. doi:10.1016/S2214-109X(16)30143-7
15. Casper C, Fitzmaurice C. Infection-related cancers: prioritising an important and eliminable contributor to the global cancer burden. Lancet Glob Health. 2016;4(9):e580–e581. doi:10.1016/S2214-109X(16)30169-3
16. Anand P, Kunnumakara AB, Sundaram C, et al. Cancer is a preventable disease that requires major lifestyle changes. Pharm Res. 2008;25(9):2097–2116. doi:10.1007/s11095-008-9661-9
17. Shyyan R, Masood S, Badwe RA, et al. Breast cancer in limited-resource countries: diagnosis and pathology. Breast J. 2006;12(Suppl 1):S27–S37. doi:10.1111/j.1075-122X.2006.00201.x
18. Odusanya OO, Tayo OO. Breast cancer knowledge, attitudes and practice among nurses in Lagos, Nigeria. Acta Oncol. 2001;40(844–8):24.
19. Oluwatosin OA, Oladepo O. Knowledge of breast cancer and its early detection measures among rural women in Akinyele Local Government Area, Ibadan, Nigeria. BMC Cancer. 2006;6:271. doi:10.1186/1471-2407-6-271
20. Yohana E, Kamuhabwa A, Mujinja P. Availability and affordability of anticancer medicines at the Ocean Road Cancer Institute in Dar es Salaam, Tanzania. East Afr J Public Health. 2011;8:52–57.
21. Haileselassie W, Mulugeta T, Tigeneh W, Kaba M, Labisso WL. The situation of cancer treatment in Ethiopia: challenges and opportunities. J Cancer Prev. 2019;24:33–42. doi:10.15430/JCP.2019.24.1.33
22. Haileselassie W, Kaba M, ArayaSellasie M, Mulugeta T, Labisso WL. Challenges and opportunities in cancer diagnosis in Ethiopia: in-depth exploration of practitioners’ view. Int J Curr Res. 2017;9:54662–54668.
23. Gemechu T, Labisso WL, Deyessa N. The relative frequency and patterns of solid malignant tumors in Tikur Anbessa specialized teaching hospital: a 10 year histopathology review. Sch J App Med Sci. 2018;6(1D):278–288.
24. Tigeneh W, Molla A, Abreha A, Assefa M. Pattern of cancer in Tikur Anbessa specialized hospital oncology center in Ethiopia from 1998 to 2010. Int J Cancer Res Mol Mech. 2015;1:1. doi:10.16966/2381-3318.103
25. Feuchtner J, Mathewos A, Solomon A, et al. Addis Ababa population-based pattern of cancer therapy, Ethiopia. PLoS One. 2019;14(9):e0219519. doi:10.1371/journal.pone.0219519
26. Getahun F, Mazengia F, Abuhay M, et al. Comprehensive knowledge about cervical cancer is low among women in Northwest Ethiopia. BMC Cancer. 2013;13:2. doi:10.1186/1471-2407-13-2
27. American Cancer Society. Cancer Prevention Study, Questionnaire for Women.Available from:https://www.cancer.org/content/dam/cancer-org/research/epidemiology/cps-I-1959-survey-women.pdf.
28. Global Task Force on Expanded Access to Cancer Care and Control in Developing Countries. (GTF. CCC). Cancer medicine prices in low– and middle–income countries. Boston: Management Sciences for Health; 2011. Available from: http://www.msh.org/sites/msh.org/files/ccd_msh.pdf.
29. Ohaeri B, Ebunu P, Ndikom C. Psycho-social factors influencing cervical cancer screening and human papilloma virus vaccination acceptance among female civil servants in Delta State, Nigeria. J Glob Oncol. 2018;4:21s. doi:10.1200/jgo.18.47800
30. Mburu A, Itsura P, Mabeya H, Kaaria A, Brown D. Knowledge of cervical cancer and acceptability of prevention strategies among human papillomavirus-vaccinated and human papillomavirus-unvaccinated adolescent women in Eldoret, Kenya. J Glob Oncol. 2018;4:196s.
31. Balla BC, Terebessy T, Tóth E, Balázs P. Young hungarian students’ knowledge about HPV and their attitude toward HPV vaccination. Vaccines. 2017;5:1. doi:10.3390/vaccines5010001
32. Chaka B, Sayed A, Goeieman B, Rayne S. A survey of knowledge and attitudes relating to cervical and breast cancer among women in Ethiopia. BMC Public Health. 2018;18:1072. doi:10.1186/s12889-018-5958-8
33. Gürdal SÖ, Saraçoğlu GV, Oran ES, Yankol Y, Soybir GR. The effects of educational level on breast cancer awareness: a cross-sectional study in Turkey. Asian Pac J Cancer Prev. 2012;12:295–300. doi:10.7314/APJCP.2012.13.1.295
34. Liu Y, Zhang J, Huang R, et al. Influence of occupation and education level on breast cancer stage at diagnosis, and treatment options in China a nationwide, multicenter 10-year epidemiological study. Medicine. 2017;96(15):e6641. doi:10.1097/MD.0000000000006641
35. Schliemann D, Su TT, Paramasivam D, et al. Effectiveness of mass and small media campaigns to improve cancer awareness and screening rates in Asia: a systematic review. J Glob Oncol. 2019. doi:10.1200/JGO.19.00011
36. Eguzo K, Kremzier M, Nnah K, Oluoha C, Ekanem U, Ogboso C. Expanding the role of Nigerian primary care providers in cancer control through continuing education: findings from government-led collaborative intervention. J Clin Res Oncol. 2018;1(2):1–6.
37. Vrinten C, van Jaarsveld CHM, Waller J, von Wagner C, Wardle J. The structure and demographic correlates of cancer fear. BMC Cancer. 2014;14(597):1–9. doi:10.1186/1471-2407-14-597
38. Consedine NS, Magai C, Krivoshekova YS, Ryzewicz L, Neugut AI. Fear, anxiety, worry, and breast cancer screening behavior: a critical review. Cancer Epidemiol Biomarkers Prev. 2004;13(4):501–510.
39. Dubayova T, van Dijk JP, Nagyova I, et al. The impact of the intensity of fear on patient’s delay regarding health care seeking behavior: a systematic review. Int J Public Health. 2010;55(5):459–468. doi:10.1007/s00038-010-0149-0
40. Hay JL, Buckley TR, Ostroff JS. The role of cancer worry in cancer screening: a theoretical and empirical review of the literature. Psychooncology. 2005;14(7):517–534. doi:10.1002/pon.864
41. Archibong E, Enang EE, Bassey GE. Witchcraft beliefs in diseases causation and health-seeking behaviour in pregnancy of women in Calabar South-Nigeria. IOSR J Hum Soc Sci. 2017;22:24–28. doi:10.9790/0837-2206042428
42. Adeniyi BO, Ilesanmi OS, Babasola OM, et al. Knowledge of the health consequences of tobacco smoking among Nigerian smokers: a secondary analysis of the Global Tobacco Survey. S Afr Respir J. 2017;2:113–120.
43. Tuyns AJ. Epidemiology of alcohol and cancer. Cancer Res. 1979;39:2840–2843.
44. Martin PM, Hill GB. Cervical cancer in relation to tobacco and alcohol consumption in Lesotho, southern Africa. Cancer Detect Prev. 1984;7:109–115.
45. Qian F, Ogundiran T, Hou N, et al. Alcohol consumption and breast cancer risk among women in three Sub-Saharan African countries. PLoS One. 2014;9(9):e106908. doi:10.1371/journal.pone.0106908
46. Getachew S, Lewis S, Britton J, Deressa W, Fogarty AW. Prevalence and risk factors for initiating tobacco and alcohol consumption in adolescents living in urban and rural Ethiopia. Public Health. 2019;174:118–126. doi:10.1016/j.puhe.2019.05.029
47. Ramogola-Masire D HPV vaccine for cervical cancer prevention in Botswana. Commonwealth Health Partnerships; 2014:81–84.
48. Ibekwe CM, Houqe ME, Ntuli-Ngcobo B. Perceived benefits of cervical cancer screening among women attending Mahalapye District Hospital, Botswana. Asian Pac J Cancer Prev. 2010;11:1021–1027.
49. Hall MT, Smiss KT, Lew J, et al. The projected timeframe until cervical cancer elimination in Australia: a modeling study. Lancet Public Health. 2019;4:e19–e27. doi:10.1016/S2468-2667(18)30183-X
50. Wigle J, Coast E, Watson-Jones D. Human papilloma virus (HPV) vaccine implementation in low and middle-income countries (LMICs): health system experiences and prospects. Vaccine. 2013;31:3811–3817. doi:10.1016/j.vaccine.2013.06.016
51. Arrossi S, Temin S, Garland S, et al. Primary prevention of cervical cancer: american society of clinical oncology resources-stratified guidelines. J Glob Oncol. 2017;3:611–634. doi:10.1200/JGO.2016.008151
52. Binagwaho A, Wagner CM, Gatera M, Karema C, Nutt CT, Ngabo F. Achieving high coverage in Rwanda’s national human papillomavirus vaccination programme. Bull World Health Organ. 2012;90:623–628. doi:10.2471/BLT.11.097253
53. La Vecchia C, Franceschi S, Decarli A, et al. Sexual factors, veneral diseases, and the risk of intraepithelial and invasive cervical neoplasia. Cancer. 1986;58:935–941. doi:10.1002/1097-0142(19860815)58:4<935::AID-CNCR2820580422>3.0.CO;2-O
54. Louie KS, de Sanjose S, Diaz M, et al. Early age at first sexual intercourse and early pregnancy are risk factors for cervical cancer in developing countries. Br J Cancer. 2009;100:1191–1197. doi:10.1038/sj.bjc.6604974
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

