Back to Journals » Nature and Science of Sleep » Volume 16
The Psychometric Properties of the Arabic Version of the Anxiety and Preoccupation About Sleep Questionnaire (APSQ)
Authors Alghamdi AA, Abanumai AA, Althobaiti MF , Alzahrani MS, Abu-Saleh SY, Ammar A , Ghazzawi H, Trabelsi K, Bragazzi N , BaHammam AS , Jahrami H , AlRasheed MM
Received 11 November 2023
Accepted for publication 29 January 2024
Published 2 February 2024 Volume 2024:16 Pages 75—83
DOI https://doi.org/10.2147/NSS.S449354
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sarah L Appleton
Abdulmajeed Abdullah Alghamdi,1 Abdulmalik Abdulrahman Abanumai,1 Meshal Fawaz Althobaiti,2 Meshari Salem Alzahrani,1 Salma Yasser Abu-Saleh,3 Achraf Ammar,4,5 Hadeel Ghazzawi,6 Khaled Trabelsi,7,8 Nicola Bragazzi,9 Ahmed S BaHammam,10,11 Haitham Jahrami,1,12 Maha M AlRasheed13
1Department of Psychiatry, College of Medicine and Medical Sciences, Arabian Gulf University, Manama, Bahrain; 2Department of Medicine, College of Medicine, Taif University, Taif, Saudi Arabia; 3Department Nutrition and Food Technology, Jordan University of Science and Technology, Irbid, Jordan; 4Department of Training and Movement Science, Institute of Sport Science, Johannes Gutenberg-University Mainz, Mainz, Germany; 5Interdisciplinary Laboratory in Neurosciences, Physiology, and Psychology: Physical Activity, Health, and Learning (LINP2), UFR STAPS (Faculty of Sport Sciences), UPL, Paris Nanterre University, Nanterre, France; 6Nutrition and Food Science Department, Agriculture School, The University of Jordan, Amman, Jordan; 7High Institute of Sport and Physical Education of Sfax, University of Sfax, Sfax, Tunisia; 8Research Laboratory: Education, Motricity, Sport and Health, EM2S, LR19JS01, University of Sfax, Sfax, Tunisia; 9Human Nutrition Unit (HNU) and Department of Food and Drugs, University of Parma, Medical School, Building C, Parma, Italy; 10The University Sleep Disorders Center, Department of Medicine, College of Medicine, King Saud University, King Saud University, Riyadh, Saudi Arabia; 11King Saud University Medical City, King Saud University, Riyadh, Saudi Arabia; 12Department of Psychiatry, Government Hospitals, Manama, Bahrain; 13Department of Clinical Pharmacy, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia
Correspondence: Maha M AlRasheed, Department of Clinical Pharmacy, College of Pharmacy, King Saud University, PO Box 2457, Riyadh, 11451, Saudi Arabia, Tel +966-114678707, Fax +966-114677480, Email [email protected]
Background: Insomnia disorder is a common health condition; it has a role in increasing the possibility of developing other psychological disorders, including anxiety and depression. Anxiety and preoccupation with sleep are two examples of common cognitive factors that contribute to the development of chronic insomnia; thus, it is important to have a tool that assesses worry in insomnia. There is no comprehensive psychiatric measure to assess anxiety and preoccupation with sleep in Arabic. We conducted this study to translate, adapt, and validate the Arabic version of the Anxiety and Preoccupation about Sleep Questionnaire (APSQ), providing a reliable psychometric tool to assess concerns regarding sleep within Arabic-speaking communities.
Methods: The translation process of the scale involved several steps, including forward and backward translation. A cross-sectional study was conducted using an online survey completed by 523 participants from various Arabic-speaking countries. Psychometric analysis was performed utilizing the R software, including internal consistency, test-retest reliability, and confirmatory factor analysis. In addition, convergent and divergent against the Athens insomnia scale (AIS) and general anxiety disorder (GAD) were conducted.
Results: The Arabic-translated form of the APSQ expresses excellent internal consistency with a value of 0.91 for both Cronbach’s α and McDonald’s ω. The test-retest reliability of a subsample showed an excellent coefficient of 0.93 (p< 0.01). A good fit of the APSQ was observed by CFI = 0.93, TLI = 0.91, SRMR = 0.05, and RMSEA = 0.1. Convergent and divergent against AIS and GAD showed statistically significant correlations of 0.85 (p< 0.01) and 0.69 (p< 0.01), respectively. Our sample showed a mean APSQ score of 31.28 ± 8.31, and the mean age was 23.62 ± 7.5.
Conclusion: The Arabic APSQ is reliable and valid for measuring anxiety and preoccupation with sleep in Arabic countries. Using translated APSQ for clinical diagnosis and research is currently trustworthy.
Keywords: anxiety, insomnia, sleep quality, daily performance, general health
Introduction
Insomnia disorder is a common health condition that affects a large proportion of the general population.1 It is defined as the inability to fall asleep, stay asleep, or even poor sleep quality that interferes with life.2 A recent systematic review during COVID-19 showed insomnia prevalence rates of 29.7% and 58.4% among the general population and university students, respectively.3 According to Spielman’s 3P model, predisposing factors (eg hyperarousal), precipitating factors (eg stressful life event), and perpetuating factors (eg maladaptive sleep habits) interact to cause and maintain insomnia.4,5 Cognitive factors play a key perpetuating role, as individuals with insomnia tend to have excessive cognitive arousal and sleep-related anxiety.6,7 They may engage in unhelpful thoughts and beliefs about sleep, have an overinvestment in and unrealistic expectations about sleep needs, and catastrophize the consequences of poor sleep.8 This cognitive hyperarousal and sleep-related anxiety lead to selecting maladaptive coping behaviors that paradoxically worsen insomnia.8 Cognitive behavioral therapy for insomnia (CBT-I) addresses both cognitive and behavioral perpetuating factors.9
Chronic insomnia is believed to increase the probability of developing other psychological disorders, such as anxiety and depression, in the future. Other comorbidities, such as diabetes and hypertension, in addition to life-threatening myocardial infarction, are some examples of the subsequent related complications of insomnia.10–12 Insomnia places a substantial financial burden on the economy, with annual costs in the US exceeding $200 billion due to decreased work output and increased absenteeism. On average, employees with insomnia symptoms are absent for 14 workdays and experience 30 additional days of reduced productivity. Considering both direct and indirect costs, the aggregate expense of insomnia is approximately $63.2 billion each year for the American workforce. Anxiety and preoccupation with sleep are two examples of common cognitive factors that contribute to the development of chronic insomnia.13
Tang and Harvey developed the Anxiety and Preoccupation about Sleep Questionnaire (APSQ), which was validated in 2011 by Jansson-Fröjmark. It is a 10-item scale that assesses sleep-related worries. The scale has two factors: the first factor is composed of six items that reflect concerns about the effects of poor sleep, while the second factor is composed of four items that capture fears about the lack of control over sleep. The APSQ has been evaluated for its validity and reliability, and it shows an association between anxiety and sleep quality.14 The APSQ is a useful tool for clinicians since it can monitor the efficacy of cognitive therapy in chronic insomnia.15
In a study conducted in 2019, 750 participants from 14 hospitals in Spain participated in a multi-institutional, prospective, observational study that looked for the prevalence of sleep issues and their potential mediating role in anxiety and depression. The results show that 65% of women reported having sleep issues, approximately 40% reported having depression, and approximately 20% reported having anxious preoccupations. Sleeping difficulty was more common in women than in men. Depression was a predictive factor of anxious preoccupation.16 Another study was performed in Saudi Arabia in 2019. There were 206 responses,17 ninety-five of which (46%) provided comprehensive details about their lifestyle, academic performance, sleep quality, and mental health. The prevalence of poor sleep was 63.2% among students who were not physically active and spent more time looking at screens. Poor sleepers showed better academic performance than adequate sleepers. The prevalence of participants who reported depression, anxiety, or stress was 42%, 53%, and 31%, respectively. There were significant relationships between depression, sleep quality, anxiety, and stress.17 These findings prove that there is a high prevalence of anxiety in the world and in different cultures. The Arab world consists of 22 countries, with a combined population of over 456 million people as of 2021. By translating, adapting, and validating the APSQ into Arabic, this study provides a reliable psychometric tool for assessing sleep-related anxiety and preoccupation in Arabic-speaking populations. Any sleep scale’s elements can have different meanings in different languages, and a scale that works for one society might not be efficient for another. The aim of this study is to translate, adapt, and validate the APSQ into Arabic to provide a reliable psychometric tool to evaluate worrying about sleep in Arabic communities; thus, the scale will be available for clinical assessment and research purposes.
Methods
The Translation
Prior to the translation process, we sought and obtained necessary approvals from the developers of the APSQ, as it is a copyrighted tool. The translation procedure commenced with two bilingual medical professionals translating the APSQ scale from English to Arabic. Subsequently, a different pair of medical experts with proficiency in both languages performed a back-translation of the Arabic version into English to ensure accuracy. Following the initial translation, the newly translated English version of the APSQ was meticulously compared to the original questionnaire. This comparison and refinement process were conducted in several rounds by the collaborators to ensure that the final English translation was consistent and accurately reflected the content of the original APSQ. Furthermore, the Arabic version of the questionnaire was piloted with a group of 30 individuals from the target demographic to assess the clarity and comprehensibility of the items. Following the pilot, feedback was collected regarding the participants’ understanding of the questions and the overall flow of the questionnaire. This feedback was then analyzed, and necessary revisions were made to refine the questionnaire further, ensuring that it was both culturally appropriate and linguistically accurate for the intended population. Following this phase, the questionnaire expressed clarity, and no changes needed to be made to the form.18 Participants who completed the pilot test were excluded from the main analyses as per our study methodology protocol.
Data Collection
The study was conducted online (in October 2023) through advertisements in various social media and messaging programs, including Twitter, Facebook, Instagram, and WhatsApp, across multiple Arabic-speaking countries: Bahrain, Saudi Arabia, Jordan, Tunisia and Jordan. Participants provided an online informed consent and filled a Google form created by the first author. The Google form included demographic data and the APSQ in Arabic form. For the validation, a sample size of 300 was enough, as the sample size followed the rule for the item-to-respondent ratio (1:30) (ie, thirty responses were needed for each item in the questionnaire).19
Several measures were implemented to ensure the integrity and prevent duplicate entries. Duplicate entries were monitored and addressed through various strategies, including checking for repeated patterns in responses and conducting data cleaning procedures to identify and remove any potential duplicate entries. Data quality checks were performed to identify any suspicious or inconsistent responses. The data was reviewed for patterns of random or meaningless answers, response patterns that suggested inattention or lack of effort, or any other indications of data quality concerns. These measures were taken to maintain the ethical standards of the research and ensure the reliability of the analyzed data.
Instruments
Anxiety and Preoccupation with Sleep Questionnaire (APSQ)
The APSQ is constructed and divided into two categories. First, the first one includes the first six items, which focus on determining worries about poor sleep consequences. The second category is the rest of the items, and they focus on determining worries about sleep uncontrollability. Each item is answered by choosing a number from 1 to 5, where 1 = strongly disagree and 5 = strongly agree; thus, the total ranges between 10 and 50.14 Eighty participants were supplied with the questionnaire two times to assess the test-retest reliability for one week between the two data points.
Athens Insomnia Scale (AIS)
It is a designed self-assessment psychometric instrument for quantifying sleep difficulty based on the ICD-10 criteria. It consists of eight items: the first five items focus on induction of sleep, night awakening, final awakening, total duration of sleep, and quality of sleep, while the remaining 3 items focus on well-being, capacity of functioning, and sleepiness during the day. It has good internal consistency with a Cronbach’s alpha of approximately 0.90.20 An AIS cutoff score of 6 considered a suitable threshold for identifying individuals with insomnia symptoms.20
General Anxiety Disorder Scale (GAD-7)
It is a diagnostic tool comprising seven items, with choices ranging between 0 and 3, where 0 = not at all and 3 = nearly every day. The total score ranges between 0 and 21. It is validated to be availably used in two settings: primary care and the general population. It has an acceptable internal consistency with a Cronbach’s alpha of 0.89.21 A GAD-7 score equal to or exceeding 10 can be considered a suitable threshold for identifying individuals with potential cases of anxiety disorders.20
Ethics
Prior to the collection of data, this study was reviewed and approved by the University of Jordan (number: UOJ-REC-23-167). Informed consent was obtained from all participants. Our study fully complied with the principles outlined in the Declaration of Helsinki, ensuring that all aspects of research involving human participants were conducted in accordance with the highest ethical standards.
Statistical Analysis
We employed descriptive statistics to delineate the sample characteristics and succinctly summarize the findings. Central tendency was measured using the mean, and the standard deviation was used for variability. Describe the response distribution for categorical variables using frequencies and percentages. The score of the APSQ was compared between males and females by using the independent sample t-test. Statistical analysis was performed using the R Statistical Foundation (R version 4.2.2). A p value < 0.05 was considered statistically significant. The internal consistency of the Arabic version of the APSQ was assessed using two statistical measures: McDonald’s omega and Cronbach’s alpha. A threshold value greater than 0.75 was established as the criterion for acceptable internal consistency for the scale.22 During the analysis, we examined each item for weak correlations with others to identify any that might be candidates for removal. However, no items exhibited weak correlations or low internal consistency. To assess convergent validity, we employed Pearson’s correlation coefficient, a measure of the strength and direction of association between two variables, to evaluate the relationship between the Arabic APSQ and the AIS23 and GAD-7. Confirmatory factor analysis (CFA) was used to examine the Arabic APSQ factor structure. CFA is a statistical technique employed to test the extent to which the observed data are consistent with a predetermined theoretical framework or model.24 CFA was conducted using a structural equation modeling (SEM) strategy for data examination.25 Assessment of the model’s goodness of fit was performed by using multiple indicators, including Tucker‒Lewis’s index (TLI), comparative fit index (CFI), standardized root mean square residual (SRMR) and root mean square error of approximation (RMSEA). >0.90 values of TLI and CFI, indicating a good fit. Moreover, <0.08 for RMSEA and SRMR represents an acceptable fit.26 The psychometric properties of the Arabic APSQ were evaluated using the Rasch model, which is a form of item response theory (IRT) analysis. This model facilitates the comparison of item difficulty and person ability on a unified scale, complementing the approaches of classical test theory. The Rasch model is a measurement model that specifically positions individuals and items on a continuum of the underlying construct being assessed.27 It is used to find item functionality that is either good or poor and to determine the scale’s working consistency among groups.
Results
A total of 523 participants were involved in our study. Eighty-one percent of them were female, and eighty-three percent were single. The mean age was 23.62 ± 7.5 years, and the mean BMI was 23.29 ± 4.78. The mean APSQ total was 31.28 ± 8.31 (Table 1). The prevalence of insomnia symptoms in our sample was 37% (95% CI 33–41%). The prevalence of anxiety symptoms in our sample was 48% (95% CI 43–52%). An independent samples t-test was conducted to compare the mean scores on the APSQ Total between female and male participants. The results showed that there was no significant difference between the two groups (t-score(521) = 1.47, p = 0.143, Mean difference = 1.35). Descriptive statistics revealed that the mean score for females (31.55 ± 8.41) was slightly higher than that for males (30.20 ± 7.81).
 |
Table 1 Descriptive Results of the Sleep Preoccupation Scale (SPS)/Anxiety and Preoccupation About Sleep Questionnaire (APSQ) n = 523 |
Two values were calculated to determine the internal consistency of the translated APSQ: Cronbach’s α = 0.91 and McDonald’s ω = 0.91. These numbers represent an excellent internal consistency value as the threshold of acceptable value is >0.75, and all items had a value of >0.75, representing accepted internal consistency values; thus, none of the items were suggested to be deleted to have higher values of internal consistency (Table 2).
 |
Table 2 Reliability Analysis Coefficients of the Anxiety and Preoccupation About Sleep Questionnaire (APSQ) n = 523 |
Based on CFA, the goodness of fit of the model was assessed by calculating four values, TLI, CFI, SRMR, and RMSEA, and their results were 0.93 and 0.91 for CFI and TLI, respectively; both represent a good fit, as they are >0.90. Moreover, 0.05 and 0.1 for SRMR and RMSEA, respectively, indicate an acceptable fit (Table 3).
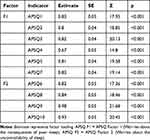 |
Table 3 Confirmatory Factor Analysis of the Anxiety and Preoccupation About Sleep Questionnaire (APSQ) n = 523 |
The convergent translated APSQ showed very good validity against the AIS and against the GAD-7 (Table 4). Specifically, correlation coefficients for: AIS with ASPQ Total (r = 0.63, p < 0.001), AIS with ASPQ Factor 1 (r = 0.59, p < 0.001), and AIS with ASPQ Factor 2 (r = 0.57, p < 0.001). Similarly, GAD-7 showed positive associations with ASPQ Total (r = 0.71, p < 0.001), ASPQ Factor 1 (r = 0.66, p < 0.001), ASPQ Factor 2 (r = 0.66, p < 0.001), and AIS(r = 0.48, p < 0.001).
 |
Table 4 Intercorrelations of the Anxiety and Preoccupation About Sleep Questionnaire (APSQ) and Convergent Validity of the Athens Insomnia Scale (AIS) and Generalized Anxiety Disorders (GAD-7) |
Discussion
Our study aims to evaluate the psychometric properties of the APSQ. The findings support that the Arabic version of the APSQ has high validity and reliability and exhibits high internal consistency. These results suggest that the Arabic translation of the questionnaire is a valid and trustworthy tool for evaluating worry in Arabic-speaking people with insomnia.
The translated form of the APSQ has shown both reliability and validity, as proven by the alpha value and CFA for the hypothesized factor structure fitting the data well, including the following fit indices: CFI, TLI, SRMR, and RMSEA, which either meet or exceed their respective benchmarks. Thus, the suggestion of the APSQ to effectively assess an important and well-defined construct is considered.
This study has a mean APSQ of 31.2 and a standard deviation of 8.31, with an overall reliability of 0.91. The original scale, which was performed in Sweden, had a mean of 13.64, with a standard deviation of 6.4 and an overall reliability of 0.93.14 The Turkish version of the scale had a mean of 41.19 and a standard deviation of 28.67, with an overall reliability of 0.95.28 Our mean is lower than the Turkish and higher than the Swedish. One possible explanation for the variation between the Turkish and Swedish scales is the prevalence of insomnia, which is 12.2% and 10.5%, respectively.
Several factors precipitate the development of insomnia. The identifiable factors can be divided into 5 main categories: health, family, work-school, psychopathology, and others. Pain and medical illness represented 21.8% of all insomnia-related factors within these categories. Stress at work or school accounts for 13.4%, and major affective disorders represent 12.6% of the total factors related to insomnia.29 The higher mean in the previous Turkish version can be attributed to the difference in the selection criteria and the study population,28 since it includes university students who are more likely to be stressed.30 In addition, the involvement of patients who have a major depressive disorder has an association with insomnia. Thus, the scale score correlates with the severity of insomnia.14 However, our study sample was notably different; our sample was the general population, which might justify the reduction in our mean compared to the Turkish version.28 The English version displays a significant variation that can be attributed to several causes.14 For instance, COVID-19 revealed an expanded prevalence of insomnia from 25.4% to 32.2% between 2018 and 2020. This wider variation might account for our higher mean since our study was conducted after the pandemic.31
The observed prevalence of insomnia symptoms in our sample (37%) suggests a significant proportion of individuals experiencing sleep difficulties. This finding aligns with previous research highlighting the widespread nature of insomnia symptoms in the general population.32–35 Further exploration of the factors contributing to the high prevalence of insomnia symptoms in our sample could provide valuable insights for developing targeted interventions and improving sleep health outcomes.
The prevalence of anxiety symptoms in our sample (48%) indicates a considerable burden of anxiety within the population studied. This finding is consistent with existing literature highlighting the pervasive nature of anxiety symptoms in various settings.36–38 Understanding the factors associated with elevated anxiety symptoms in our sample can guide the development of effective interventions and support strategies to alleviate the impact of anxiety on individuals’ well-being and daily functioning. Future research should explore potential risk factors and protective factors contributing to anxiety symptoms, considering their implications for mental health interventions.
One possible explanation for the worldwide increasing incidence of insomnia and preoccupation with sleep is the expanding use of watches/applications that track sleep. As these trackers provide an idea about sleep quality, most users look for perfectionism of sleep quality. This makes them obsessive about their sleep, resulting in insomnia and sleep preoccupation.39
Arabic-speaking societies and other non-English societies need further tools to assess sleep since most of the tools are available in English only.40 Chronic insomnia has been proven to be treated with cognitive therapy, leading to a subsequent reduction in worry that can be evaluated by using the APSQ scale. Depressed patients can also benefit from the treatment of chronic insomnia.41 Insomnia is a common health problem that varies between different societies, making it crucial to investigate disparities.
Correlations between different indices that assess different aspects can provide valuable insights into the relationships between various constructs. In the context of our study, examining the correlations between the APSQ, AIS, and GAD-7 can help us understand the interplay between sleep-related anxiety, insomnia symptoms, and general anxiety symptoms. By exploring these associations, we can gain a deeper understanding of how sleep-related anxiety may relate to insomnia and anxiety symptoms more broadly. This can contribute to our understanding of the unique contributions of each construct and shed light on potential treatment implications. Therefore, while the measures assess different aspects, investigating their correlations can provide valuable information to enhance our understanding of the complex relationships between sleep-related anxiety, insomnia, and general anxiety symptoms.
Strengths and Limitations
Our translated and validated form of the APSQ had several strengths and limitations. Starting with strength, the translation process has been through many expert people in both languages; in addition, they have medical backgrounds, which provide helpful adjustments to the translated form. The rigorous methodology involved a four-step translation process to ensure the accuracy and cultural appropriateness of the Arabic version of the APSQ. The study also employed an acceptable sample size of 523 participants from various Arabic-speaking countries, which enhances the generalizability of the findings. The analysis that has been performed to examine and validate the scale is a very beneficial test for assessing and evaluating the psychometric properties of the questionnaire. Despite its strengths, the study also has some limitations. Using an online survey for data collection may have introduced selection bias, as individuals without internet access or those not active on social media platforms were excluded. Additionally, the study relied on self-reported assessment, which may be subject to response bias. Future studies could benefit from incorporating objective assessments, such as clinical interviews or polysomnography, to corroborate self-reported data.
Conclusions
The Arabic version of the APSQ is a reliable and valid tool for assessing sleep-related anxiety and preoccupation in Arabic-speaking populations. It can be used in clinical and research settings, and it also provides a means to monitor the effectiveness of cognitive therapy for chronic insomnia. The Arabic APSQ also opens up new research avenues, particularly in understanding sleep-related anxiety and its impact on other health outcomes. This could lead to a more holistic approach to healthcare, recognizing sleep as a key factor in overall well-being. The Arabic APSQ is not only a reliable and valid tool for measuring sleep-related anxiety and preoccupation but also a catalyst for future research and clinical practice improvements in the Arabic-speaking world.
Acknowledgments
The authors extend their appreciation to the Deputyship for Research and Innovation, Ministry of Education in Saudi Arabia for funding this research work through project no. (IFKSUOR3-007-3).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Morin CM, Jarrin DC. Epidemiology of insomnia: prevalence, course, risk factors, and public health burden. Sleep Med Clin. 2013;8(3):281–297.
2. Momin RR, Ketvertis K Short term insomnia. 2020.
3. Yuan K, Zheng Y-B, Wang Y-J, et al. A systematic review and meta-analysis on prevalence of and risk factors associated with depression, anxiety and insomnia in infectious diseases, including COVID-19: a call to action. Mol Psychiatry. 2022;27(8):3214–3222. doi:10.1038/s41380-022-01638-z
4. Garland SN, Vargas I, Grandner MA, Perlis ML. Insomnia—behavioral treatments. Manage Sleep Disorders Psychiatr. 2020;4:118.
5. Benz F, Hertenstein E, Johann A, Riemann D. Insomnia disorder—pathophysiology. Manage Sleep Disorders Psychiatr. 2020;4:89.
6. Vaziri Z, Nami M, Leite JP, Delbem ACB, Hyppolito MA, Ghodratitoostani I. Conceptual framework for insomnia: a cognitive model in practice. Front Neurosci. 2021;15:628836. doi:10.3389/fnins.2021.628836
7. Harvey AG, Tang NK, Browning L. Cognitive approaches to insomnia. Clinic Psychol Rev. 2005;25(5):593–611. doi:10.1016/j.cpr.2005.04.005
8. Laidlaw K, Thompson LW, Gallagher-Thompson D, Dick-Siskin L. Cognitive Behaviour Therapy with Older People. John Wiley & Sons; 2003.
9. Williams J, Roth A, Vatthauer K, McCrae CS. Cognitive behavioral treatment of insomnia. Chest. 2013;143(2):554–565. doi:10.1378/chest.12-0731
10. Hu S, Lan T, Wang Y, Ren L. Individual insomnia symptom and increased hazard risk of cardiocerebral vascular diseases: a meta-analysis. Frontiers in Psychiatry. 2021;12:654719. doi:10.3389/fpsyt.2021.654719
11. Fernandez-Mendoza J, Vgontzas AN, Liao D, et al. Insomnia with objective short sleep duration and incident hypertension: the Penn State Cohort. Hypertension. 2012;60(4):929–935. doi:10.1161/HYPERTENSIONAHA.112.193268
12. Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Bixler EO. Insomnia with objective short sleep duration is associated with type 2 diabetes: a population-based study. Diabetes Care. 2009;32(11):1980–1985. doi:10.2337/dc09-0284
13. Bhaskar S, Hemavathy D, Prasad S. Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. J Family Med Prim Care. 2016;5(4):780. doi:10.4103/2249-4863.201153
14. Jansson-Fröjmark M, Harvey AG, Lundh L-G, Norell-Clarke A, Linton SJ. Psychometric properties of an insomnia-specific measure of worry: the anxiety and preoccupation about sleep questionnaire. Cognit Behav ther. 2011;40(1):65–76. doi:10.1080/16506073.2010.538432
15. Harvey AG, Sharpley AL, Ree MJ, Stinson K, Clark DM. An open trial of cognitive therapy for chronic insomnia. Behav Res Ther. 2007;45(10):2491–2501. doi:10.1016/j.brat.2007.04.007
16. Calderon C, Carmona-Bayonas A, Hernandez R, et al. Incidence of sleep problems and their mediating role on depression and anxious preoccupation in patients with resected, non-advanced cancer: data from NEOcoping study. Clin Transl Oncol. 2019;21(8):1104–1107. doi:10.1007/s12094-018-02018-2
17. Al-Khani AM, Sarhandi MI, Zaghloul MS, Ewid M, Saquib N. A cross-sectional survey on sleep quality, mental health, and academic performance among medical students in Saudi Arabia. BMC Res Notes. 2019;12(1):1–5. doi:10.1186/s13104-018-4038-6
18. Awwad O, AlMuhaissen S, Al-Nashwan A, AbuRuz S. Translation and validation of the Arabic version of the Morisky, Green and Levine (MGL) adherence scale. PLoS One. 2022;17:10.
19. Tsang S, Royse CF, Terkawi AS. Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine. Saudi J Anaesthe. 2017;11(Suppl 1):3.
20. Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens insomnia scale: validation of an instrument based on ICD-10 criteria. J Psychoso Res. 2000;48(6):555–560. doi:10.1016/s0022-3999(00)00095-7
21. Löwe B, Decker O, Müller S, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46(3):266–274. doi:10.1097/MLR.0b013e318160d093
22. Bonniga R, Saraswathi DA. Literature review of cronbachalphacoefficient And Mcdonald’s Omega coefficient. Eur J Mol Clin Med. 2020;7:06.
23. Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesthesia Analg. 2018;126(5):1763–1768.
24. Brown TA. Confirmatory Factor Analysis for Applied Research. Guilford publications; 2015.
25. Kelava A. A Review of Confirmatory Factor Analysis for Applied Research. Los Angeles, CA: SAGE Publications Sage CA; 2016.
26. Marsh HW, Guo J, Dicke T, Parker PD, Craven RG. Confirmatory factor analysis (CFA), exploratory structural equation modeling (ESEM), and set-ESEM: optimal balance between goodness of fit and parsimony. Multivar Behav Res. 2020;55(1):102–119. doi:10.1080/00273171.2019.1602503
27. Wilson M. Constructing Measures: An Item Response Modeling Approach. Taylor & Francis; 2023.
28. Uygur ÖF, Orhan FÖ, Uygur H, Kandeger A, Hursitoglu O. Psychometric properties of the Turkish version of the anxiety and preoccupation about sleep questionnaire in clinical and non-clinical samples. Sleep Sci. 2022;15(1):68. doi:10.5935/1984-0063.20210033
29. Bastien CH, Vallières A, Morin CM. Precipitating factors of insomnia. Behav. Sleep Med. 2004;2(1):50–62. doi:10.1207/s15402010bsm0201_5
30. Jiang X-L, Zheng X-Y, Yang J, et al. A systematic review of studies on the prevalence of insomnia in university students. Public Health. 2015;129(12):1579–1584. doi:10.1016/j.puhe.2015.07.030
31. Morin CM, Vézina-Im L-A, Ivers H, et al. Prevalent, incident, and persistent insomnia in a population-based cohort tested before (2018) and during the first-wave of COVID-19 pandemic (2020). Sleep. 2022;45(1):zsab258. doi:10.1093/sleep/zsab258
32. Klimt F, Jacobi C, Brähler E, Stöbel-Richter Y, Zenger M, Berth H. Insomnia symptoms in adulthood. Prevalence and incidence over 25 years. Sleep Med. 2023;109:240–244. doi:10.1016/j.sleep.2023.07.013
33. Ohayon MM, Sagales T. Prevalence of insomnia and sleep characteristics in the general population of Spain. Sleep Med. 2010;11(10):1010–1018. doi:10.1016/j.sleep.2010.02.018
34. Aernout E, Benradia I, Hazo J-B, et al. International study of the prevalence and factors associated with insomnia in the general population. Sleep Med. 2021;82:186–192. doi:10.1016/j.sleep.2021.03.028
35. AlRasheed MM, Fekih-Romdhane F, Jahrami H, et al. The prevalence and severity of insomnia symptoms during COVID-19: a global systematic review and individual participant data meta-analysis. Sleep Med. 2022;3:6.
36. Remes O, Brayne C, Van der linde R, Lafortune L. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain behaV. 2016;6(7):e00497. doi:10.1002/brb3.497
37. Kan FP, Raoofi S, Rafiei S, et al. A systematic review of the prevalence of anxiety among the general population during the COVID-19 pandemic. J Affective Disorders. 2021;293:391–398. doi:10.1016/j.jad.2021.06.073
38. da Silva ML, Rocha RSB, Buheji M, Jahrami H, Cunha Kd C. A systematic review of the prevalence of anxiety symptoms during coronavirus epidemics. J Health Psychol. 2021;26(1):115–125. doi:10.1177/1359105320951620
39. Jahrami H, Trabelsi K, Vitiello MV, BaHammam AS. The tale of orthosomnia: I am so good at sleeping that i can do it with my eyes closed and my fitness tracker on me. Nat Sci Sleep. 2023;15:13–15. doi:10.2147/NSS.S402694
40. Ali RM, Zolezzi M, Awaisu A. A systematic review of instruments for the assessment of insomnia in adults. Nature Sci Sleep. 2020;12:377–409. doi:10.2147/NSS.S250918
41. Gebara MA, Siripong N, DiNapoli EA, et al. Effect of insomnia treatments on depression: a systematic review and meta‐analysis. Depression Anxiety. 2018;35(8):717–731. doi:10.1002/da.22776
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
