Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 16
The Implementation of a Modified Fluid Assessment Tool to Improve the Clinical Assessment, Detection, and Management of Blood Pressure Control and Fluid Alterations Among Hemodialysis Patients
Authors Al Nusair H, Hamdan W, Garma J, Eid A, Alnjadat R , Al-Nsair N, Fonbuena M, Davao C
Received 19 September 2023
Accepted for publication 29 November 2023
Published 11 December 2023 Volume 2023:16 Pages 261—268
DOI https://doi.org/10.2147/IJNRD.S440990
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pravin Singhal
Hussam Al Nusair,1 Wael Hamdan,1 Joy Garma,1 Ahmed Eid,1 Rafi Alnjadat,2 Nezam Al-Nsair,3 Mariezl Fonbuena,1 Christin Davao1
1Dialysis Department, Sheikh Khalifa General Hospital, Umm Al Quwain, United Arab Emirates; 2Applied Health Sciences, Al-Balqa Applied University, Irbid, Jordan; 3College of Nursing, Xavier University, Cincinnati, OH, USA
Correspondence: Rafi Alnjadat, Applied Health Sciences, Al-Balqa Applied University, Irbid, Jordan, Tel +962772496680, Email [email protected]
Background: Fluid overload is a common complication of the care of End-stage Renal Disease patients that may lead to prolonged hospitalization and mortality. This warrants an effective and systemic approach to early recognition and management to improve patient outcomes.
Aim: This study aims to evaluate the effect of a modified fluid assessment tool to improve accurate clinical assessments, detection, and management of blood pressure control and fluid alteration among hemodialysis patients.
Methods: In this retrospective study, data were collected from forty-three dialysis patients who were seen and followed up from a dialysis unit of an acute care hospital during 8 weeks of standard care. A modified assessment tool was used to systematically highlight the appropriateness of the patient set dry weight using intradialytic weight gain (IWDG) and patient blood pressure. Paired sample t-test and repeated measure ANOVA within-group analysis were applied to compare the mean difference score for IDWG and the mean arterial pressure within the study group, respectively.
Result: A total of 43 patients were enrolled (mean age, 59.07) (ranges 27– 88 years) (SD – 14.30); 51.16% female; 79% Emirati Nationals, with Chronic Kidney Disease. A repeated measure ANOVA analysis showed a significant difference in the mean arterial pressure within the study group based on time, over six measurements (p = 0.001). However, the difference between the pre- and post-intra-dialytic weight gain mean scores yields insignificant results (p = 0.346).
Conclusion: The implementation of a modified assessment tool improved blood pressure control, increased staff and physician involvement in assessing patient dry weight facilitated through fluid status evaluation, methodical assessment of dry weight, and precise fluid removal calculation, enhancing overall blood pressure and fluid management in HD patients.
Keywords: hemodialysis, fluid management, fluid assessment, modified assessment tool, chronic kidney disease
Introduction
When chronic kidney disease causes progressive loss of kidney function and reaches an advanced stage, it results in end-stage renal disease (ESRD), or kidney failure. In this stage, dialysis or a kidney transplant is very important to stay alive and meet the body’s functional needs. Nowadays, the hemodialysis (HD) population has been rapidly growing. Although data on the epidemiology of chronic kidney disease and related risk factors in the United Arab Emirates are scarce, Alalawi et al study in Dubai found that the number of patients with end-stage kidney disease (ESRD) on dialysis is increasing worldwide including United Arab Emirates (UAE),1 this makes it a significant clinical and public health concern, accounting for 1.1 million deaths worldwide.2 Several studies also highlighted the importance of Chronic Kidney Disease (CKD) as a risk factor for COVID-19 mortality, a finding that necessitates a call for action.3–5
A growing body of compelling evidence highlighted that the hydration status, as well as the blood pressure of chronic patients undergoing hemodialysis, was two of the key indicators and predictors of patient outcomes.6–9 Risk factors such as over-hydration or fluid depletion are risk factors for mortality and morbidity of patients undergoing hemodialysis.10–13 The accurate assessment of fluid overload is crucial and can be very challenging in clinical practice because this can be subjective or objective. This has led to the use of different techniques, tools, and advanced devices such as handheld ultrasound and bioimpedance spectroscopy (BIS) technology.14–16 However, BIS is often misrepresented in clinically healthy weight.17 Biomarkers can be used like BNP (brain natriuretic peptide), pro-BNP and ANP (atrial natriuretic peptide), ultra-sonographic findings (inferior vena cava collapsibility, lung ultrasonography, carotid artery Doppler, relative blood volume monitoring), and bio-impedance. Each of these methods has its strengths and weaknesses.
The fluid status of dialysis patients should be regularly monitored, and each patient should have a set dry weight as a target for each dialysis treatment. Determining the proper dry weight is crucial because if it is set too high, over-hydrating the patient could cause hypertension, left ventricular hypertrophy (LVH), and potentially left ventricular failure. If it is set too low, the patient could have severe dehydration and hypotension.18
Dry weight is defined as the normal body weight without any extra fluid that builds up between dialysis treatments.19 Dry body weight is important to maintain or normalize blood pressure and prevent further cardiovascular complications. A metric for fluid and salt intake in between the two HD (hemodialysis) sessions is called intra-dialytic weight gain (IDWG). IDWG is calculated as pre-dialysis weight minus post-dialysis weight from the session before HD treatment. It affects HD patients’ survival and blood pressure.20–22
A systematic clinical assessment of fluid status may facilitate early recognition and management of fluid alterations. The study authors believed that improving the quality of care and approach through quality improvement initiatives, evidence-based practice, and clinical experiences is warranted because of the high morbidity and mortality rates among dialysis patients and the lack of rigorous trial data to guide accurate decisions in hemodialysis therapy. This is supported by authors McClellan et al and Nissenson.23,24 The study aims to evaluate the effect of a modified fluid assessment tool (Supplementary Material Appendix I) on improving accurate clinical assessments, detection, and management of blood pressure control and fluid alteration among hemodialysis patients.
Methods
Research Design
Data were extracted from the patient’s session tracker sheet and modified fluid assessment charts of 43 dialysis patients who were scheduled thrice weekly for hemodialysis sessions in a dialysis unit of an acute care hospital in the Northern Emirates from April 1, 2020, to May 30, 2020. Inclusion criteria include all patients enrolled for treatment and hemodialysis sessions during the study period, and patients who were admitted to different hospitals or on vacation during the data collection and monitoring were excluded from the study.
Data Collection and Analysis
During this study, dialysis staff nurses established a special Excel spreadsheet for data collection which includes demographic information such as the age, gender, nationality, and marital status. The presence of comorbidities, compliance with the thrice weekly sessions, IDWG, pre- and post-BP were also collected. Data entry and analysis were performed using the Statistical Package for the Social sciences (SPSS®) version 23. Descriptive statistics analysis was done to evaluate the means, frequency distribution, and standard deviation (SD). Repeated measure ANOVA within-group analysis (Time effect) was applied followed by pairwise comparison with confidence interval adjustment.
Ethical Approval
This study was reviewed and approved by the institutional review board at Al-Balqa Applied University which granted the ethical approval for this study (37/5/7/2341). The relevant guidelines/regulations and informed consent were obtained voluntarily from all participants and/or their legal guardians.
The authors would like also to confirm that the study research was performed in accordance with the Declaration of Helsinki.
Development of the Modified Assessment Tool
As part of standard dialysis unit treatment, patients’ fluid status is closely monitored, dry weight is regularly measured, and fluid removal during hemodialysis sessions is precisely adjusted. For dialysis patients, this procedure is essential for preserving ideal blood pressure levels and avoiding problems brought on by fluid imbalance. An EBP (Evidence-based Practice) team was formed which consisted of five members of the hemodialysis nurses, charge nurse, and Senior Charge Nurse (SCN) in collaboration with the Nephrologists to review the current Fluid Assessment of the Dialysis Flowsheet used in the department. The old fluid assessment/ultrafiltration calculation chart in the dialysis flow sheet entails simple questions and details related to the presence of edema (periorbital and pedal), priming volume, rinse volume, planned weight loss, total oral fluids, total saline (0.9%) boluses, other fluids, and total volume removal. After searching for updated pieces of literature and best study findings related to the fluid assessment tool, the team decided to adopt and modify the assessment tool developed by Fielding et al.25
The physiological parameters in this tool are more comprehensive that include post-dialysis SBP (Systolic Blood Pressure), post-dialysis DBP (Diastolic Blood Pressure), cramps on dialysis, presence of edema at the ankle, number of in-patient days in the last month, and patient appetite. However, there were few modifications made from the adopted tool such as the blood pressure medication list since the complete list of medications is already recorded in the Medication Administration Record of patient’s file. Also, the actions to be carried out for the ongoing assessment table were not included since patients are assessed monthly, or even every two weeks if needed.
Using the modified assessment tool (Supplementary Material Appendix I), staff education and piloting was done for two months by the EBP team through the charge nurse and SCN to all the staff nurses and physicians in the department before its use. Nurses were selected randomly to use the modified tool individually in the fluid assessment of the patient. After the piloting, the form was carefully examined once more for any minor comments and staff feedback and then finalized thereafter. The modified fluid assessment tool was incorporated into the multidisciplinary re-assessment form used on monthly basis to aid the nurses and prompt nephrologists to determine the accurate dry weight of the patient who is undergoing hemodialysis treatment regularly during 8 weeks of standard care. Details about the patient’s dry weight, pre- and post-HD weight, weight gain, IDWG in percentage, and pre- and post-BP were documented and tracked every dialysis session using the dialysis department patient session tracker.
Why and How to Use the Tool?
In using the modified assessment tool (Supplementary Material Appendix I), the nurse has to circle relevant scores in the scoring sheet for each variable under two categories: Overload and Under-load. Depending on the total scores, an action is taken as follows: If the total score is less than −0.5, the action is to increase the target weight by one (1) kg (or increase by 0.5 kg if the current weight is 45 kg or less); no action is required if the total score is between +0.5 and −0.5 and reduce the target weight by one (1) kg (or reduce by 0.5 kg if current target weight is 45 kg or less if the total score is greater than +0.5).
And then based on the desired course of action, the following ongoing assessments should then be carried out: If no action is required, a reassessment should be done in 1 month; if the target weight requires adjustment for the patient who is stable and not on antihypertensive medication, make a change and repeat assessment in 2 weeks; and if the target weight requires adjustment for an unstable patient and/or on antihypertensive medication, then discuss it with the unit consultant.
Results
A total of 43 dialysis patients were enrolled in the study, and the assessment tool (Supplementary Material Appendix I) was used in each patient on monthly basis. Table 1 shows the demographic data for all HD patients. The majority (79%) of the participants were Emirates nationals, mostly (86%) are married and aged above 50 years (69.77%), and with almost equal gender distributions. Almost half (48.83%) of them were having co-morbidities that are well controlled and 62.79% were compliant with their prescribed three times dialysis sessions per week (Table 1).
 |
Table 1 Descriptions of Variables (n-43) |
In Table 2, a pairwise comparison with confidence interval adjustment was performed. The results showed a significant difference in the study group post-implementation. There was a significant difference in the mean arterial pressure within the study group based on time (7.21, p = 0.001). However, there was no significance in the two comparisons of time: MAP April Pre vs MAP May Pre (mean difference = −0.45, 95% CI: −3.26, 2.35; p = 1.000) and MAP April Post vs MAP May Post (mean difference = −1.24, 95% CI (−3.99, 1.52; p = 1.000)). The p-value of the average scores of the IDWG before and after the intervention was <0.346, therefore there is no significant difference in the mean score between trial 1 and trial 2 after the implementation (Table 3).
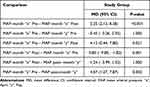 |
Table 2 Comparison of Mean Arterial Pressure (MAP) Within the Study Group Based on Time (Time Effect) |
 |
Table 3 Difference Between the Pre- and Post-Intra-Dialytic Weight Gain Mean Scores |
Discussion
The EBP team aimed to adopt an assessment tool that provides a more comprehensive assessment of the patient’s fluid status compared to the old assessment form used. Specifically, this study aims to evaluate the effect of the modified fluid assessment tool (Supplementary Material Appendix I) on improving accurate clinical assessments, detection, and management of blood pressure control and fluid alteration among hemodialysis patients. It does have the advantage of including variables that might direct the clinicians to further evaluation of the dry weight of the patient is needed. To the author’s knowledge, this is one of the few clinical studies conducted in the United Arab Emirates regarding hemodialysis patients. Utilizing the modified fluid assessment tool (Supplementary Material Appendix I) showed a comparative result between the mean arterial pressure within the study population based on time and the difference between the Pre and Post-intra-dialytic Weight Gain Mean Scores.
The result of the current study indicated a statistical difference in the mean scores of the mean arterial pressure within the study group based on the time when compared between pre - and post-implementation. This could signify that the accurate fluid assessment of patients may have contributed to the management and stability of the patient’s blood pressure as manifested in the patient’s MAP. The average arterial pressure throughout one cardiac cycle is called the mean arterial pressure (MAP). It functions to perfuse blood to all the tissues of the body to keep them functional. As a result, the MAP can be used to detect both hypertension and hypotensive states, as well as to give clinicians the diagnostic data they need to choose the best course of treatment.26
Although the relationship between compliance with treatment sessions and the control of co-morbidities such as BP was not established in our study, the dialysis treatment sessions played a significant role in this significant finding. In the randomized controlled trial conducted by Agarwal et al,27 dry weight reduction yielded BP control of the patient and removal of excess fluid through ultrafiltration, believed to decrease systolic BP. Meanwhile, in another experimental study, results as mean arterial pressure decreased from 110 to 95 mmHg (p < 0.001), systolic BP from 158 to 136 (p < 0.001), and intra-dialytic weight gains were reduced from 3.25 to 1.21L (p < 0.001) signify that volume control with ultrafiltration yields in improved BP control.28 Hence, the study yields a significant difference in the mean arterial pressure due to the utilization of ultrafiltration focusing on the removal of excess fluid from the patient.
From the beginning to the end of the study period, there was no significant difference observed between the study group’s IDWG mean scores. Although fluid management is crucial when performing hemodialysis treatment, numerous factors can be considered, and these impede the actual plan of care. These are nutritional status, duration of dialysis treatment, compliance with the prescribed frequency of treatment, uncontrolled comorbidities (DM, HTN), ultrafiltration rate, and perhaps the dialysis machine settings. Regarding nutritional status, malnutrition can be a cause of mortality in dialysis patients. Therefore, a nutritional assessment is essential to the modality of treatment needed. Thus, control of IDWG in HD patients is of great importance, keeping in mind the importance of the nutritional status of HD patients that may also impact IDWG.29 Furthermore, when the patient is under nutrition it is unlikely to have an accurate dry weight and that could interfere with the precise fluid removal. Also, the two-month trial of implementing the modified tool (Supplementary material Appendix I) in the current study might not be enough to show accurate significant findings.
Dialysis prescriptions such as duration, frequency of hemodialysis treatment, target dry weight as well as machine settings play an important role in fluid management. On the account of a target dry weight prescription, a dry weight that is too low may lead to hypotension, whereas a target weight that is too high may yield hypervolemia. Consequently, increased intradialytic weight in between treatments may also require an extended period of treatment time in order to achieve maximum fluid removal as necessary. Furthermore, in relation to the amount of fluid removal for all the dialysis patients at the unit including the patients involved in the study, the ultrafiltration rate limited to 12.5 cc/kg/hour is considered due to the associated mortality rate of high ultrafiltration rate.30 Responding appropriately to dialysis prescriptions, machine settings like sodium profiling, ultrafiltration profiling, and even dialysate temperature can also contribute to the achievement of the actual care plan.
Estimation of removable excess body fluid of a patient undergoing hemodialysis treatment is a challenging task in the way that it needs an accurate and thorough assessment from healthcare providers such as nurses and nephrologists. Moreover, numerous considerations need to be taken seriously as complications might happen anytime during treatment. Thus, the modified assessment tool (Supplementary Material Appendix I) was implemented as it was believed to be helpful in a systematic clinical judgment of a patient’s fluid status, providing a sense of autonomy for nurses to early recognize any fluid alterations and to compare with the use of Body Composition Monitor (BCM) to accurately determine the accuracy of the dry/target weight prescription. In addition, since the tool provides some actions that need to be taken according to the result of the scoring system, it aids clinicians/nephrologists in accurately prescribing the dry/target weight about their clinical judgments. Finally, the utilization of this assessment tool is paramount to blood pressure and fluid management, hence preventing episodes of fluid overload, hemodynamic instabilities, and lower rates of admissions.
Limitations of our study include a constraint to one entity; thus, the sample size is small, and the result of the current study should be interpreted with caution. Also, we did not collect data such as the presence of cramps, edema, and appetite that are included in the comprehensive assessment tool which may also impact the findings of our study. In the current study, the documented comprehensive assessment of HD patients using a modified fluid assessment tool (Supplementary Material Appendix I) and session tracker sheet during the three times per week sessions of hemodialysis provided a quick look at the previous treatments of patients that includes the following set of readings such as pre- and post-BP pre- and post-weight as well as intra-dialytic weight gain. A well-documented policy may ensure that the approach is consistent as fluid management frequently necessitates feedback from a multidisciplinary team.31 It is recommended that the use of modified fluid assessment tools (Supplementary Material Appendix I) must be continued and standardized in the hospital setting. It is also highly suggested from the nephrologist and nurses’ point of view to increase its utilization, like weekly or bi-monthly instead of monthly, to closely monitor the fluid status of the patients and to have immediate intervention as needed whenever possible.
Our study contributes to a strong support for the proper use of fluid assessment, which will enhance patient care and outcome. Lastly, our study findings indicated that there are other factors influencing the IDWG. Therefore, future studies are required to establish the relationship among these variables. A longitudinal study on a larger population might be needed to know accurately the impact of the modified assessment tool (Appendix I) used in the fluid management of hemodialysis patients.
Conclusion
This is the first study in the UAE to evaluate the impact of an assessment tool among hemodialysis patients. In conclusion, a Modified assessment tool helped with better control of the blood pressure and encouraged more engagement of the staff and physician in evaluating patient dry weight, aid them in the thorough evaluation of fluid status, methodical evaluation of dry weight, and precise calculation of fluid removal, thus helps in the blood pressure and fluid management of HD patients.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgment
We thank the nurses and doctors in the Dialysis Department who participated in this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-to-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Alalawi F, Ahmed M, AlNour H, Noralla M, Alhadari A. Epidemiology of end-stage renal disease in Dubai: single-center data. Saudi J Kidney Dis Transpl. 2017;28(5):1119–1125. PMID: 28937072. doi:10.4103/1319-2442.215126
2. Al-Shamsi S, Regmi D, Govender RD, Cheng X. Chronic kidney disease in patients at high risk of cardiovascular disease in the United Arab Emirates: a population-based study. PLoS One. 2018;13:e0199920. PMID: 29949629; PMCID: PMC6021088. doi:10.1371/journal.pone.0199920
3. Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi:10.1038/s41586-020-2521-4
4. Henry BM, Lippi G. Chronic kidney disease is associated with severe coronavirus disease 2019 (COVID-19) infection. Int Urol Nephrol. 2020;52(6):1193–1194. doi:10.1007/s11255-020-02451-9
5. Gansevoort RT, Hilbrands LB. CKD is a key risk factor for COVID-19 mortality. Nat Rev Nephrol. 2020;16(12):705–706. doi:10.1038/s41586-020-2521-4
6. Turner JM, Peixoto AJ. Blood pressure targets for hemodialysis patients. Kidney Int. 2017;92(4):816–823. doi:10.1016/j.kint.2017.01.038
7. Slabbert A, Chothia MY. The association between office blood pressure and fluid status using bioimpedance spectroscopy in stable continuous ambulatory peritoneal dialysis patients. Clin Hypertens. 2022;28(8). doi:10.1186/s40885-021-00192-0
8. Ruperto M, Sánchez-Muniz FJ, Barril G. Extracellular mass to body cell mass ratio as a potential index of wasting and fluid overload in hemodialysis patients. A case-control study. Clin Nutr. 2020;39(4):1117–1123. doi:10.1016/j.clnu.2019.04.021
9. Kolak E, Radić J, Vučković M, Bučan Nenadić D, Begović M, Radić M. Nutritional and hydration status and adherence to dietary recommendations in dalmatian dialysis patients. Nutrients. 2022;14(17):3553. doi:10.3390/nu14173553
10. Dekker MJE, Kooman JP. Fluid status assessment in hemodialysis patients and the association with outcome. Curr Opin Nephrol Hypertens. 2018;27:188–193. doi:10.1097/MNH.0000000000000409
11. Zoccali C, Moissl U, Chazot C, et al. Chronic Fluid Overload and Mortality in ESRD. J Am Soc Nephrol. 2017;28(8):2491–2497. PMID: 28473637; PMCID: PMC5533242. doi:10.1681/ASN.2016121341
12. Chou JA, Kalantar-Zadeh K, Mathew AT. A brief review of intradialytic hypotension with a focus on survival. Semin Dial. 2017;30:473–480. doi:10.1111/sdi.12627
13. van der Sande F, Kooman J, van der Net J, et al. Pre-dialysis fluid status, pre-dialysis systolic blood pressure and outcome in prevalent haemodialysis patients: results of an international cohort study on behalf of the MONDO initiative. Nephrol Dial Transplant. 2018;33:2027–2034. doi:10.1093/ndt/gfy095
14. Ekinci C, Karabork M, Siriopol D, Dincer N, Covic A, Kanbay M. Effects of volume overload and current techniques for the assessment of fluid status in patients with renal disease. Blood Purif. 2018;46(1):34–47. doi:10.1159/000487702
15. Keane DF, Baxter P, Lindley E, et al. The Body Composition Monitor: a flexible tool for routine fluid management across the haemodialysis population. Biomed Phys Eng Express. 2017;3(3):035017. doi:10.1088/2057-1976/aa6f45
16. Shrestha SK, Ghimire A, Ansari SR, Adhikari A. Use of handheld ultrasound to estimate fluid status of hemodialysis patients. Nepal Med J. 2018;1(2):65–69. doi:10.3126/nmj.v1i2.21584
17. Kim HR, Bae HJ, Jeon JW, et al. A novel approach to dry weight adjustments for dialysis patients using machine learning. PLoS ONE. 2021;16(4):e0250467. doi:10.1371/journal.pone.0250467
18. Mitchell S. Estimated dry weight: aiming for accuracy. Nephrol Nurs J. 2002;29(5):421–428.
19. Scott D What is meant by dry weight in a hemodialysis patient?; 2016. Available from: https://aakp.org/what-is-meant-by-dry-weight-in-A-hemodialysis-patient/.
20. López-Gómez JM, Villaverde M, Jofre R, Rodriguez-Benítez P, Pérez-García R. Interdialytic weight gain as a marker of blood pressure, nutrition, and survival in hemodialysis patients. Kidney Int. 2005;67:S63–S68. doi:10.1111/j.1523-1755.2005.09314x
21. Flythe JE, Curhan GC, Brunelli SM. Disentangling the ultrafiltration rate–mortality association: the respective roles of session length and weight gain. Clin J Am Soc Nephrol. 2013;8(7):1151–1161. CJASN July 2013, 8 (7) 1151-1161. doi:10.2215/CJN.09460912
22. Stefánsson BV, Brunelli SM, Cabrera C, et al. Intradialytic hypotension and risk of cardiovascular disease. Clin J Am Soc Nephrol. 2014;9(12):2124–2132. doi:10.2215/CJN.02680314
23. McClellan WM, Plantinga LC, Wilk AS, Patzer RE. ESRD databases, public policy, and quality of care: translational medicine and nephrology. Clin J Am Soc Nephrol. 2017;12(1):210–216. PMID: 27852663; PMCID: PMC5220648. doi:10.2215/CJN.02370316.
24. Nissenson AR. Improving outcomes for ESRD patients: shifting the quality paradigm. Clin J Am Soc Nephrol. 2014;9(2):430–434. PMID: 24202130; PMCID: PMC3913244. doi:10.2215/CJN.05980613
25. Fielding C, Rhodes C, Fluck RJ. Development of a fluid assessment tool to aid nursing assessment of dry weight.
26. DeMers D, Wachs D. Physiology, mean arterial pressure. In: StatPearls [Internet]. StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK538226/.
27. Agarwal R, Alborzi P, Satyan S, Light RP. Dry-weight reduction in hypertensive hemodialysis patients (DRIP) a randomized, controlled trial. Hypertension. 2009;53(3):500–507. doi:10.1161/HYPERTENSIONAHA.108.125674
28. J JP, Leonard EF, Sandhu G, et al. Daily ultrafiltration results in improved blood pressure control and more efficient removal of small molecules during hemodialysis. Blood Purif. 2012;34:325–331. doi:10.1159/000345334
29. Al Maimani Y, Elias F, Al Salmi I, Aboshakra A, Alla MA, Hannawi S. Interdialytic weight gain in hemodialysis patients: worse hospital admissions and intradialytic hypotension. Open J Nephrol. 2021;11(2):156–170. doi:10.4236/ojneph.2021.112013
30. Assimon MM, Wenger JB, Wang L, Flythe JE. Ultrafiltration rate and mortality in maintenance hemodialysis patients. Am J Kidney Dis. 2016;68(6):911–922. doi:10.1053/j.ajkd.2016.06.020
31. Ashby D, Borman N, Burton J, et al. Renal association clinical practice guideline on haemodialysis. BMC Nephrol. 2019;20:379. doi:10.1186/s12882-019-1527-3
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
