Back to Journals » Nature and Science of Sleep » Volume 15
Serum Zonula Occludens-1 and Claudin-5 Levels in Patients with Insomnia Disorder: A Pilot Study
Authors Fan M , Deng F, Tang R, Cai Y , Zhang X, Li H, Xiang T, Pan J
Received 7 June 2023
Accepted for publication 18 October 2023
Published 31 October 2023 Volume 2023:15 Pages 873—884
DOI https://doi.org/10.2147/NSS.S424756
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Ahmed BaHammam
Mei Fan, Fangyi Deng, Rui Tang, Yixian Cai, Xiaotao Zhang, Hongyao Li, Ting Xiang, Jiyang Pan
Department of Psychiatry, Sleep Medicine Centre, The First Affiliated Hospital, Jinan University, Guangzhou, People’s Republic of China
Correspondence: Jiyang Pan, Department of Psychiatry, Sleep Medicine Centre, The First Affiliated Hospital, Jinan University, 613, West Huangpu Avenue, Guangzhou, 510630, People’s Republic of China, Tel +86 2038688651, Email [email protected]
Purpose: This research aimed to investigate serum Zonula occludens-1 (ZO-1) and Claudin-5 (CLDN5) levels to show whether or not their eventual changes in patients with insomnia disorder could have etiopathogenetic importance. There was no research investigating serum ZO-1 and CLDN5 concentrations in insomnia disorder.
Patients and Methods: This study included 60 insomnia disorder patients and 45 normal controls. None of the patients received drugs for insomnia. The patients completed Insomnia Severity Index (ISI) and Pittsburgh Sleep Quality Index (PSQI), and Polysomnography (PSG) to score the insomnia disorder symptoms. Venous blood samples were collected, and serum ZO-1 and claudin-5 levels were analyzed by enzyme-linked immunosorbent assay (ELISA).
Results: Serum ZO-1 level was significantly higher without a significant difference between age, sex, and body mass index, whereas the difference in serum claudin-5 level between the two groups was not statistically significant. In addition, ZO-1 levels were positively correlated with ISI and PSQI and negatively with N1 and N1_perc. We also demonstrated a positive correlation between the levels of CLDN5 and HAMA, and a negative correlation with total sleep time (TST), N1 and N1_perc.
Conclusion: Our findings suggest an association between these intestinal and brain endothelial permeability markers and insomnia disorders. However, these remain modest and preliminary and need more extensive studies, including long-term follow-up populations and involving gut microbes, to further validate and explore the mechanisms involved.
Keywords: insomnia disorder, blood-brain barrier, intestinal permeability, claudin-5, zonula occludens-1, biomarker
Introduction
Insomnia disorder is one of the common sleep disorders. Epidemiological studies show that 10–15% of the general adult population suffers from insomnia disorder,1 and more than 15% in China,2 characterized by difficulty falling and/or staying asleep, with a duration of more than three months, which can lead to daytime fatigue, low energy, reduced cognitive function,3 and is significantly associated with an increased risk of mood disorders and physical severe illnesses and death,4 and has become a serious social and public health problem because of its profound impact on physical and mental health, quality of life, and social functioning. However, the pathogenesis of insomnia disorder is not yet fully understood. Benzodiazepine (BZD) and non-BZD drugs are commonly used to treat insomnia. However, both often cause drowsiness, dependence, withdrawal symptoms, and other side effects.5 Therefore, further exploration of the underlying pathogenesis of insomnia disorder is vital for the precise treatment of insomnia disorder.
Studies have confirmed that the gut microbiota may play a role in the pathogenesis of insomnia disorders.6–8 Gut flora changed in the stool of clinical insomnia patients,8–10 and evidence from brain imaging studies suggests that gut flora can influence brain function.11,12 The gut microbiome may regulate sleep through the microbiome-gut-brain (BGM) axis.13 The BGM axis has gained increasing attention in research on the biological and physiological basis of psychiatric, neurodevelopmental, aging-related, and neurodegenerative disorders.6,14 Two dynamic barriers regulate signal transduction within the BGM axis: the intestinal mucosal barrier and Blood Brain Barrier (BBB), which consist of endothelial cells interconnected by tight junctions (TJ).15 The intestinal barrier is impaired in various psychiatric disorders.16 Furthermore, it is becoming increasingly clear that, in addition to impaired intestinal barrier, increased blood-brain barrier (BBB) permeability may also be part of the clinical picture in schizophrenia, bipolar disorder, major depression, autism,17,18 and early-onset psychosis.19
Previous markers used to assess blood-brain barrier permeability are more or less limited, such as radiolabeled -mannitol, which requires a radiological license and entails high costs, and Evans blue, which is potentially toxic in vivo and its quantification is unreliable.18 In recent years several studies have shown that peripheral circulating tight junction proteins qualify as potential biomarkers for the assessment of BBB.20,21 Plasma claudin-5 levels are significantly higher in depressed adolescents than in healthy controls and can be sufficient as a diagnostic marker for major depression in adolescents.22
Claudin-5 is the most enriched tight junction protein and a critical integrin that regulates the permeability of BBB 15. In addition, claudin-5 links to cytoplasmic proteins, including ZO-1, ZO-2, and ZO-3, via its carboxyl terminus to form TJ 15. Current studies confirm that claudin-5 dysfunction is associated with psychiatric disorders such as major depression disorder,22 obsessive-compulsive disorder,23 bipolar disorder,24 schizophrenia,25 and neurodegenerative diseases such as Alzheimer’s disease.26 However, no studies have examined the relationship between insomnia disorders and claudin-5.
ZO-1, a 210–225 kDa phosphorylated protein, interacts with occludin, claudins, and ligand adhesion molecules and ZO-2, ZO-3, cingulin, and the actin cytoskeleton. Thus, it plays a crucial role in bringing together several components responsible for the paracellular barrier and attaching tight junction proteins to the cytoskeleton.27 Elevated serum ZO-1 levels have been observed in several gastrointestinal and non-gastrointestinal disorders associated with increased intestinal paracellular permeability due to tight junction dysfunction (eg, celiac disease, inflammatory bowel disease, obesity, and rheumatoid arthritis).28–30 These findings suggest that serum ZO-1 can be used as a marker of intestinal tight junction integrity and intestinal barrier function.30
To our knowledge, serum ZO-1 and claudin-5 concentrations have not been assessed in patients with insomnia disorder. Therefore, in this study, we hypothesized that increased concentrations of ZO-1 and CLDN5 may occur in insomnia disorders and that disease severity may be related to ZO-1 and CLDN5 concentrations in patients with insomnia disorders. Therefore, this study aimed to investigate whether there are differences in serum ZO-1 and CLDN5 concentrations between patients with insomnia disorder and healthy controls.
Materials and Methods
Participants and Procedures
The Medical Ethics Committee of the First Affiliated Hospital of Jinan University (IRB of First Affiliated Hospital of Jinan University, No. KY-2022-167) granted Ethics Committee approval for the study, and we followed the Declaration of Helsinki in conducting the survey. In this study, sixty patients with insomnia disorder from the outpatient clinic of the Sleep Medicine Center of the First Affiliated Hospital of Jinan University were in the insomnia disorder group (INS), and forty-five healthy subjects without any psychiatric disorders were in the normal healthy control group (NC) (Figure 1). Inclusion criteria were (1) Han Chinese, (2) age 18–60 years (including upper and lower limits), (3) long-term living in Guangzhou city, (4) 18.5 kg/m2 ≤BMI ≤ 26.9 kg/m2 (the lower limit of obesity standards in China), and Insomnia Severity Index (ISI) and Pittsburgh Sleep Quality Index (PSQI) scales were used to measure the severity of insomnia symptoms. 17-item Hamilton Depression Scale (HAMD-17); Hamilton Anxiety Scale (HAMA); Generalized Anxiety Disorder (GAD-7) and Patient Health Questionnaire-9 (PHQ-9) were used to measure the mood symptoms.
 |
Figure 1 Participants recruitment flow chart. |
Using the DSM-5 criteria, each patient received a comprehensive diagnostic evaluation by a senior psychiatrist. Patients with any other psychiatric comorbidities were excluded. We carefully evaluated all participants to exclude the presence of autoimmune diseases, pulmonary diseases, infectious diseases, endocrine disorders and treatments, and tumors. In addition, exclusion criteria included (1) co-morbid other sleep disorders, including excessive daytime sleepiness, sleep-related respiratory disorders, sleep-related movement disorders, or sleep circadian rhythm disorders, (2) HAMD-17 score ≥17, HAMA score ≥14, (3) history of regular alcohol consumption, (4) Menstruating, pregnant and lactating women, (5) taking CNS active agents (including sedative-hypnotic, psychotropic drugs) for at least two weeks (or five half-lives) before enrollment. (6) Receiving other insomnia interventions, such as CBT-I.
In addition, body mass index (BMI) is body weight in kilograms divided by the square of height in meters (BMI = kg/m2). Our study obtained written informed consent for participation from the subjects after thoroughly understanding the study details.
Polysomnography (PSG)
All subjects received two consecutive nights of PSG before enrollment, with the first night of PSG to exclude other sleep disorders such as sleep apnea syndrome (SAS) and periodic limb movement disorder (PLMD). Subjects completed polysomnography using a dynamic 64-lead PSG device (Compumedics, Australia) with a continuous recording time of at least 7 hours to assess objective sleep. All sleep recordings were interpreted by the same experienced registered PSG technologist using the American Academy of Sleep Medicine sleep scoring criteria. Sleep physiologic parameters obtained include: Apnea-Hypopnea Index (AHI), Periodic Limb Movement Index (PLMI), Sleep Efficiency (SE), Sleep Latency (SOL), Wake After Sleep Onset (WASO), Total Sleep Time (TST), Duration of sleep stage 1,2,3 and rapid eye movement (N1, N2, N3, and R), Percentage of N1, N2, N3, R in total sleep (N1_perc, N2_perc, N3_perc, R_perc), Arousal Index of total sleep (ArI_total), Arousal Index of REM (ArI_REM) and Arousal Index of Non-Rapid eye movement (ArI_NREM).
Biochemical Analysis
Sample Collection and Pretreatment
Venous blood samples were collected from the anterior elbow vein from 8 am to 10 am on the day following the PSG for patients and controls to determine the serum concentrations of ZO-1 and CLDN-5. Venous blood samples from patients included in the study were taken into biochemical tubes, centrifuged at 3000 rpm for 10 min, and the serum fraction was taken. The obtained serum samples were stored at −80 °C.
Determination of Serum ZO-1 and CLDN5
Levels of human ZO-1 and human claudin-5 were determined using commercial enzyme-linked immunosorbent assay (ELISA) kits (Jiangsu Meimian Industrial Co., Ltd., Jiangsu, China) from the same manufacturer as that used by Guo et al.31 Standards, control sera, and samples are run in duplicate in each assay. Samples were diluted 5-fold at the beginning of the assay. We used a standard concentration-optical density plot to determine the levels of the parameters mentioned in the patient samples, and the results were multiplied by 5. The CLDN5 assay included 5-point calibrators at 7.5 pg/mL, 15 pg/mL, 30 pg/mL, 60 pg/mL, and 120 pg/mL, respectively. Similarly, the human ZO-1 assay includes five spot calibrators at 10 pg/mL, 20 pg/mL, 40 pg/mL, 80 pg/mL, and 160 pg/mL, respectively.
Statistical Analysis
Our data were analyzed on IBM SPSS Statistics software (version 27, IBM Corp., Armonk, NY, USA) and R 4.4.2. The Shapiro–Wilk test was used to assess the normality of data distribution. Normally distributed variables were described as mean ± standard deviation, t-test was used to compare the two groups. Non-normally distributed variables were described as median (interquartile range, IQR), Mann–Whitney test was used for comparison between the two groups. Enumeration data were analyzed by χ2 test, and correlation analysis was performed by partial correlation analysis, with gender, age, and weight as control variables. In the Receiver operating characteristic curve (ROC curve) analysis, binary logistic regression was used to obtain propensity scores to test the discriminatory power of two markers to diagnose insomnia disorder. Multiple comparison tests were performed using the False Discovery Rate (FDR) correction. All tests were two-sided, and differences were considered statistically significant at p < 0.05.
Results
Demographic and clinical variables for each group are summarized in Table 1. As shown in Table 1, there were no significant differences between the two groups regarding age, male-to-female ratio, the prevalence of smoking, Marital status, and BMI. In addition, the lifestyle habits questionnaire found no significant differences in dietary habits, exercise habits, and recent stress between the two groups (Table 2).
 |
Table 1 Demographic and Clinical Characteristics of Patients with Insomnia Disorder (INS) and Normal Controls (NC) |
 |
Table 2 Exercise and Diet Habits |
The sixty patients with insomnia disorder who participated in this study had a minimum duration of 0.25 years and a maximum of 25.0 years since their illness. Compared to normal controls, patients with insomnia disorder had significantly higher ISI (3.00 [4.00] vs 15.00 [5.00], p < 0.001), PSQI (4.00 [2.00] vs 9.00 [3.00], p < 0.001), HAMD (1.00 [6.00] vs 7.00 [5.00], p < 0.01), HAMA (1.00 [3.00] vs 7.00 [3.00], p < 0.001), PHQ-9 (1.00 [3.00] vs 5.00 [5.00], p < 0.001), and GAD-7 (1.00 [3.00] vs 2.00 [6.00], p = 0.049) scores. ESS scores of INS were higher than those of NC, with no significant difference between the two groups. In contrast to the above scales, which assess patients’ subjective sleep, the PSG sleep physiological parameters reflect patients’ objective sleep conditions. Compared with normal controls, patients with insomnia disorder had significantly decreased TST (t=3.158, p= 0.002), SE (Z=−2.911, p= 0.004), duration of N1 (Z=−2.25, p= 0.024), duration of N2 (t=2.171, p= 0.032) and period of R (t=2.147, p= 0.034), and significantly increased WASO (Z=−2.228, p= 0.026), SOL (Z=−2.251, p= 0.024), Wake duration (Z=−2.746, p= 0.006), ArI_total (5.90 [4.70] vs 8.65 [6.00], p= 0.028), and ArI_REM (1.30 [3.50] vs 5.80 [8.40], p< 0.01). The differences in the percentage of each sleep stage between the two groups were not statistically significant (all p-values > 0.05). AHI and PLMI were consistent in INS and NC (p-values =0.435 and 0.867, respectively). These results are mostly consistent with the clinical features of sleep onset and sleep maintenance difficulties in insomnia disorder.32
We measured serum CLDN5 and ZO-1 concentrations using ELISA. ZO-1 was significantly elevated (117.29 [107.24] pg/mL in INS, 90.50 [52.69] pg/mL in NC, P=0.002). Although there was a higher level of CLDN5 in INS (143.74 [101.06] pg/mL in INS, 114.69 [85.69] pg/mL in NC) compared to NC, there was no significant difference (P = 0.368) (Table 3 and Figure 2).
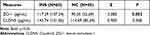 |
Table 3 Serum Zonula Occludens-1 and Claudin-5 Levels of Patients with Insomnia Disorder and Controls |
 |
Figure 2 Boxplot representing the distribution of serum (A) CLDN5 and (B) ZO-1 concentration in insomnia disorder (INS) and normal controls (NC). **P < 0.01. Abbreviation: ns, no significance. |
We performed a partial correlation analysis to understand the correlation between serum CLDN5, ZO-1 and clinical characteristics (Figure 3). ZO-1 levels positively correlated with ISI, PSQI, HAMA, and HAMD for the scales, while CLDN5 levels only positively correlated with HAMA. For PSG, ZO-1 levels negatively correlated with N1 and N1_perc, and CLDN5 levels positively correlated with N3_perc and negatively correlated with TST, N1 and N1_perc.
We performed ROC curve analysis using propensity scores from binary regression to quantify the diagnostic performance of the two markers (ZO-1 and claudin-5) with age, sex, BMI, and HAMA and HAMD as covariates. The ability of markers CLDN5 and ZO-1 to discriminate patients with insomnia disorders from the average population both decreased after adjustment for age, sex, and BMI, but after adjustment for HAMA and HAMD, the AUC value for marker zo-1 increased to 0.882, but not for CLDN5 (Figure 4).
 |
Figure 4 ROC curve. Adjusteda: adjusted for age, gender and BMI. Adjustedb: adjusted for age, gender, BMI, HAMA and HAMD. |
Discussion
To our knowledge, this is the first study on serum ZO-1 and claudin-5, markers of intestinal and brain endothelial permeability, in insomnia disorder. The main findings of our study were that ZO-1 levels were significantly higher in patients with insomnia disorder than in controls and that although levels of the tight junction protein claudin-5 were higher in patients with insomnia disorder than in controls, the difference between the two groups was not significant. In addition, correlation analysis showed that both correlated with clinical symptoms of insomnia disorder.
CLDN5 and the TJs-associated protein ZO-1 are the main components of TJs in the blood-brain barrier. Detecting circulating tight junction proteins is a new approach to assessing the integrity of endothelial TJs.21,33
Studies have shown that CLDN5 is closely associated with psychiatric disorders. Reduced claudin-5 levels have been observed in both the cadaveric brain and serum of schizophrenic patients,34 and claudin-5 polymorphisms are associated with the risk of schizophrenia.35,36 In depressed patients and male mice, CLDN5 expression is reduced in the nucleus accumbens (NAc),37 and serum claudin-5 levels are significantly elevated in bipolar disorder, suggesting a role for the blood-brain barrier in the pathogenesis of bipolar disorder.24 Similarly, elevated serum claudin-5 levels have been observed in patients with Obsessive-compulsive disorder (OCD) and Attention deficit hyperactivity disorder (ADHD).23,38 Our findings showed that serum ZO-1 concentrations were higher in patients with insomnia disorder compared to normal controls.
Furthermore, we found that ZO-1 levels positively correlated with Sleep Assessment Scale scores. Patients with insomnia disorder often have sleep fragmentation, which may lead to disruption of the blood-brain barrier.39 Similarly, the present study found that patients with insomnia had significantly higher WASO and significantly reduced TST, N1, and N2 phase times. TST, N1, N1_perc and N3_perc negatively correlated with ZO-1 or CLDN5 levels. In addition, sleep fragmentation was associated with changes in the abundance of SCFA-producing flora (predominantly Firmicutes) in the gut,40 with an increase in Bacteroidetes and a decrease in Firmicutes in patients with insomnia disorders9,10 and sleep quality was positively correlated with the higher relative abundance of butyrate-producing flora.41 In addition, animal studies have shown that interventions targeting short-chain fatty acids increase NREM sleep42 and sleep duration.43 Fock Ekaterina and Rimma Parnova suggested that SCFA produced by intestinal microbiota regulates tight junction protein ZO-1 and claudin-5 expression directly or by suppressing peripheral inflammation with a protective effect on BBB.44 The above findings suggest the presence of an impaired blood-brain barrier in patients with insomnia disorder, which may be related to the etiology of insomnia disorder. On the other hand, chronic sleep deprivation can also lead to impaired blood-brain barrier function by mechanisms including increased inflammatory mediators and down-regulation of tight junction proteins, such as TNF-α and IL-6, leading to reduced and mislocalized ZO-1 expression.45 Therefore, the causal relationship between ZO-1 levels and disease may be unclear.
Depression and anxiety are two common symptoms in patients with insomnia disorders,46 and their common pathological mechanisms involve the dysregulation of inflammatory factors and neurotransmitter systems.47,48 Indeed, our findings showed that although HAMA and HAMD scores of patients did not reach the diagnosis of depressive-anxiety disorder, they were significantly higher than normal controls, suggesting the presence of mood problems in patients with insomnia disorder. Our correlation analysis also showed that serum ZO-1 levels positively correlated with HAMA and HAMD, and the CLDN5 positively correlated with HAMA. The CLDN5 indicator was significantly reduced, and the ZO1 indicator was significantly increased in AUC after adjustment for HAMA and HAMD in the ROC analysis, suggesting that CLDN5 is associated with anxiety and depression. These correlations may be explained by the interaction of the blood-brain barrier with inflammatory factors.49 Furthermore, claudin-5 levels were significantly elevated in depressed patients and negatively correlated with TNFα, suggesting that there may be a specific interaction between claudin-5 and inflammatory markers in the pathogenesis of depression.50 These findings indicate that blood-brain barrier endothelial dysfunction is associated with mood and insomnia symptoms in patients with insomnia disorder, indirectly suggesting that targeting blood-brain barrier endothelial dysfunction is a potential novel intervention strategy to improve the clinical signs of insomnia disorder by modulating the levels of these markers. However, no studies have reported changes in blood-brain barrier-related markers claudin-5 and ZO-1 levels in patients with insomnia disorder.
In contrast to claudin-5, which is abundantly expressed in the blood-brain barrier, ZO-1 is also one of the major proteins that constitute the intercellular junctions in the intestinal epithelium. Since the structure and function of ZO-1 are closely related to other members of TJs, the position of TJs, in most cases, is altered with the disruption of ZO-1. Therefore, ZO-1 has been used as an indicator and marker to observe various tissues’ barrier function and permeability.21,29,30 Our results also found that elevated serum ZO-1 levels positively correlated with PSQI and ISI but also, to some extent, suggest intestinal mucosal barrier damage may be present in patients with insomnia disorders.
Although the correlations between CLDN5 and ZO-1 and some clinical symptoms of insomnia disorders in the correlation analyses were weak, they were both significant, suggesting that they are associated with insomnia disorders. In the ROC curves, the covariate-adjusted AUC value of ZO-1 was 0.883, sufficient to make ZO-1 biomarkers. However, Large and longitudinally tracked populations may ensure more reliable results.
Although the insomnia disorder group included in our study was unmedicated or had not taken medication for at least two weeks recently, excluding the effect of drugs, and there were no significant differences between the insomnia disorder group and normal controls in terms of age, sex, weight, and lifestyle habits (exercise and diet). However, several limitations should also be considered. First, we did not test the gut microbiota. Second, the relatively small sample size may prevent the generalization of the study results, for example, the participants in this study were relatively young and did not include an older population. Third, our results that ZO-1 and CLDN5 correlate with subjective sleep (PSQI and ISI) but not with objective sleep measures of PSG major parameters (SOL and WASO) may require us to consider insomnia disorder subtypes further. Finally, the cross-sectional nature of the study is a significant limitation. It did not allow us to find any causal relationship for our findings. Larger samples, cohort studies, and animal studies are needed to validate further and further explore the mechanisms of impaired endothelial function in developing insomnia disorders.
Conclusion
These findings suggest that ZO-1 and CLDN5 alterations play an essential role in the pathology of insomnia disorders and may be clinical markers of insomnia disorders. Regardless of the limitations, combined with our results, impaired endothelial barrier in the intestine and brain, especially ZO-1 and CLDN5, may be related to the etiology of insomnia disorders. However, more detailed and comprehensive cohort studies or Zoological and cytological experiments are highly needed to validate further and explore the mechanisms of impaired endothelial function in the development of insomnia disorders.
Acknowledgments
We would like to thank all the participants for their time and efforts.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Key R&D Program of China (Grant No.: 2022YFC2503902) and the National Natural Science Foundation of China (Grant No.: 8187050617).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Roth T. New developments for treating sleep disorders. J Clin Psychiatry. 2001;62(Suppl 10):3–4.
2. Morin CM, Benca R. Chronic insomnia. Lancet. 2012;379(9821):1129–1141. doi:10.1016/S0140-6736(11)60750-2
3. Edinger JD, Bonnet MH, Bootzin RR, et al. Derivation of research diagnostic criteria for insomnia: report of an American Academy of Sleep Medicine Work Group. Sleep. 2004;27(8):1567–1596. doi:10.1093/sleep/27.8.1567
4. Buysse DJ. Insomnia. JAMA. 2013;309(7):706–716. doi:10.1001/jama.2013.193
5. Perlis ML, Posner D, Riemann D, Bastien CH, Teel J, Thase M. Insomnia. Lancet. 2022;400(10357):1047–1060. doi:10.1016/S0140-6736(22)00879-0
6. Wang Z, Wang Z, Lu T, et al. The microbiota-gut-brain axis in sleep disorders. Sleep Med Rev. 2022;65:101691. doi:10.1016/j.smrv.2022.101691
7. Wagner-Skacel J, Dalkner N, Moerkl S, et al. Sleep and microbiome in psychiatric diseases. Nutrients. 2020;12(8):2198. doi:10.3390/nu12082198
8. Smith RP, Easson C, Lyle SM, et al. Gut microbiome diversity is associated with sleep physiology in humans. PLoS One. 2019;14(10):e0222394. doi:10.1371/journal.pone.0222394
9. Liu B, Lin W, Chen S, et al. Gut microbiota as an objective measurement for auxiliary diagnosis of insomnia disorder. Front Microbiol. 2019;10:1770. doi:10.3389/fmicb.2019.01770
10. Li Y, Zhang B, Zhou Y, et al. Gut microbiota changes and their relationship with inflammation in patients with acute and chronic insomnia. Nat Sci Sleep. 2020;12:895–905. doi:10.2147/NSS.S271927
11. Feng Y, Fu S, Li C, et al. Interaction of gut microbiota and brain function in patients with chronic insomnia: a Regional Homogeneity Study. Front Neurosci. 2021;15:804843. doi:10.3389/fnins.2021.804843
12. Chen Z, Feng Y, Li S, et al. Altered functional connectivity strength in chronic insomnia associated with gut microbiota composition and sleep efficiency. Front Psychiatry. 2022;13:1050403. doi:10.3389/fpsyt.2022.1050403
13. Li Y, Hao Y, Fan F, Zhang B. The role of microbiome in insomnia, circadian disturbance and depression. Front Psychiatry. 2018;9:669. doi:10.3389/fpsyt.2018.00669
14. Shin C, Kim Y-K. Microbiota-gut-brain axis: pathophysiological mechanism in neuropsychiatric disorders. Adv Exp Med Biol. 2023;1411:17–37. doi:10.1007/978-981-19-7376-5_2
15. Wettschureck N, Strilic B, Offermanns S. Passing the vascular barrier: endothelial signaling processes controlling extravasation. Physiol Rev. 2019;99(3):1467–1525. doi:10.1152/physrev.00037.2018
16. Wasiak J, Gawlik-Kotelnicka O. Intestinal permeability and its significance in psychiatric disorders - A narrative review and future perspectives. Behav Brain Res. 2023;448:114459. doi:10.1016/j.bbr.2023.114459
17. Kealy J, Greene C, Campbell M. Blood-brain barrier regulation in psychiatric disorders. Neurosci Lett. 2020;726:133664. doi:10.1016/j.neulet.2018.06.033
18. Kadry H, Noorani B, Cucullo L. A blood-brain barrier overview on structure, function, impairment, and biomarkers of integrity. Fluids Barriers CNS. 2020;17(1):69. doi:10.1186/s12987-020-00230-3
19. Wang X, Ma L, Luo Y, et al. Increasing of blood brain barrier permeability and the association with depression and anxiety in systemic lupus erythematosus patients. Front Med. 2022;9:852835. doi:10.3389/fmed.2022.852835
20. Thal SC, Luh C, Schaible EV, et al. Volatile anesthetics influence blood-brain barrier integrity by modulation of tight junction protein expression in traumatic brain injury. PLoS One. 2012;7(12):e50752. doi:10.1371/journal.pone.0050752
21. Zhu JC, Si MY, Li YZ, et al. Circulating tight junction proteins mirror blood-brain barrier integrity in leukaemia central nervous system metastasis. Hematol Oncol. 2017;35(3):365–373. doi:10.1002/hon.2289
22. Wu H, Wang J, Teng T, et al. Biomarkers of intestinal permeability and blood-brain barrier permeability in adolescents with major depressive disorder. J Affect Disord. 2023;323:659–666. doi:10.1016/j.jad.2022.11.058
23. Kılıç F, Işık Ü, Kumbul Doğuç D. Serum Claudin-5, but not zonulin, may be associated with obsessive-compulsive disorder. Psychiatr Danub. 2022;34(2):273–278. doi:10.24869/psyd.2022.273
24. Kılıç F, Işık Ü, Demirdaş A, Doğuç DK, Bozkurt M. Serum zonulin and claudin-5 levels in patients with bipolar disorder. J Affect Disord. 2020;266:37–42. doi:10.1016/j.jad.2020.01.117
25. Usta A, Kılıç F, Demirdaş A, Ü I, Doğuç DK, Bozkurt M. Serum zonulin and claudin-5 levels in patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2021;271(4):767–773. doi:10.1007/s00406-020-01152-9
26. Zhu N, Wei M, Yuan L, et al. Claudin-5 relieves cognitive decline in Alzheimer’s disease mice through suppression of inhibitory GABAergic neurotransmission. Aging. 2022;14(8):3554–3568. doi:10.18632/aging.204029
27. Itoh M, Nagafuchi A, Yonemura S, Kitani-Yasuda T, Tsukita S, Tsukita S. The 220-kD protein colocalizing with cadherins in non-epithelial cells is identical to ZO-1, a tight junction-associated protein in epithelial cells: cDNA cloning and immunoelectron microscopy. J Cell Biol. 1993;121(3):491–502. doi:10.1083/jcb.121.3.491
28. Fasano A. Intestinal permeability and its regulation by zonulin: diagnostic and therapeutic implications. Clin Gastroenterol Hepatol. 2012;10(10):1096–1100. doi:10.1016/j.cgh.2012.08.012
29. Wells JM, Brummer RJ, Derrien M, et al. Homeostasis of the gut barrier and potential biomarkers. Am J Physiol Gastrointest Liver Physiol. 2017;312(3):G171–G193. doi:10.1152/ajpgi.00048.2015
30. Assimakopoulos SF, Akinosoglou K, de Lastic A-L, Skintzi A, Mouzaki A, Gogos CA. The prognostic value of endotoxemia and intestinal barrier biomarker ZO-1 in bacteremic sepsis. Am J Med Sci. 2020;359(2):100–107. doi:10.1016/j.amjms.2019.10.006
31. Guo M, Du C, Li B, Yao R, Tang Y, Jiang Y, Liu H, Su H, Zhou Y, Wang L, Yang X, Zhou M, Yu W. Reducing particulates in indoor air can improve the circulation and cardiorespiratory health of old people: A randomized, double-blind crossover trial of air filtration. Sci Total Environ. 2021;798:149248.
32. Baglioni C, Regen W, Teghen A, et al. Sleep changes in the disorder of insomnia: a meta-analysis of polysomnographic studies. Sleep Med Rev. 2014;18(3):195–213. doi:10.1016/j.smrv.2013.04.001
33. Kazmierski R, Michalak S, Wencel-Warot A, Nowinski WL. Serum tight-junction proteins predict hemorrhagic transformation in ischemic stroke patients. Neurology. 2012;79(16):1677–1685. doi:10.1212/WNL.0b013e31826e9a83
34. Nishiura K, Ichikawa-Tomikawa N, Sugimoto K, et al. PKA activation and endothelial claudin-5 breakdown in the schizophrenic prefrontal cortex. Oncotarget. 2017;8(55):93382–93391. doi:10.18632/oncotarget.21850
35. Guo Y, Singh LN, Zhu Y, et al. Association of a functional Claudin-5 variant with schizophrenia in female patients with the 22q11.2 deletion syndrome. Schizophr Res. 2020;215:451–452. doi:10.1016/j.schres.2019.09.014
36. Greene C, Kealy J, Humphries MM, et al. Dose-dependent expression of claudin-5 is a modifying factor in schizophrenia. Mol Psychiatry. 2018;23(11):2156–2166. doi:10.1038/mp.2017.156
37. Menard C, Pfau ML, Hodes GE, Kana V, Wang VX, Bouchard S, Takahashi A, Flanigan ME, Aleyasin H, LeClair KB, Janssen WG, Labonté B, Parise EM, Lorsch ZS, Golden SA, Heshmati M, Tamminga C, Turecki G, Campbell M, Fayad ZA, Tang CY, Merad M, Russo SJ. Social stress induces neurovascular pathology promoting depression. Nat Neurosci. 2017;20:1752–1760.
38. Aydoğan Avşar P, Ü I, Aktepe E, Kılıç F, Doğuç DK, Büyükbayram H. Serum zonulin and claudin-5 levels in children with attention-deficit/hyperactivity disorder. Int J Psychiatry Clin Pract. 2021;25(1):49–55. doi:10.1080/13651501.2020.1801754
39. Hurtado-Alvarado G, Domínguez-Salazar E, Pavon L, Velázquez-Moctezuma J, Gómez-González B. Blood-brain barrier disruption induced by chronic sleep loss: low-grade inflammation may be the link. J Immunol Res. 2016;2016:4576012. doi:10.1155/2016/4576012
40. Maki KA, Burke LA, Calik MW, et al. Sleep fragmentation increases blood pressure and is associated with alterations in the gut microbiome and fecal metabolome in rats. Physiol Genomics. 2020;52(7):280–292. doi:10.1152/physiolgenomics.00039.2020
41. Grosicki GJ, Riemann BL, Flatt AA, Valentino T, Lustgarten MS. Self-reported sleep quality is associated with gut microbiome composition in young, healthy individuals: a pilot study. Sleep Med. 2020;73:76–81. doi:10.1016/j.sleep.2020.04.013
42. Szentirmai É, Millican NS, Massie AR, Kapás L. Butyrate, a metabolite of intestinal bacteria, enhances sleep. Sci Rep. 2019;9(1):7035. doi:10.1038/s41598-019-43502-1
43. Yu L, Han X, Cen S, et al. Beneficial effect of GABA-rich fermented milk on insomnia involving regulation of gut microbiota. Microbiol Res. 2020;233:126409. doi:10.1016/j.micres.2020.126409
44. Fock E, Parnova R. Mechanisms of Blood-brain barrier protection by microbiota-derived short-chain fatty acids. Cells. 2023;12(4):657.
45. Cuddapah VA, Zhang SL, Sehgal A. Regulation of the blood-brain barrier by circadian rhythms and sleep. Trends Neurosci. 2019;42(7):500–510. doi:10.1016/j.tins.2019.05.001
46. Luo C, Zhang J, Pan J. One-year course and effects of insomnia in rural Chinese adolescents. Sleep. 2013;36(3):377–384. doi:10.5665/sleep.2454
47. Plante DT, Jensen JE, Schoerning L, Winkelman JW. Reduced γ-aminobutyric acid in occipital and anterior cingulate cortices in primary insomnia: a link to major depressive disorder? Neuropsychopharmacology. 2012;37(6):1548–1557. doi:10.1038/npp.2012.4
48. Blake MJ, Trinder JA, Allen NB. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: implications for behavioral sleep interventions. Clin Psychol Rev. 2018;63:25–40. doi:10.1016/j.cpr.2018.05.006
49. Zhao Y, Gan L, Ren L, Lin Y, Ma C, Lin X. Factors influencing the blood-brain barrier permeability. Brain Res. 2022;1788:147937. doi:10.1016/j.brainres.2022.147937
50. Hochman E, Taler M, Flug R, et al. Serum claudin-5 levels among patients with unipolar and bipolar depression in relation to the pro-inflammatory cytokine tumor necrosis factor-alpha levels. Brain Behav Immun. 2023;109:162–167. doi:10.1016/j.bbi.2023.01.015
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

