Back to Journals » Drug, Healthcare and Patient Safety » Volume 15
Prevalence and Determinants of Household Medication Storage During the COVID-19 Outbreak in Southwest Ethiopia
Authors Kahssay SW , Hammeso WW , Getachew D , Woldeselassie BD
Received 15 October 2022
Accepted for publication 25 December 2022
Published 19 January 2023 Volume 2023:15 Pages 1—11
DOI https://doi.org/10.2147/DHPS.S392564
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Siew Siang Chua
Semere Welday Kahssay,1 Workineh Woldeselassie Hammeso,2 Dawit Getachew,3 Behailu Dessalegn Woldeselassie4
1Department of Pharmacognosy and Pharmaceutical Chemistry, School of Pharmacy, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan-Aman, Ethiopia; 2Department of Pharmacy, College of Health Sciences and Medicine, Dilla University, Dilla, Ethiopia; 3Department of Epidemiology and Biostatistics, School of Public Health, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan-Aman, Ethiopia; 4Department of Statistics, College of Natural and Computational Sciences, Dilla University, Dilla, Ethiopia
Correspondence: Semere Welday Kahssay, Department of Pharmacognosy and Pharmaceutical Chemistry, School of Pharmacy, College of Medicine and Health Sciences, Mizan-Tepi University, P.O.Box 5140-260, Mizan-Teferi, Ethiopia, Tel +251904296810, Email [email protected]
Background: Most households worldwide keep medicines on hand for various reasons, including emergency use, treatment of acute and chronic diseases, and anticipated future use. Being infected or fear of getting COVID-19 in the current pandemic could increase the storage of drugs at home. Thus, this study aimed to assess the prevalence of household storage of medicines and associated factors in southwest Ethiopia during the COVID-19 outbreak.
Methods: A cross-sectional household survey was conducted from February 1 to May 30, 2022. Data on the extent of storage, storage conditions, their current status, disposal methods, among others, were collected through structured interviews and observations. The data were entered into EPI info, exported, and analyzed using Statistical Packages for Social Sciences (SPSS). Bivariate followed by multivariate logistic regression was used to identify associated factors. P-value < 0.05 was used as a cut-off point to decide statistical significance.
Results: The magnitude of household medication storage was 48% (95% CI). Analgesics (28.7%) and antibacterial (21.1%) agents were the most predominant class of drugs stored in the households. The most significant proportion of the home-stored medications (34.7%) was reserved for future use, and 31.8% were for treating current medical conditions. The majority of the respondents (84.1%) had never heard/learned about the safe disposal ways of drugs. The presence of children aged less than 5 years in a household [AOR = 1.90 (1.19, 3.05)] and the existence of chronically sick patients in a household [AOR = 4.3 (2.25, 8.45)] were factors significantly associated with household medication storage.
Conclusion: The current study revealed a high prevalence of home medication storage; thus, to lessen or eliminate the negative consequences of storing medications at home, it is necessary to review the medication utilization chain and offer community-based training on proper medication storage and disposal techniques, including establishing take-back programs.
Keywords: medication storage, disposal, COVID-19, household, southwest Ethiopia
Background
Medicines are kept on hand in most households for different reasons, including emergency use and treatment of acute and/or chronic disorders. In addition, treatment change, non-adherence/death, the high cost of medicines, lack of knowledge on appropriate medication disposal methods, and saving medicines for future use are common reasons for patients to keep medicines at home.1,2
Poor medication storage practices, use of medications from different prescribers, reuse of discontinued medicines, and keeping expired or no longer required drugs are common irrational drug use at home reported in developing countries. These are attributed to patients’ lack of information on proper storage conditions, proper disposal of unused medicines, and risks associated with inappropriate/irrational drug use.3,4
Globally, studies in different countries revealed a high prevalence of irrational household medication storage, ranging from 35.1% to about 100%.5 The commonly household stored classes of drugs were systemic anti-infective drugs, nervous system drugs, gastrointestinal drugs followed by drugs of the cardiovascular and respiratory systems. This increases the risk of treatment failure, antimicrobial resistance, accidental intoxication, inappropriate self-medication, and unsafe disposal of medications which can endanger public health by causing environmental pollution and accidental poisoning of animals and humans.5–9
Most COVID-19 patients have mild illnesses and can rehabilitate at home with over-the-counter drugs, such as paracetamol and ibuprofen.10 Besides, despite warnings from CDC and NIH, COVID-19-positive outpatients use antiviral and supporting agents such as antibiotics and corticosteroids to manage symptoms of the disease.11,12 Thus, being infected or fear of acquiring COVID-19 could increase the storage of drugs at home.
Having evidence on the extent, source, use, and storage conditions of medicines at household level and associated factors are vital to take actions toward assuring rational use of drugs. In Ethiopia, few studies, specifically in northern Ethiopia, were conducted at the household level to assess medications’ storage practice. Therefore, this study aimed to explore the prevalence of household medicine storage practices and associated factors among households in Mizan-Aman town, Southwestern Ethiopia.
Methods and Materials
Study Area and Design
A community-based cross-sectional study was done in some selected households of Mizan-Aman Town from February 1 to May 30, 2022, Southwestern Ethiopia. The town is located about 561 km away from the capital Addis Ababa. The administrative division of the town includes a total of 10 Woredas (districts) and 246 kebeles (smallest administrative units) (229 rural and 17 urban) (18). The present study was undertaken in the urban areas of the town (Mizan-Aman administrative).
Sample Size Determination and Sampling Procedure
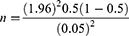
The number of households included in the study was determined using a single population proportion formula. To get the maximum possible sample size, the proportion (p) of households with at least one medicine during data collection was taken to be 50%. The margin of error (δ) was taken to be 5%, and the z1 − ∝ at 95% confidence interval (CI) was set at 1.96. Based on this, the sample size was calculated using the formula:
n = 384, adding 5% for non-response rate (0.05 * 384 = 19) the final sample size was 403.
The households were selected by using a simple random sampling method after proportional allocation of the sample size to each district.
Data Collection Tool and Procedure
To assess the research theme, a questionnaire that included socio-demographic factors, history of illness in the month preceding the study, home storage of medications, their disposal methods, and other important variables was prepared (Supplementary Material). Data were collected in a face-to-face interview using a structured questionnaire and by observation. Whenever selected houses were found closed or missing adult members, they were revisited continuously for three subsequent days in order to collect data. For households that were missing adult members, the nearest houses were selected, while houses which were found closed during the three subsequent days were considered as non-response cases. When multiple adults were present in the same household, lottery method was applied to select a single adult.
Data Processing and Analysis
The data were entered into Epi Info Version 3.5.1 and checked for completeness, and then it was transported to Statistical Software Package for Social Science (SPSS) version 22. Descriptive analysis was done, and findings were presented with percentages, tables, and graphs. GraphPad prism version 9.4.0 was used to draw graphs. To determine the variables influencing the storage of medications in homes, bivariate followed by multivariate logistic regression were used. After bivariate analysis, predictor variables with a p-value of less than 0.2 were considered in multivariate logistic regression analysis. Predictor variables in multivariate logistic regression were regarded to have a significant connection with the outcome variable if their p-value was less than 0.05. Finally, adjusted odds ratio (AOR) with its 95% CI was reported.
Definition of Terms
Medications: Any prescribed or over-the-counter drugs stored in households for any purpose.
Appropriate storage conditions: Storage of medications in a dry, clean, and well-ventilated area at an appropriate temperature and away from reach of children.
Adequately labeled: If the label on the medication contains at least the drug’s name, strength or unit dose, frequency, and duration of administration, then the drug was deemed adequately labeled.
Results
A total of 367 households were included in the present study, with a response rate of 91%. The majority of the respondents were male, 228 (62%), and in the age group between 18 and 29, 155 (42%). Most of the respondents, 212 (69%), cannot read and write. More than half of the respondents (60.8%) have above five family members. On the other hand, about half of the respondents (50.4%) had a monthly income that ranged from 1500 to 5000 ETB (equivalent to 28–93 US dollar) (Table 1).
 |
Table 1 Sociodemographic Characteristics of the Respondents and Households in Southwest Ethiopia, 2022, (n=367) |
Medical and Health Status of Household Members
Of the respondents, 56 (15%) had at least one chronic patient in their family. Of those who were sick in the last 3 months, the majority (70.8%) of them had an acute illness. Hypertension (32%) followed by diabetes mellitus (25%) and bronchial asthma (25%) were the most common chronic diseases for which medicines were kept in the households (Table 2).
 |
Table 2 Medical and Health Status of Household Members in Southwest Ethiopia, 2022, (n=367) |
Prevalence, Disposal, and Situation of Home Stored Medicines
From a total of 367 households visited, 176 (48%) had stored drugs. As depicted in Figure 1, from a total of 251 medication types observed in households during data collection, analgesics (28.7%), antibacterial (21.1%), antimalarial (17.53%), and anthelmintics (12.75%) were the predominant class of drugs stored in the households. The largest proportion of the home-stored medications (34.7%) was reserved for future use, and 31.8% were stored for treating current medical conditions. Most of the households (36.9%) kept the medications on a shelf, followed by inside a box (26.7%) and in a bedroom (18.75%). Solid dosage forms were the most common medication formulations, of which tablets and capsules account 73% and 11.1%, respectively. About half of the households (50.6%) obtained the medications from public hospitals, followed by private pharmacies (42.6%) and family/friends (6.8%). Regarding the number of drugs stored in households, about 40% of the households stored two types of medications. Though most of the medications (84.8%) were not expired, 62.5% of them lacked clear instructions on how to use them. Besides, 9.2% of the households stored drugs with their primary package damaged, and 75.6% stored the medications inappropriately (Table 3).
 |
Table 3 Information on Medications Stored in the Households, Southwest Ethiopia, 2022, (n=176) |
 |
Figure 1 Types of medication stored in the households of southwest Ethiopia, 2022. |
As portrayed in Figure 2, planned methods for disposal of home-stored medication were throwing it into the garbage/dust bin (38.6%), flushing it down the toilet (30.7%), and burning it (6.8%). A significant proportion of the respondents (21%) had no idea how to discard leftover or expired medications. The majority of the respondents (84.1%) had never heard/learned about the safe disposal ways of drugs. Only a few of them (15.9%) had information from neighbors/friends, e-media, literature, and healthcare providers (Figure 3).
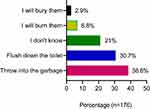 |
Figure 2 Planned methods of disposing unused or expired medications. |
 |
Figure 3 Sources of information on how to dispose of medications. |
Factors Associated with Medication Storage at Household Level in Southwest Ethiopia
In bivariate analysis, variables such as education, number of family member, HH monthly income, presence of children less than 5 years in HH, presence of elders greater than 65 years in HH, and presence of health professionals in HH were associated with medication storage in HH at p-value less than 0.2. In multiple variable regression, the presence of children less than five years in HH and the existence of chronic patients in HH were significantly associated with medication storage in HH at P-value less than 0.05 (Table 4).
 |
Table 4 Factors Associated with Medication Hoarding at Household Level in Southwest Ethiopia, 2022 |
In this study, the odds of household medication storage was 1.90 times higher among households with children less than five when compared with those households that do not have children less than five [AOR = 1.90 (1.19, 3.05)]. In addition, the odds of household medication storage was 4.3 times higher among households in which chronically sick patients exist [AOR = 4.3 (2.25, 8.45)].
Discussion
Despite variations in the reasons behind it, household medication storage is a common practice worldwide with both prescription and over-the-counter medications.13 The findings of the present study revealed that the prevalence of household medication storage during the COVID-19 outbreak was 48%, which is higher than the studies done in similar areas before the COVID-19 era. For instance, studies from Tigray,14 northern Ethiopia; Gondar,15 northwest Ethiopia; and Northern Uganda16 showed a prevalence of 29%, 44.2%, and 35.1%, respectively. Thus, the COVID-19 outbreak could be one potential factor for the relatively high prevalence of household medication storage in the present study area.
The finding of the current study disclosed that largest proportion of the home-stored medications (34.7%) were reserved for future use, 31.8% of them stored for treating current medical conditions, and the rest 33.5% were left over from past treatments. Similar studies from Iraq,17 Tigray (Ethiopia),14 and Northern Uganda16 showed a large percentage of stored drugs were for ongoing use, whereas leftover and standby drugs make up relatively small percentages. The large percentage of medications set aside for future use could be attributed to the stockpiling of medications in case of acquiring COVID-19.
In the present study, analgesics (28.7%) followed by antibacterial (21.1%) were the most common drugs hoarded in households which is in line with the studies done in Northwest Ethiopia,18 Northern Uganda,16 and Riyadh (Saudi Arabia).19 This is because most COVID-19 patients develop mild illnesses and can rehabilitate at home with over-the-counter analgesics. Besides, large proportions of COVID-19 patients are reported using antibiotics for managing their symptoms.11 The higher percentage of stored antibiotics at home might also be an indicator of poor adherence, which could lead to antibiotic resistance and treatment failure.
Most of the households in our study (36.9%) kept the medications on shelf followed by inside a box (26.7%) and in bedroom (18.75%). Besides, 9.2% of the households stored drugs with their primary package damaged, and 75.6% of them stored the medications inappropriately. Observation of the storage conditions of the inappropriately stored medicines revealed that 61.9%, 25.9%, and 12.2% were stored within reach of children, contaminated with dust, and directly exposed to sunlight, respectively. Reports from West Bengal,7 Brazil,20 and Qatar21 disclosed that 16.7%, 26.5%, and 90% of home-stored medications were easy to reach/within reach of children. Inappropriate storage of medicines and damage of the primary packaging have the potential to cause physical, chemical, and microbiological changes, which cause loss of effectiveness and safety of the medications. Moreover, storing drugs within reach of children increases the risk of accidental poisoning and suicide attempts.13 To promote safe utilization of stored medications, especially in households with chronic patients, it should be recommended to use a home medication cabinet with a lock and key.
Solid dosage forms were the most common medication formulations stored in this study, of which tablets and capsules account for 73% and 11.1%, respectively, followed by liquid (8.7%) and semisolid formulations (3.2%). Almost all of the studies done in the area reflect our findings. This is because solid and liquid dosage forms are standard discharge formulations; besides, many individuals use over-the-counter medications in these dosage forms.
This study showed that about half of the households (50.6%) obtained the medications from public hospitals, followed by private pharmacies (42.6%) and family/friends (6.8%). A study done in Awi Zone (Ethiopia) reported that most (95.9%) home hoarded medications were obtained from public health facilities and about 2.5% from a friend.18 Similarly, a report from Iraq revealed that private pharmacies were the primary source of home-stored medications, followed by public health centers.17 In all cases, almost all of the households had contact with at least one healthcare provider (pharmacist); thus, pharmacists’ provision of a full package of information about the drug they dispense with appropriate labeling would promote safe utilization and disposal of medications.
Though in our study, most of the medications (84.8%) were not expired, 62.5% of them lacked clear instructions on how to use them. The percentage of expired drugs in our study is relatively lower than the reports from South India (17%) and higher than Gondar (3.14%). Families could possibly keep expired medications due to a lack of information about such substances and their appropriate disposal methods.
The current investigation documented unneeded or expired medications being disposed of in dustbins (38.6%) and toilets (30.7%). These were uninformed decisions because most respondents (84.1%) uncovered that they had never heard about the proper disposal methods of drugs. This finding is in line with the studies done in Tanzania,22 Northern Ethiopia,18 and Saudi Arabia.23 These environmentally harmful disposal techniques could cause detrimental effects in human and animal health; thus, awareness creation or campaign on the safest disposal methods of home stored medications such as returning expired or unneeded drugs to pharmacies and initiating take-back programs should be carried out. Though the Food, Medicine and Healthcare Administration and Control Authority (FMHACA) of Ethiopian, now called the Ethiopian Food and Drug Authority (EFDA), has developed a guideline on medicines waste management and disposal, there needs to be more awareness creation and enforcement of its implementation.24
The presence of under-five children and chronically sick individuals in households were the two factors that significantly affected home storage of medications in the current study. This finding strengthens the assumption that being infected or fear of getting COVID-19 to be the potential reason for the high prevalence of household medication storage in the present study. This is supported by different studies which revealed that children who are black and under the age of 5, and individuals with comorbid conditions are at high risk of severe COVID-19.25–27 Therefore, being more vulnerable to coronavirus may prompt the stockpiling of medications for home management of the disease.
Limitation of the Study
The study’s cross-sectional design makes it difficult to establish a causal connection between the predictor and outcome variables. Besides, the absence of studies on the prevalence of household medication storage in the current study area before the COVID-19 outbreak makes it difficult to compare our findings and clearly show the effect of coronavirus pandemic on the prevalence of home stored medications.
Conclusion
As per our finding, the prevalence of home-stored drugs was high (48%) in southwest Ethiopia, where around two-thirds of the stored drugs were not for ongoing treatment. Some drugs were also expired, and their primary package was damaged. Besides, most of the respondents were not aware of the proper methods of medication storage and disposal. The presence of under-five children and chronically sick individuals in households were the two factors that significantly affected home storage of medications. Based on the findings of the present result, it is possible to say that COVID-19 outbreak could be one primary factor for the relatively high prevalence of household medication storage in the current study area. Thus, to lessen or eliminate the negative consequences of storing medications at home, it is necessary to review the medication utilization chain and offer community-based training on proper medication storage and disposal techniques, including establishing take-back programs in developing nations like Ethiopia. The Ethiopian Food and Drug Authority (EFDA) should take these initiatives for their enactment.
Data Sharing Statement
All data are within the manuscript.
Ethical Approval and Consent to Participate
This study was approved by the Research Ethics Review Committee (RERC) of Mizan-Tepi University (SP-01627/22). Before the start of the study, a written consent to participate was obtained from all respondents after clarifying the objectives, purpose, and the harm and benefits of the study. Also, confidentiality, anonymity, and freedom to withdraw from the study at any time were maintained throughout the study. Our study complies with the declaration of Helsinki.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. World Health Organization. Promoting rational use of medicines: core components patient care indicators; 2022. Available from: https://scholar.google.com/scholar?hl=en≈sdt=0%2C5&q=World+Health+Organization%3A+Promoting+rational+use+of+medicines%3A+core+components+patient+care+indicators&btnG=.
2. Kebede M, Dereje Kebebe Borga EMB, Mulisa Bobasa E. Drug utilization in selected health facilities of South West Shoa Zone, Oromia region, Ethiopia. Drug Healthc Patient Saf. 2015;7:121–127. doi:10.2147/DHPS.S84890
3. Melku L, Wubetu M, Dessie B. Irrational drug use and its associated factors at Debre Markos Referral Hospital’s outpatient pharmacy in East Gojjam, Northwest Ethiopia. SAGE Open Med. 2021;9:1. doi:10.1177/20503121211025146
4. Ofori-Asenso R, Agyeman AA. Irrational use of medicines—A summary of key concepts. Pharmacy. 2016;4(4):35. doi:10.3390/pharmacy4040035
5. Jafarzadeh A, Mahboub-Ahari A, Najafi M, Yousefi M, Dalal K. Medicine storage, wastage, and associated determinants among urban households: a systematic review and meta-analysis of household surveys. BMC Public Health. 2021;21(1):1–15. doi:10.1186/s12889-021-11100-4
6. Alenazi AB, Alsharidah MS, Al-Najjar AH, Alghazy SA, Alqadi AAA, Marzouk A. Medication storage at home among people in Al-Qassim Region, Saudi Arabia. Int J Pharmacol Clin Sci. 2019;8(1):52–59. doi:10.5530/ijpcs.2019.8.10
7. Maharana S, Paul B, Dasgupta A, Garg S. Storage, reuse, and disposal of unused medications: a cross-sectional study among rural households of Singur, West Bengal. Int J Med Sci Public Heal. 2017;2017:1.
8. Kassie AD, Bifftu BB, Mekonnen HS. Self-medication practice and associated factors among adult household members in Meket district, Northeast Ethiopia, 2017. BMC Pharmacol Toxicol. 2018;19(15):4–11. doi:10.1186/s40360-018-0205-6
9. Deviprasad PS, Laxman CV. Cross sectional study of factors associated with home storage of medicines. J Chem Pharm Res. 2016;8(8):1114–1120.
10. Treatments for COVID-19 - Harvard health; 2022. Available from: https://www.health.harvard.edu/diseases-and-conditions/treatments-for-covid-19.
11. CDC. Corticosteroids, antibiotics generally not recommended for COVID-19 outpatients | AHA news; 2022. Available from: https://www.aha.org/news/headline/2022-04-26-cdc-corticosteroids-antibiotics-generally-not-recommended-covid-19.
12. COVID-19 Treatment Guidelines Panel. Coronavirus disease 2019 (COVID-19) treatment guidelines. National Institutes of Health; 2022. Available from: https://www.covid19treatmentguidelines.nih.gov/.
13. Martins RR, Farias DA, Oliveira MY, Diniz RDS, Oliveira AG. Prevalence and risk factors of inadequate medicine home storage: a community-based study. Rev Saude Publica. 2017;51(95):1–8. doi:10.11606/S1518-8787.2017051000053
14. Wondimu A, Molla F, Demeke B, Eticha T, Assen A. Household storage of medicines and associated factors in Tigray Region, Northern Ethiopia. PLoS One. 2015;2015:1.
15. Teni FS, Surur AS, Belay A, et al. A household survey of medicine storage practices in Gondar town, northwestern Ethiopia. BMC Public Health. 2017;17:1–9. doi:10.1186/s12889-017-4152-8
16. Ocan M, Bbosa GS, Waako P, Ogwal-okeng J, Obua C. Factors predicting home storage of medicines in Northern Uganda. BMC Public Health. 2014;14:1–7. doi:10.1186/1471-2458-14-650
17. Abood SJ, Abdulsahib WK, Al-Radeef MY. Prevalence of home storage of medicines and associated factors in Iraq. Open Access Maced J Med Sci. 2021;9:356–363. doi:10.3889/oamjms.2021.5997
18. Yimenu DK, Teni FS, Ebrahim AJ. Prevalence and predictors of storage of unused medicines among households in Northwestern Ethiopia. J Environ Public Health. 2020;2020:1–10. doi:10.1155/2020/8703208
19. Wajid S, Siddiqui NA, Mothana RA, Samreen S. Prevalence and practice of unused and expired medicine - A community-based study among Saudi adults in Riyadh, Saudi Arabia. Biomed Res Int. 2020;2020:1–5. doi:10.1155/2020/6539251
20. Santos DF, Pinto M, Silveira T, et al. Unsafe storage of household medicines: results from a cross-sectional study of four- year-olds from the 2004 Pelotas birth cohort (Brazil). BMC Pediatr. 2019;19(235):1–9. doi:10.1186/s12887-019-1597-1
21. Hendaus MA, Saleh M, Darwish S, et al. Parental perception of medications safe storage in the State of Qatar. J Fam Med Prim Care. 2021;10:2969–2973. doi:10.4103/jfmpc.jfmpc_1259_20
22. Marwa KJ, Mcharo G, Mwita S, Katabalo D, Ruganuza D, Kapesa A. Disposal practices of expired and unused medications among households in Mwanza, Tanzania. PLoS One. 2021;16:1–9. doi:10.1371/journal.pone.0246418
23. Lucca JM, Dhfer Alshayban DA. Storage and disposal practice of unused medication among the Saudi families: an endorsement for best practice. Imam J Appl Sci. 2019;4:1–6.
24. World Health Organization. Food, medicine and healthcare administration and control authority of Ethiopia. Med Waste Manag Disposal Dir. 2011;2011:1–40.
25. Bandi S, Nevid MZ, Mahdavinia M. African American children are at higher risk of COVID‐19 infection. Pediatr Allergy Immunol. 2020;31(7):861. doi:10.1111/pai.13298
26. Special considerations in children | COVID-19 treatment guidelines; 2022. Available from: https://www.covid19treatmentguidelines.nih.gov/management/clinical-management-of-children/special-considerations-in-children/.
27. CDC. People with certain medical conditions; 2022. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.