Back to Journals » Cancer Management and Research » Volume 13
Predictive Value of Preoperative Controlling Nutritional Status Score Combined with Fibrinogen–Albumin Ratio in Postoperative Local Recurrence-Free Survival of Patients with Retroperitoneal Liposarcoma
Authors Xue GQ, Li CP, Lv A, Tian XY, Wu JH, Qiu H , Hao CY
Received 22 February 2021
Accepted for publication 13 July 2021
Published 6 August 2021 Volume 2021:13 Pages 6157—6167
DOI https://doi.org/10.2147/CMAR.S307920
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Guo-Qiang Xue, Cheng-Peng Li, Ang Lv, Xiu-Yun Tian, Jian-Hui Wu, Hui Qiu, Chun-Yi Hao
Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Department of Hepato-Pancreato-Biliary Surgery, Peking University Cancer Hospital & Institute, Beijing, People’s Republic of China
Correspondence: Chun-Yi Hao
Key laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Department of Hepato-Pancreato-Biliary Surgery, Peking University Cancer Hospital & Institute, No. 52 Fucheng Road, Haidian District, Beijing, People’s Republic of China
Tel +86-10-88196182
Fax +86-10-88196548
Email [email protected]
Background: Previous studies have shown that nutrition and systemic inflammation plays an essential role in the development of soft tissue sarcoma. However, few studies have explored the association of clinicopathologic features and local recurrence with nutritional and inflammatory markers in retroperitoneal liposarcoma (RPLS). This study sought to evaluate the prognostic value of the preoperative nutritional and inflammatory markers for local recurrence-free survival (LRFS) among surgical RPLS patients.
Methods: The study included 111 RPLS patients who underwent surgery between May 2010 and June 2019 at the Peking University Cancer Hospital Sarcoma Center. Time-dependent receiver operating characteristic (time-ROC) curve analysis was conducted to evaluate the ability of markers to predict LRFS. The associations of the CONUT-FAR score with clinicopathological variables and LRFS were evaluated.
Results: In the time-ROC curve analysis, the CONUT-FAR score was superior to other nutritional and inflammatory markers in predicting LRFS. The CONUT-FAR score was the only nutritional and inflammatory marker that independently predicted LRFS in the multivariate analysis, and patients with a high CONUT-FAR score (> 11) showed significantly decreased LRFS. Although the CONUT-FAR score failed to discriminate patients with low grade (G1) (p = 0.327) or undergoing incomplete (R2) resection (p = 0.072), it stratified patients with high grade (G2 and G3) or undergoing complete resection (R0/R1) into subgroups with significantly distinct LRFS (p < 0.001). The CONUT-FAR score also showed good clinical utility among patients with different clinical characteristics.
Conclusion: The preoperative CONUT-FAR score reflects both nutritional and inflammatory factors and is an effective predictor of LRFS for surgical RPLS patients.
Keywords: nutritional status, fibrinogen–albumin ratio, retroperitoneal liposarcoma, prognostic factor, time-dependent ROC
Introduction
Retroperitoneal sarcoma (RPS) is a rare and heterogeneous disease that accounts for approximately 15% of soft tissue sarcomas diagnoses.1 Liposarcoma is the most common histological type of RPS, accounting for approximately 40–60% of RPS.2 Since retroperitoneal liposarcoma (RPLS) is relatively insensitive to chemotherapy or radiotherapy, extensive resection is the primary curative treatment.3 Considering that retroperitoneal anatomy limits the ability to achieve wide resection margins, local recurrence after surgery remains the main cause of treatment failure and the primary cause of disease-specific death, with rates ranging from 30% to 50%.4 Hence, a reliable prognostic indicator is needed to identify patients at high risk of recurrence and optimize their follow-up strategy and adjuvant therapies.
RPLS tends to present as a large, painless mass that compresses the gastrointestinal tract, which can lead to elevated systemic inflammation and malnutrition.5,6 Therefore, the nutritional and inflammatory status play critical roles in tumor progression and prognosis.5,7 Peripheral blood parameters such as neutrophil count, lymphocyte count, platelet count, serum albumin (ALB) levels, fibrinogen levels, and total cholesterol (TC) are prognostic determinants and have clinical utility according to several studies.8–12 Several methods for the assessment of inflammatory and/or nutritional status, which are mainly derived from routine blood examinations, have been explored, including the neutrophil-lymphocyte ratio (NLR), platelet-lymphocyte ratio (PLR), fibrinogen–albumin ratio (FAR), and controlling nutritional status (CONUT) score.12–15 The CONUT score, which is calculated from ALB, total lymphocyte count (TLC), and TC, was developed to assess nutritional status.13 Multiple studies have revealed that malnutrition and elevated inflammatory status significantly increase postoperative complications and have a negative impact on the survival of patients with soft tissue sarcoma.14,16,17 However, to our knowledge, few studies have explored the association of clinicopathologic features and local recurrence with the nutritional and inflammatory markers in RPLS.
This study therefore aimed to evaluate the prognostic relevance of the preoperative nutritional and inflammatory markers in predicting local recurrence for surgical RPLS patients.
Patients and Methods
The study was supported by the Ethics Committee of the Peking University Cancer Hospital, and informed consent was obtained from all patients prior to participation in this study.
Patients
From May 2010 to June 2019, data of 125 consecutive patients who underwent surgical resection for RPLS at the Peking University Cancer Hospital Sarcoma Center were carefully reviewed. The eligibility criteria were as follows: (1) pathologically confirmed RPLS; (2) absence of metastasis; (3) available medical records and follow-up data; and (4) no preoperative chemotherapy, radiotherapy or targeted therapy. Patients who were lost to follow-up (n=1), received preoperative targeted therapy (n=5), were diagnosed with acute infection or chronic inflammatory diseases (n=3) or had incomplete laboratory data (n=5) were excluded. Finally, 111 patients were included for analysis.
Diagnosis and Treatment
A diagnosis of RPLS was confirmed based on the histopathologic evidence. The histological subtypes were classified according to the 2013 World Health Organization classification.18 Considering the rarity of the retroperitoneal pathological subtypes, the myxoid/round cell subtype was considered a continuum. The RPLS was therefore classified into four histologic subtypes: 1) well-differentiated (WDLPS), 2) myxoid/round cell (MLPS), 3) dedifferentiated (DDLPS), and 4) pleomorphic (PLPS). The histological grade was determined based on the French Federation of Cancer Centers Sarcoma Group (FNCLCC).19 The variables retrieved from the medical records included sex, age, presentation status, size, multifocality, histological subtypes, FNCLCC grade, and extent of resection.
The decision to conduct surgical resection was made by a multidisciplinary team. R0/R1 and R2 resection were defined as complete resection and incomplete resection, respectively.3 For presentation status, the study identified sarcomas as primary when diagnosed without previous surgical resection, and as recurrent when the sarcomas presented at least three months after curative resection. Multifocality was defined as more than one noncontiguous tumor through pathological confirmation.
Definition of Preoperative Nutritional and Inflammatory Indicators
Blood test results, including serum fibrinogen, ALB, white blood cell count, platelet count and TC, were collected within two weeks before surgery. Nutritional and inflammatory biomarkers were calculated as follows: NLR = neutrophil count/lymphocyte count; PLR = platelet count/ lymphocyte count; FAR = fibrinogen/ALB×100; CONUT score = ALB score + total lymphocyte score + TC score. The CONUT score was determined based on previously described methods (details shown in Table S1).13
Patients were dichotomized into low and high FAR groups according to the cut-off value. Based on the median of CONUT score, the low FAR group and high FAR group scores were 4 and 8, respectively. The COUNT-FAR score was defined as the CONUT score + the FAR score.
Follow-Up
Patients were regularly evaluated every three months during the first two years after discharge and every six months thereafter. At each follow-up, routine hematology (complete blood count), serum biochemistry (liver and renal function test), and abdominopelvic contrast-enhanced CT or MRI were performed. The primary end-point of the study was local recurrence-free survival (LRFS, defined as the time from surgery to the first local recurrence). Local recurrence was defined as the presence of new lesions revealed by imaging. Survival outcomes were collected from the outpatient clinic visits and telephone interviews.
Statistical Analysis
Continuous variables were presented as median (interquartile range [IQR]) and were evaluated using the Mann–Whitney U-test, whereas categorical data were summarized as numbers (proportions) and were analyzed by the two-sided Chi-square test or Fisher’s exact test. Time-dependent receiver operating characteristic (ROC) curve analysis was performed via the inverse probability of censoring weighting approach and the area under the ROC curve (AUC) was estimated to compare the ability of nutritional and inflammatory biomarkers in predicting LRFS.20 The optimal cut-off value of nutritional and inflammatory biomarkers is determined by the largest point of the log-rank statistic for 5-year LRFS by applying X-tile analysis.21 LRFS rates were calculated using the Kaplan–Meier method and were compared between groups by the Log rank test. Multivariate Cox regression analysis was conducted to determine the independent predictors of LRFS. Hazard ratios (HRs) estimated from the Cox analysis were reported as relative risks with corresponding 95% confidence intervals (95% CIs). Time-dependent ROC curve analysis was performed with the “time-ROC” package in R version 3.6.1 (http://www.r-project.org/); X-tile analysis was conducted using X-tile software (version v3.6.1, Yale University); and other statistical analyses were carried out using SPSS software (version 24.0, Chicago, IL, USA). A p-value < 0.05 was considered statistically significant.
Results
Patient Characteristics
The detailed baseline characteristics of the 111 patients are summarized in Table 1. The majority of patients were male (56.8%) and the median age was 57 years (IQR 48–63). Fifty-nine patients (53.2%) presented with recurrence, and the remaining 52 patients (46.8%) had primary tumors. G1, G2 and G3 tumors were found in 22 (19.8%), 49 (44.1%) and 40 (36.0%) patients, respectively. The median tumor size was 20 cm (IQR 14–28). The pathological subtypes were identified as follows: WDLPS (n=24, 21.6%), DDLPS (n=61, 55.0%), MLPS/RLPS (n=17,15.3%) and PLPS (n=9, 8.1%). The proportion of multifocality was 85.6%, and 14.4% of patients underwent incomplete resection. The median levels of the FAR, NLR, PLR, and CONUT scores were 10.8 (IQR 7.8–17.9), 2.5 (IQR 1.6–3.6), 167.6 (IQR 133.9–254.9), and 4 (IQR 3–5), respectively.
 |
Table 1 Baseline Characteristics of Total 111 Patients with Retroperitoneal Liposarcoma, as Well as Patients in the High (> 11) and Low (≤11) CONUT-FAR Score Groups |
Comparison of the Ability of Nutritional and Inflammatory Indicators in Predicting Local-Recurrence-Free Survival (LRFS)
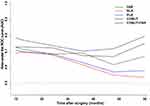
The AUC of the CONUT-FAR score for predicting LRFS was significantly higher than those of the NLR, PLR, FAR and CONUT score at all tested timepoints (Figure 1). Therefore, the CONUT-FAR score was superior for predicting LRFS in surgical RPLS patients than any other markers assessed. The AUCs of the CONUT-FAR in predicting the 1-, 3-, and 5-year LRFS were 0.776, 0.704, and 0.796, respectively. The data for the NLR, PLR, FAR and CONUT scores were shown in Table S2.
The Optimal Cut-off Values of Nutritional and Inflammatory Indicators
X-tile analysis for 5-year LRFS was used to determine the optimal cut-off value of nutritional and Inflammatory markers. The high and low groups were created based on the markers’ respective optimal cut-off values. The optimal cut-off values of NLR, PLR, FAR, CONUT score, and CONUT-FAR score were 3.6, 153.3, 16.9, 5 and 11, respectively (Figure S1). Therefore, for the CONUT-FAR score, patients were divided into low (≤11, n = 85) and high (>11, n = 26) CONUT-FAR groups.
Correlation Between the CONUT-FAR Score and Clinicopathologic Characteristics
As presented in Table 1, the following variables were significantly different between the low and high CONUT-FAR groups: presentation status (p = 0.032), multifocality (p = 0.012), and extent of resection (p < 0.001). However, the groups were similar in terms of sex, age, tumor size, proportion of histological subtypes and FNCLCC grade (p > 0.05 for all). In addition, the high CONUT-FAR group also had a significantly elevated FAR (p < 0.001), elevated NLR (p < 0.001), elevated PLR (p < 0.000) and elevated CONUT score (p < 0.001).
Univariable and Multivariable Analyses for LRFS
In univariate analyses, the presentation, histologic subtypes, FNCLCC grade and extent of resection were significantly associated with LRFS, as were the FAR, NLR, PLR, CONUT score and CONUT-FAR score. Multivariate analysis showed that the CONUT-FAR score was an independent prognostic factor of LRFS in surgical RPLS patients (>11 vs ≤11: HR 2.552, 95% CI 1.476–4.415; p = 0.001), as were the FNCLCC grade (G3 vs G1:HR 4.798,95% CI 1.821–12.641; p = 0.005) and the extent of resection (incomplete vs complete: HR 3.849, 95% CI 2.001–7.406; p < 0.001) (Table 2).
 |
Table 2 Univariate and Multivariate Analyses to Determine Independent Predictors of LRFS of RPLS |
LRFS in the High and Low CONUT-FAR Groups
With a median follow-up of 32 months (IQR 24–51), 24 patients (92.3%) in the high CONUT-FAR group developed recurrence compared with 45 (52.9%) in the low CONUT-FAR group. The median LRFS in the high CONUT-FAR group (7 months) was significantly lower than in the low CONUT-FAR group (29 months, p < 0.001) (Figure 2).
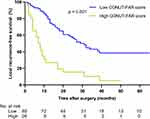 |
Figure 2 Comparison of local recurrence-free survival (p<0.001) between patients with high (> 11) and low (≤11) CONUT-FAR score in the entire patient cohort. |
Subgroup Analyses of LRFS in Patients with High and Low CONUT-FAR According to the Extent of Resection and Histologic Grade
Considering that FNCLCC grade and extent of resection were the two most critical factors in the prognosis of RPLS, we further examined the prognostic role of the CONUT-FAR score in RPLS patients stratified by FNCLCC grade and extent of resection.
Using the optimal cut-off value, the CONUT-FAR score stratified patients who received complete resection into two subgroups with significantly distinct LRFS (p <0.001) (Figure 3A). However, for patients who underwent incomplete R2 resection, there was no significant prognostic difference between the high CONUT-FAR score group and the low CONUT-FAR score group (p = 0.072) (Figure 3B).
Similarly, when we divided patients based on histological grade, the CONUT-FAR score stratified patients with high-grade tumors (G2 and G3) into two subgroups with significantly distinct LRFS (G2: p <0.001; G3: p<0.001) (Figure 4B and C). However, for patients with G1 tumors, the high CONUT-FAR subgroup had no significant prognostic differences than those in the low CONUT-FAR subgroup (p = 0.327) (Figure 4A).
Subgroup Analyses to Assess the Clinical Utility of the CONUT-FAR in Predicting LRFS
To further assess the clinical utility of the CONUT-FAR score in predicting LRFS, subgroup analyses using univariate Cox regression were conducted on the basis of sex (female or male), age (≤ 60 or >60 years), presentation status (primary or recurrence), multifocality (no or yes), FNCLCC grade (G1, G2 or G3), and extent of resection (complete or incomplete). We found that a high CONUT-FAR score (>11) was associated with poor LRFS in nearly all subgroup analyses (Figure 5). Although it failed to obtain statistical significance in subgroup analyses of LRFS in patients with G1 sarcoma and who underwent incomplete resection, the trend of poor prognosis in patients with a high CONUT-FAR score was consistent.
Discussion
Current prognostic tools focus on tumor pathologic and histologic characteristics available only after surgery, such as the Personalised Sarcoma Care (PERSARC) model and prognostic nomograms. The recommended prognostic Sarculator used for RPS is a postoperative prognostic nomogram, which incorporated tumor size, FNCLCC grade, histologic subtype and multifocality to determine 7-year disease-free survival.22 And the PERSARC model, which included age, size, depth, histology and radiotherapy (RT), only focused on the patients with high-grade extremity soft-tissue sarcomas after surgical resection,23 and has limited value for RPS because of the anatomic constraints of the retroperitoneum as well as the different histologic subtype distribution. Although these postoperative prognostic models are validated, a growing body of evidence suggests that preoperative patient-specific factors, such as nutritional and systemic inflammation, can improve prognostication for STS in the preoperative setting.12,15,17,24 However, the prognostic value of these markers in patients with RPLS is still unknown.
This study investigated the prognostic significance of preoperative nutritional and inflammatory markers in surgical RPLS patients. We found that the combined use of the CONUT score and the FAR is superior to the CONUT score, FAR, NLR, and PLR for predicting LRFS among RPLS patients. Moreover, the preoperative CONUT-FAR score was an independent predictor of LRFS. With the robust prognostic value in subgroup analyses of patients with different clinical characteristics, the CONUT-FAR score is a more valuable prognostic marker for RPLS patients than other commonly used nutritional and inflammatory indicators.
Studies examining the association between the NLR or PLR and prognosis in STS have found widely divergent results.12,14,16,25,26 In the present study, we confirmed that the NLR and PLR were not independently associated with LRFS among RPLS patients. In line with our observations, Nakamura et al examined the role of the pretreatment NLR and PLR in a cohort of 310 STS patients and observed that neither the NLR nor the PLR were independent prognostic factors for OS and DFS.14 However, these results were not confirmed in other studies. In a cohort of 260 STS patients with limb soft tissue sarcomas, a high NLR (≥ 3.58) was significantly associated with decreased time to tumor recurrence and poor OS.25 Similarly, in a cohort of 222 STS patients, a significantly worse disease-specific survival was observed in patients with a high PLR.16 However, RPLS patients accounted for only a small proportion of these cohorts.
The CONUT score is a nutritional evaluation score, based on three objective parameters (ALB, TLC, and TC).13 Hypoalbuminemia has proved to be strongly associated with cachexia and poor survival.8 TLC is found to be an effective detector to predict survival in sarcomas.9 Serum TC level is correlated with tumor progression and patient survival in various cancers.27 Therefore, the CONUT score is an effective readout of the nutritional condition. A study by Zhou et al indicated that the CONUT score was superior to the NLR and PLR for predicting survival and was associated with OS and DFS in patients with STS.17 A high-plasma fibrinogen level is secondary to increased systemic inflammatory responses.28 A previous study revealed that an elevated FAR was a strong unfavorable prognostic factor in STS patients.15 In our study, although elevated preoperative FAR and CONUT scores showed an association with decreased LRFS in univariate analysis, they were not significant in multivariate analysis. Our results probably differ from those of previous studies because those studies included various histologic and anatomic presentations of STS. This has intrinsic limitations, because the oncologic outcome of STS strongly correlates with both the site of tumor origin and the histologic subtype.29–31 Therefore, researches focused on site-specific and histology-specific prognosis should be endorsed.
The combination of the CONUT score and FAR (CONUT-FAR score) exhibited superior prognostic ability for patients with RPLS after surgery than any single factor alone, as confirmed by the discriminatory power of time-dependent ROC analyses. In addition, the CONUT-FAR score was shown to be an independent prognostic indicator on multivariate analysis. Hence, we conclude that compared with the traditional nutritional and inflammatory markers, the CONUT-FAR score, which takes into account both the inflammatory status and nutritional status, could more accurately predict the LRFS of surgical RPLS patients.
FNCLCC grade and extent of resection are two critical and well-known prognostic factors of LRFS for RPLS patients.32 In the present study, FNCLCC grade and extent of resection were also identified as independent predictors of LRFS. Moreover, in the subgroup analyses of the FNCLCC grade and extent of resection, an elevated CONUT-FAR score was associated with decreased LRFS among patients with high-grade tumors (G2 and G3) and those who received complete resection, and the CONUT-FAR score further stratified these patients into subgroups with significantly distinct LRFS. However, the CONUT-FAR score was not significantly associated with LRFS among patients with G1 tumors and those who received incomplete resection, probably due to the small number of patients with G1 tumors and the intrinsic tendency of recurrence after incomplete resection, respectively.
In this study, a high CONUT-FAR score (>11) was more likely to be found in patients who presented with recurrence (p = 0.017), had multifocality tumors (p = 0.006), or underwent incomplete resection (P < 0.001), suggesting that the CONUT-FAR score could reflect tumor progression in patients with RPLS. Additionally, the CONUT-FAR score showed good clinical utility in patients with different clinical characteristics. Further subgroup analysis revealed that a high CONUT-FAR score was associated with decreased LRFS in patients regardless of sex, age, presentation status, or multifocality. Because patients with a high CONUT-FAR score have a high risk of recurrence, more frequent follow-up and molecular analysis should be considered.
There are several limitations in this study. First, the optimal cut-off value of nutritional and inflammatory markers may fluctuate based on sample size, and could be affected by patient-specific variables, such as age, alcoholism, smoking status, mental issues, comorbidities, socioeconomic status, among others. Second, this study was a retrospective analysis and selection bias could not be avoided. Because none patients in our cohort received preoperative radiotherapy or chemotherapy, so our study lacks the power to give insight into how preoperative treatment might affect the association between nutritional and inflammatory markers and (LRFS) among surgical RPLS patients. Third, due to the low incidence of RPLS, the sample size is relatively limited. Further large-scale, multi-center studies should be performed to verify our findings.
Conclusion
In summary, the preoperative CONUT-FAR score is not only significantly associated with clinical characteristics but also a preferred predictor of LRFS for surgical RPLS patients, superior to the traditional nutritional and inflammatory markers. The CONUT-FAR score is efficient, economical, and has robust predictive ability, making it a valuable marker in monitoring local recurrence in RPLS patients after surgery. Our findings may help surgeons and oncologists to monitor disease progression accurately and to plan individualized postoperative treatment strategies.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics
All patients provided written informed consent for participation in the study. The study protocol was in accordance with the Declaration of Helsinki, and the research ethics committee of Peking University Cancer Hospital approved this study (approval no. 2016KT41).
Funding
This work was supported by the Capital Health Research and Development of Special Funds (approval No.: 2020-1-1021), Beijing Municipal Administration of Hospital’s Ascent Plan (approval No.: DFL20181104), and Beijing Municipal Administration of Hospitals’ Youth Programme (approval No. QML20181104), interdisciplinary medicine Seed Fund of Peking University and the Fundamental Research Funds for the Central Universities [approval No.: BMU2020MX015], Science Foundation of Peking University Cancer Hospital 2020-13 and 2020-14.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Group T-ARW. Management of primary retroperitoneal sarcoma (RPS) in the adult: a consensus approach from the trans-atlantic RPS working group. Ann Surg Oncol. 2015;22(1):256–263. doi:10.1245/s10434-014-3965-2.
2. Improta L, Tzanis D, Bouhadiba T, Abdelhafidh K, Bonvalot S. Overview of primary adult retroperitoneal tumours. Eur J Surg Oncol. 2020;46(9):1573–1579. doi:10.1016/j.ejso.2020.04.054
3. Bonvalot S, Raut CP, Pollock RE, et al. Technical considerations in surgery for retroperitoneal sarcomas: position paper from E-Surge, a master class in sarcoma surgery, and EORTC-STBSG. Ann Surg Oncol. 2012;19(9):2981–2991. doi:10.1245/s10434-012-2342-2
4. Fairweather M, Wang J, Jo VY, Baldini EH, Bertagnolli MM, Raut CP. Surgical management of primary retroperitoneal sarcomas: rationale for selective organ resection. Ann Surg Oncol. 2018;25(1):98–106. doi:10.1245/s10434-017-6136-4
5. Kirov KM, Xu HP, Crenn P, et al. Role of nutritional status in the early postoperative prognosis of patients operated for retroperitoneal liposarcoma (RLS): a single center experience. Eur J Surg Oncol. 2019;45(2):261–267. doi:10.1016/j.ejso.2018.07.001
6. Hou T, Guo T, Nie R, et al. The prognostic role of the preoperative systemic immune-inflammation index and high-sensitivity modified Glasgow prognostic score in patients after radical operation for soft tissue sarcoma. Eur J Surg Oncol. 2020;46(8):1496–1502. doi:10.1016/j.ejso.2020.05.026
7. Elinav E, Nowarski R, Thaiss CA, Hu B, Jin C, Flavell RA. Inflammation-induced cancer: crosstalk between tumours, immune cells and microorganisms. Nat Rev Cancer. 2013;13(11):759–771. doi:10.1038/nrc3611
8. McMillan DC, Watson WS, O’Gorman P, Preston T, Scott HR, McArdle CS. Albumin concentrations are primarily determined by the body cell mass and the systemic inflammatory response in cancer patients with weight loss. Nutr Cancer. 2001;39(2):210–213. doi:10.1207/S15327914nc392_8
9. Ray-Coquard I, Cropet C, Van Glabbeke M, et al. Lymphopenia as a prognostic factor for overall survival in advanced carcinomas, sarcomas, and lymphomas. Cancer Res. 2009;69(13):5383–5391. doi:10.1158/0008-5472.CAN-08-3845
10. Gay LJ, Felding-Habermann B. Contribution of platelets to tumour metastasis. Nat Rev Cancer. 2011;11(2):123–134. doi:10.1038/nrc3004
11. Asanuma K, Matsumine A, Nakamura T, et al. Impact of plasma fibrinogen levels in benign and malignant soft tissue tumors. Cancer Biomark. 2016;16(3):453–458. doi:10.3233/CBM-160584
12. Chan JY, Zhang Z, Chew W, et al. Biological significance and prognostic relevance of peripheral blood neutrophil-to-lymphocyte ratio in soft tissue sarcoma. Sci Rep. 2018;8(1):11959. doi:10.1038/s41598-018-30442-5
13. Ignacio de Ulíbarri J, González-Madroño A, de Villar NGP, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005;20(1):38–45.
14. Liang Y, Wang W, Li J, et al. Combined use of the neutrophil-lymphocyte and platelet-lymphocyte ratios as a prognostic predictor in patients with operable soft tissue sarcoma. J Cancer. 2018;9(12):2132–2139. doi:10.7150/jca.24871
15. Liang Y, Wang W, Que Y, et al. Prognostic value of the fibrinogen/albumin ratio (FAR) in patients with operable soft tissue sarcoma. BMC Cancer. 2018;18(1):942. doi:10.1186/s12885-018-4856-x
16. Que Y, Qiu H, Li Y, et al. Preoperative platelet-lymphocyte ratio is superior to neutrophil-lymphocyte ratio as a prognostic factor for soft-tissue sarcoma. BMC Cancer. 2015;15:648. doi:10.1186/s12885-015-1654-6
17. Liang Y, Hou T, Que Y, et al. Elevated controlling nutritional status (CONUT) score is associated with poor long-term survival in patients with low-grade soft-tissue sarcomas treated with surgical resection. Clin Orthop Relat Res. 2019;477(10):2287–2295. doi:10.1097/CORR.0000000000000767
18. Jo VY, Fletcher CDM. WHO classification of soft tissue tumours: an update based on the 2013 (4th) edition. Pathology. 2014;46(2):95–104. doi:10.1097/PAT.0000000000000050
19. Neuville A, Chibon F, Coindre J-M. Grading of soft tissue sarcomas: from histological to molecular assessment. Pathology. 2014;46(2):113–120. doi:10.1097/PAT.0000000000000048
20. Blanche P, Dartigues J-F, Jacqmin-Gadda H. Estimating and comparing time-dependent areas under receiver operating characteristic curves for censored event times with competing risks. Stat Med. 2013;32(30):5381–5397. doi:10.1002/sim.5958
21. Camp RL, Dolled-Filhart M, Rimm DL. X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res. 2004;10(21):7252–7259. doi:10.1158/1078-0432.CCR-04-0713
22. Gronchi A, Miceli R, Shurell E, et al. Outcome prediction in primary resected retroperitoneal soft tissue sarcoma: histology-specific overall survival and disease-free survival nomograms built on major sarcoma center data sets. J Clin Oncol. 2013;31(13):1649–1655. doi:10.1200/JCO.2012.44.3747
23. van Praag VM, Rueten-Budde AJ, Jeys LM, et al. A prediction model for treatment decisions in high-grade extremity soft-tissue sarcomas: personalised sarcoma care (PERSARC). Eur J Cancer. 2017;83:313–323. doi:10.1016/j.ejca.2017.06.032
24. Nakamura T, Matsumine A, Matsubara T, Asanuma K, Uchida A, Sudo A. The combined use of the neutrophil-lymphocyte ratio and C-reactive protein level as prognostic predictors in adult patients with soft tissue sarcoma. J Surg Oncol. 2013;108(7):481–485. doi:10.1002/jso.23424
25. Szkandera J, Absenger G, Liegl-Atzwanger B, et al. Elevated preoperative neutrophil/lymphocyte ratio is associated with poor prognosis in soft-tissue sarcoma patients. Br J Cancer. 2013;108(8):1677–1683. doi:10.1038/bjc.2013.135
26. Szkandera J, Gerger A, Liegl-Atzwanger B, et al. The lymphocyte/monocyte ratio predicts poor clinical outcome and improves the predictive accuracy in patients with soft tissue sarcomas. Int J Cancer. 2014;135(2):362–370. doi:10.1002/ijc.28677
27. Okuyama H, Ichikawa Y, Sun Y, Hamazaki T, Lands WEM. Cancer and all-cause mortalities are lower in the higher total cholesterol groups among general populations. World Rev Nutr Diet. 2007;96(1):37–54. doi:10.1159/000097806
28. Szkandera J, Pichler M, Liegl-Atzwanger B, et al. The elevated pre-operative plasma fibrinogen level is an independent negative prognostic factor for cancer-specific, disease-free and overall survival in soft-tissue sarcoma patients. J Surg Oncol. 2014;109(2):139–144. doi:10.1002/jso.23458
29. Callegaro D, Miceli R, Mariani L, Raut CP, Gronchi A. Soft tissue sarcoma nomograms and their incorporation into practice. Cancer. 2017;123(15):2802–2820. doi:10.1002/cncr.30721
30. Abaricia S, Van Tine BA. Management of localized extremity and retroperitoneal soft tissue sarcoma. Curr Probl Cancer. 2019;43(4):273–282. doi:10.1016/j.currproblcancer.2019.06.002
31. Gamboa AC, Gronchi A, Cardona K. Soft-tissue sarcoma in adults: an update on the current state of histiotype-specific management in an era of personalized medicine. CA Cancer J Clin. 2020;70(3):200–229. doi:10.3322/caac.21605
32. Singer S, Antonescu CR, Riedel E, Brennan MF. Histologic subtype and margin of resection predict pattern of recurrence and survival for retroperitoneal liposarcoma. Ann Surg. 2003;238(3):358–370. doi:10.1097/01.sla.0000086542.11899.38
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.